Ruptured mycotic aneurysm following infective endocarditis is rare, but remains a life-threatening condition. We report a case of surgical management of a ruptured mycotic aneurysm of the common femoral artery, complicating mitral valve endocarditis with heart failure in a twenty-nine-year-old female who underwent a prosthetic mitral valve replacement and an in situ successful reconstruction using reversed saphenous vein graft. The patient recovered uneventfully and was found in good condition as a three-year follow-up.
El aneurisma micótico roto después de una endocarditis infecciosa es raro, pero sigue siendo una afección potencialmente mortal. Presentamos el caso de manejo quirúrgico de un aneurisma micótico roto de la arteria femoral común, que complica la endocarditis de la válvula mitral con insuficiencia cardíaca en una mujer de 29 años, a la que se le realizó un reemplazo valvular mitral y una reconstrucción exitosa in situ, utilizando injerto de vena safena. El paciente se recuperó sin incidentes y se encontró en buenas condiciones a los tres años de seguimiento.
The development of peripheral mycotic aneurysms and subsequent rupture was a common occurrence in the preantibiotic era. The first complete description of mycotic aneurysm was presented in 1885 by Sir William Osler, in a 30-year-old man with four aneurysms of the aortic arch, arising as a complication of endocarditis. It is a serious, clinical condition with significant morbidity and mortality rates. Mycotic aneurysms of the femoral artery are a rarity, accounting for merely 0.8% of all aneurysms. We report a case of surgical management of a ruptured mycotic aneurysm complicating mitral valve endocarditis.
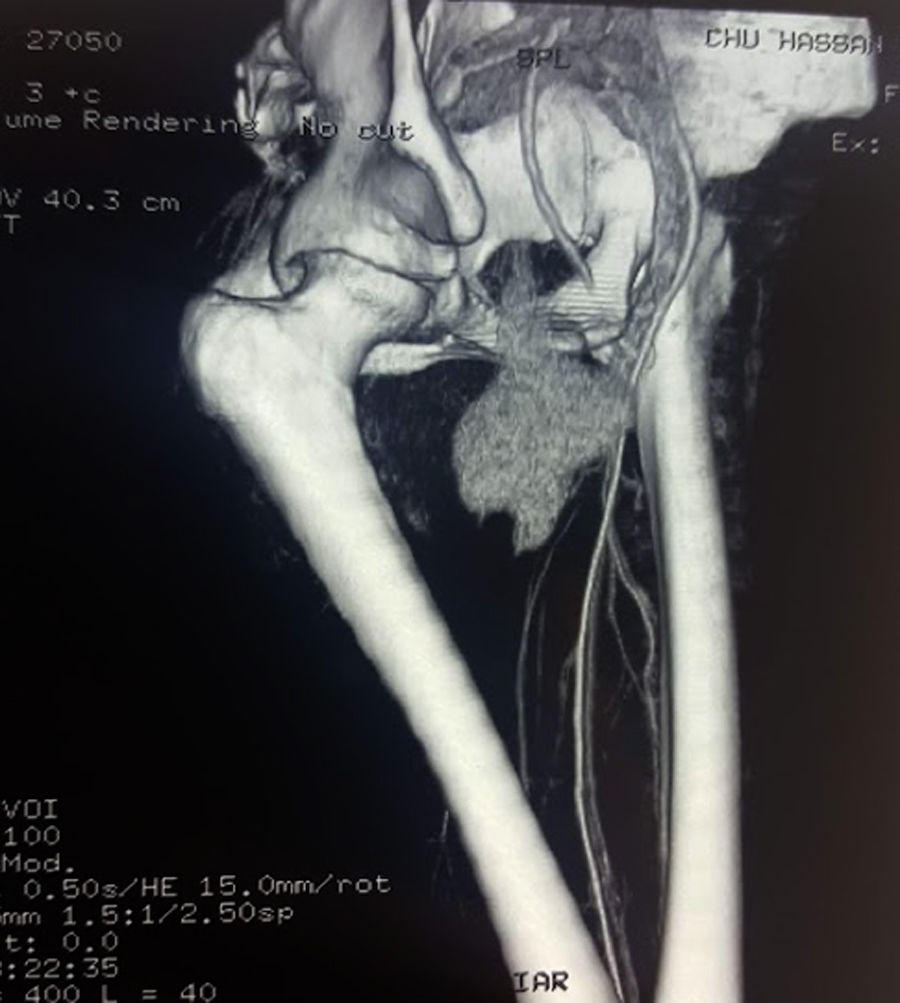
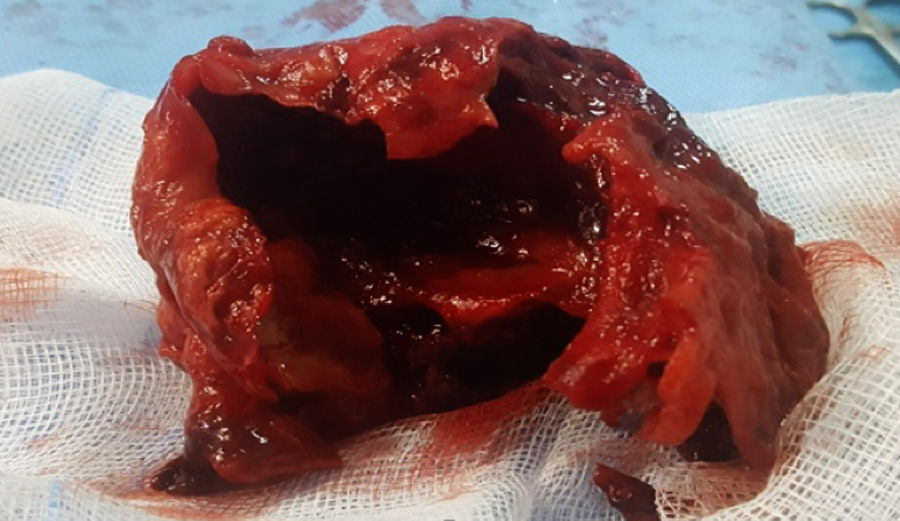
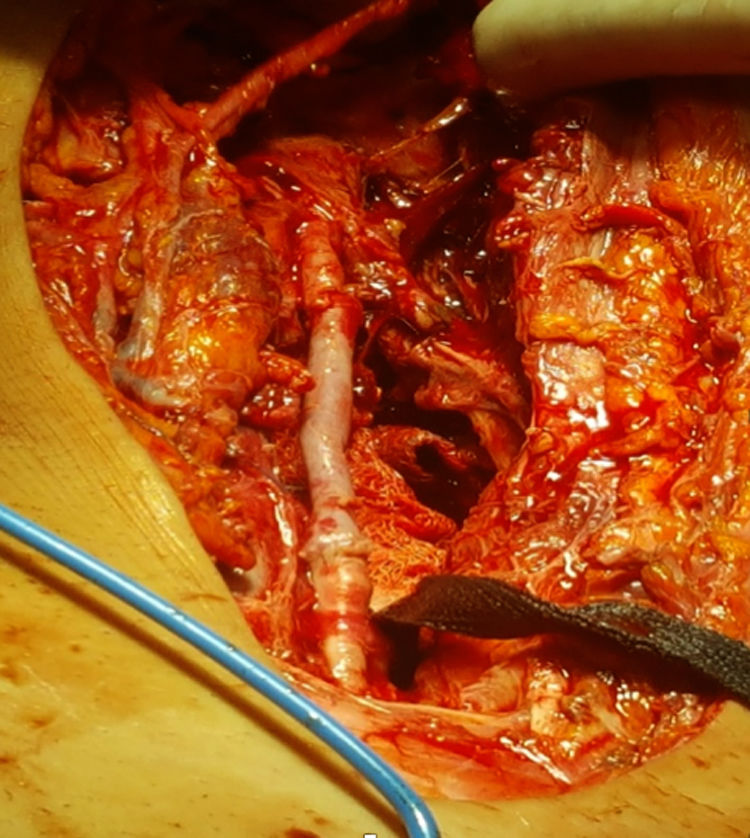
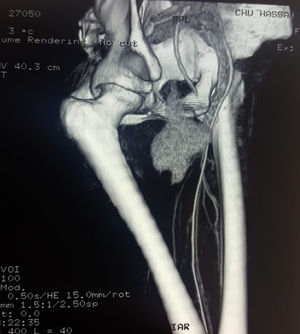
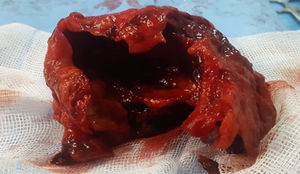
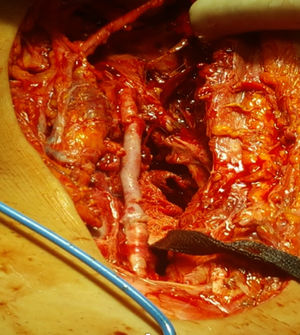
Case reportA 29 years old lady, with known rheumatic disease, previously diagnosed to have mitral valve prolapse, was admitted to the emergency department with a two-months history of fever, night sweats, increasing breathlessness, and weight loss over three months. The patient also reported a pulsatile, painful swelling in the right thigh. On examination her temperature was 39°C, heart rate 110beats/min and blood pressure 102/60mmHg. Auscultation of her chest revealed bibasilar crepitations and a 4/6 pan-systolic murmur was heard best at the apex radiating to the axilla. There was also a large pulsating mass in the anteromedial right thigh. Blood tests showed anemia (hemoglobin 10g/dl), mild neutrophil leukocytosis (white cell count 12.5109/L), and raised C-reactive protein (178mg/L) with normal electrolytes, blood cultures were found positive for Staphylococcus Hominis. Transthoracic echocardiography revealed a bright echogenic mobile mass on the mitral valve measuring 21mm on the atrial side of the anterior mitral valve, several other small vegetations were evident on the posterior mitral valve with severe mitral regurgitation and elevated pulmonary artery systolic pressure. Color doppler ultrasound was performed and showed a thrombosed aneurysm of the common femoral artery. Appropriate intravenous antibiotic therapy was initiated and given the severity of endocarditis and cardiac failure, the patient underwent first an emergency prosthetic mitral valve replacement with a 31-mm SJM valve under standard cardiopulmonary bypass. The postoperative course was uneventful, the fevers remitted, but the white blood cell/C-reactive protein (WBC/CRP) count elevated, with a continuous complaint of right thigh pain and numbness. On the 4th day after MVR, the patient experienced acute pain and a marked increase in the thigh swelling (Fig. 1), contrast-enhanced CT scan showed acute expansion of the common femoral aneurysm with evidence for contained rupture (Fig. 2). Under general anesthesia, the patient underwent an emergency exploratory surgery of the right lower limb. There was a large-volume hematoma related to the ruptured aneurysm of the common femoral artery (Fig. 3). The aneurysm was resected and the vascular segment reconstructed by reversed interposition of a segment of the ipsilateral saphenous vein (Fig. 4). The post-operative course was uneventful and other laboratory data immediately normalized. Microbiology tests on the aneurysm sac were negative with no germ growth on culture. On histopathology, the artery wall was disrupted and replaced by fibrin and thrombus. The patient progressed well and was discharged on the fifth postoperative day. There was no recurrence of infection, and the graft remains patent.
Despite improvement in treatment of infective endocarditis (IE), the complications are frequently seen. The complications of IE consist of neurological vascular complications (45.5%) and peripheral vascular complications (myocardial infarction, pulmonary embolism, splenic infarction, acute limb ischemia, gangrene) that are mainly the consequence of emboli from valve vegetations, which are life threatening and debilitating. However, 20% of embolisms are asymptomatic.1 Mycotic aneurysms (MA) are rarely seen and defined as localized, irreversible vascular dilatations caused by weakening and destruction of the vessel wall by an invasive organism establishing an infective arteritis. In 1885, Sir William Osler described the first infected aneurysm of the aorta complicating bacterial endocarditis.2 The term ‘mycotic’ derives from the mushroom-like appearance of the aneurysms originally described, and not their underlying microbiological etiology.2 Endarterial infection may arise through hematogenous seeding from distant septic foci either direct to the arterial intima or to deeper mural layers via the vasa vasorum. Currently, the incidence of these aneurysms following an episode of endocarditis is quite rare, and their location is dependent upon the peripheral lodgment site of mycotic emboli. Peripheral embolic events usually involve the lower extremities with most emboli lodging at the common femoral artery bifurcation followed by the abdominal and thoracic aorta. MA of intracranial vessels are uncommon and visceral arteries are extremely rare.3 Fever, painful pulsatile mass with palpable thrill and local inflammatory changes are the most clinical findings of physical examination.4,5 The most frequently involved bacteria are Staphylococcus, Streptococcus, Pneumococcus and Pseudomonas aeruginosa however negative hemocultures are seen relatively high (25%). Transthoracic and transesophageal echocardiography are used for the prediction of embolisms. The size and mobility of vegetations are predictive factors of embolisms.1 In the literature, the most often reported MA diagnostic tool is angiography.6 Computed tomographic angiography is an accurate and effective diagnostic method for tracking size, configuration, and extravasation of blood into the soft tissue of the thigh. Ultrasound is considered a better test to precisely determine aneurysm diameter.7 MRI can be of diagnostic utility or of discriminatory value when other tests are inconclusive.8 The natural history of untreated mycotic aneurysms is of fatality from either massive hemorrhage or fulminant sepsis.9 Manifestations of aneurysm expansion correlate with anatomical location. Although occurring as late as complications in terms of the natural history, up to 45% rupture, with fistula formation in 18%.9 Management of MA is less clear because of paucity of cases reported in the literature, in general, the standard therapy includes early antibiotic use, which should be based on appropriate guidelines, valve surgery and/or complete excision of infective tissues. Surgical treatment of MA is directed to control hemorrhage. Debridement of all infected tissue and restoration of circulation is the subsequent aim. Hemorrhage can be controlled by clamping the vessel proximally and distally. Debridement should include evacuation of infected hematoma and excision of all necrotic tissues, which usually includes the arterial wall itself. Restoration of circulation in such cases is typically achieved with bypass grafting using autogenous vein. Endovascular options such as coil embolization/thrombin glue injection, stenting appear attractive alternatives to surgery.10 We did not consider them in our case, as the patient had signs of compartmental compression due to the large thigh hematoma. Additionally, the evidence of such interventions in mycotic aneurysms is limited.
ConclusionMycotic aneurysms are a serious clinical condition that are associated with significant morbidity and mortality. They may be prevented with an early and appropriate management of IE but once diagnosed they should be treated surgically. Even if Antibiotics may control sepsis, they do not reduce risk of rupture of the weakened vessel wall.
Informed consentVerbal and written informed consent were obtained from the patient for the publication of this case report.
Conflicts of interestsThe authors declare that there is no conflict of interest regarding the publication of this paper.