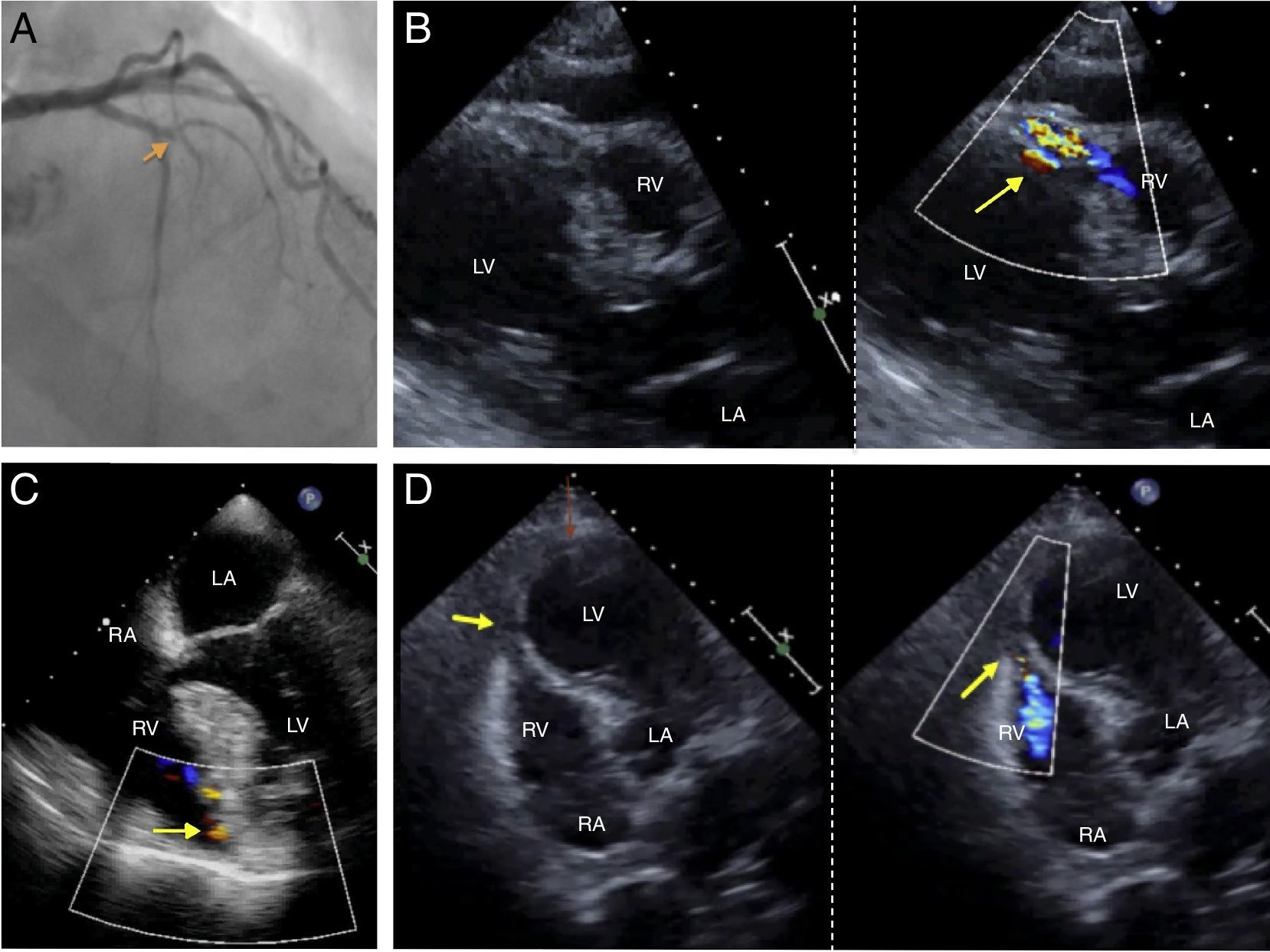
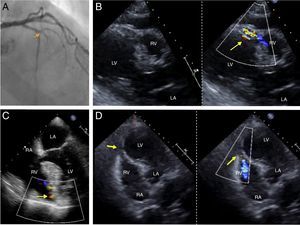
A 82 year-old man presented with an anterior acute ST-elevation myocardial infarction. An emergent coronariography showed a thrombotic occlusion of the proximal segment of the anterior descending coronary artery (Fig. 1A, Video 1), therefore a primary percutaneous coronary intervention (PCI) with a bare metal stent implantation was performed. In the first 24hours, a new pansystolic murmur was detected. A transthoracic and a transesophageal echocardiogram showed an apical interventricular communication with a left-to-right shunt (Fig. 1B, C, Video 2 and 3). An intra aortic balloon pump (IABP) was placed and emergent surgical repair with closure of the defect with a Dacron patch was carried out. Twelve hours after surgery, the patient presented hemodynamic deterioration and a new systolic murmur appeared. The echocardiogram confirmed the recurrence of a significant interventricular communication (Fig. 1D, Video 4). Unfortunately, despite agressive medical treatment, the patient perished.
In the era of primary PCI, mechanical complications after acute myocardial infarction such as post infarction ventricular septal rupture (VSR) are extremely rare, with an incidence less than 0.5%. Nevertheless, current mortality remains high and a prompt diagnosis and treatment are imperative to increase survival. Risk factors include age, female gender, hypertension, first MI, and poor coronary artery collateralization. Despite early surgical repair, recurrence and subsequent mortality represent a threat in these patients. The strategy of surgery following stabilization for around 6 weeks, often with IABP counterpulsation, is an attractive option in VSR, as it allows an infarcted septum to “mature” with fibrotic healing. However, in some patients who are at high risk of perioperative death but in whom surgery cannot be safely deferred, the use of mechanical circulatory support, such as Veno-arterial extracorporeal membrane oxigenation (VA-ECMO) and other temporary circulatory support devices allows for peri-operative support of these patients and potentially for patient optimization, surgery at a delayed stage, and may result in improved survival. The role of percutaneous devices to primarily close defects following VSR is limited at present to selected patients with simple defects that are less than 15mm in diameter and after approximately 3 weeks following AMI, although percutaneous closure has also been used in the acute setting, with variable results.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflict of interestThe authors declare no conflict of interest.