Sudden natural deaths, particularly those resulting from cardiovascular causes such as cardiac tamponade and aortic dissection, present significant challenges in forensic medicine and public health.
MethodsThis study prospectively analyzes six cases of sudden death due to ruptured dissecting aorta, identified through postmortem examinations conducted in 2023. Cases included all individuals who exhibited sudden collapse and death within 24h of symptom onset.
ResultsAn unusually frequent incidence of cardiac tamponade was observed during autopsies conducted in 2023, with the rupture of a dissecting aorta being the most frequent cause and found in six cases. Notably, rupture at the origin of the aorta was the most common finding, accounting for 90% of cases in our study. The affected individuals ranged in age from 35 to 55 years, and all succumbed to their symptoms within 24h of onset.
ConclusionsEfforts to enhance diagnostic capabilities, raise awareness among healthcare professionals, and implement preventive strategies are crucial for mitigating the burden of sudden cardiovascular deaths. Collaborative approaches involving forensic practitioners, clinicians, and researchers are essential for understanding the underlying mechanisms of sudden natural deaths and implementing evidence-based interventions to prevent future fatalities.
Las muertes naturales súbitas, en particular las que resultan de causas cardiovasculares como el taponamiento cardíaco y la disección aórtica, presentan desafíos importantes en la medicina forense y la salud pública.
MétodosEste estudio analiza prospectivamente 6 casos de muerte súbita debido a la rotura de la aorta disecante, identificados a través de exámenes post mortem realizados en 2023. Los casos incluyeron a todos los individuos que presentaron colapso repentino y muerte dentro de las 24h posteriores al inicio de los síntomas.
ResultadosSe observó una incidencia inusualmente frecuente de taponamiento cardíaco durante las autopsias realizadas en 2023, siendo la rotura de una aorta disecante la causa más frecuente, y encontrada en 6 casos. En particular, la rotura en el origen de la aorta fue el hallazgo más común, representando el 90% de los casos en nuestro estudio. Los individuos afectados tenían entre 35 y 55 años de edad, y todos sucumbieron a sus síntomas dentro de las 24h posteriores al inicio.
ConclusionesLos esfuerzos para mejorar las capacidades de diagnóstico, generar conciencia entre los profesionales de la salud e implementar estrategias preventivas son cruciales para mitigar la carga de muertes súbitas cardiovasculares. Los enfoques colaborativos que involucran a médicos forenses, médicos clínicos e investigadores son esenciales para comprender los mecanismos subyacentes de las muertes súbitas naturales e implementar intervenciones basadas en la evidencia para prevenir futuras muertes.
Sudden or unexpected fatal events occurring within 1h of the onset of symptoms in apparently healthy individuals, or in those with existing diseases not severe enough to account for such an abrupt outcome, are classified as natural deaths. Some definitions extend to cases where individuals, not previously known to be suffering from any serious illness, injury, or poisoning, are found dead or die within 24h of the onset of a terminal illness.1 Sudden deaths are more common among older individuals and typically occur under circumstances that do not raise immediate suspicion. However, sudden death of younger individuals almost always triggers suspicion and warrants further investigation.
Sudden natural deaths represent 10–20% of all cases that undergo autopsy in India. Among these, cardiac causes are responsible for 50–60% of sudden natural deaths. However, deaths due to cardiac tamponade are relatively rare, accounting for only 1–2% of cardiovascular-related deaths. Cardiac tamponade is a life-threatening condition characterized by a rapid increase in pericardial pressure, resulting from the accumulation of blood, pus, other fluids, or gas in the pericardial cavity. This accumulation impedes ventricular filling, cardiac output, and hemodynamic stability. Normally, the pericardial cavity contains 20–50ml of fluid, but the sudden accumulation of 350–400ml of blood or fluid can lead to abrupt cardiac arrest and death.2–5 Common causes of cardiac tamponade include chest trauma, intra-pericardial rupture of major blood vessels, complications following acute myocardial infarction, malignancies, dissecting aortic aneurysms, and surgical trauma during both open and closed procedures.4–8 Additionally, chronic myocardial rupture, which may have been present for an extended period, can evolve into an pseudoaneurysm, leading to sudden death.3,9,10
Acute aortic syndrome is a critical medical condition that encompasses a spectrum of life-threatening aortic diseases, including acute aortic dissection, intramural hematoma, and penetrating aortic ulcer. These conditions share a common underlying pathology involving a tear or rupture in the aortic wall.8,11 Aortic dissection, although less common, is a life-threatening condition that, if not promptly diagnosed, can lead to death owing to complications such as cardiac tamponade, aortic regurgitation, or acute myocardial infarction.4,5,8,12,13 Timely diagnosis and appropriate intervention are imperative to manage such cases. In 2023, a significant number of individuals in India experienced sudden collapses and fatalities during their daily activities, often without prior major illnesses or symptoms. The sudden increase in cardiovascular cases underscores the urgent need for further research and effective solutions. Each year, many individuals die undiagnosed, imposing a burden on the economy and causing financial hardships for families. It is crucial to evaluate the various factors contributing to the natural causes of cardiac tamponade, such as aortic dissection rupture, through further studies to reduce the fatality rate associated with this condition.
In forensic practice, cardiovascular causes are frequently implicated in cases of sudden natural death. Given the abrupt onset and rapid deterioration associated with cardiac tamponade, diagnosis often occurs during autopsy procedures.3,14 In the present study, we examined six cases of sudden death and, upon detailed history and postmortem examination, identified aortic dissection with rupture at various sites as the underlying cause.
MethodsThis cross sectional observational study prospectively analyzes six cases of sudden death due to ruptured dissecting aorta, identified through postmortem examinations conducted in 2023. Cases were included all individuals who exhibited sudden collapse and death within 24h of symptom onset. Detailed postmortem examinations, including external and internal evaluations, were performed to identify the underlying cause of death. Data regarding clinical history, symptoms, and autopsy findings were collected and analyzed.
Ethical consideration: Ethical approval and the need for informed consent were waived for this study as it utilized deidentified data and autopsy specimens. Institutional review board (IRB) approval was not required due to the use of existing deidentified data. All patient data used in this study were anonymized to protect patient privacy and confidentiality.
ResultsCompared to the observation of the previous five years, out of 141 sudden natural death cases in 2023, an unusually high incidence of cardiac tamponade was observed during autopsies, with the rupture of a dissecting aorta being the most frequent cause, identified in six cases. Notably, rupture at the origin of the aorta was the most common finding, accounting for 90% of cases in our study. The affected individuals ranged in age from 35 to 55 years, and all succumbed to their symptoms within 24h of onset. Below, we provide a brief description of the circumstances surrounding each death event, followed by the postmortem findings in the six cases.
Case 1A 55-year-old male presented to the casualty with complaints of chest pain, accompanied by feelings of unease and tightness in the chest. The patient collapsed during the examination and was declared dead. There was no history of hypertension or diabetes. A provisional diagnosis of poisoning was suspected at the casualty.
Postmortem findingsExternal examinationFace congested; white froth present at the mouth and bluish discoloration of the nails. The deceased weighed approximately 74kg and had a height of 179cm.
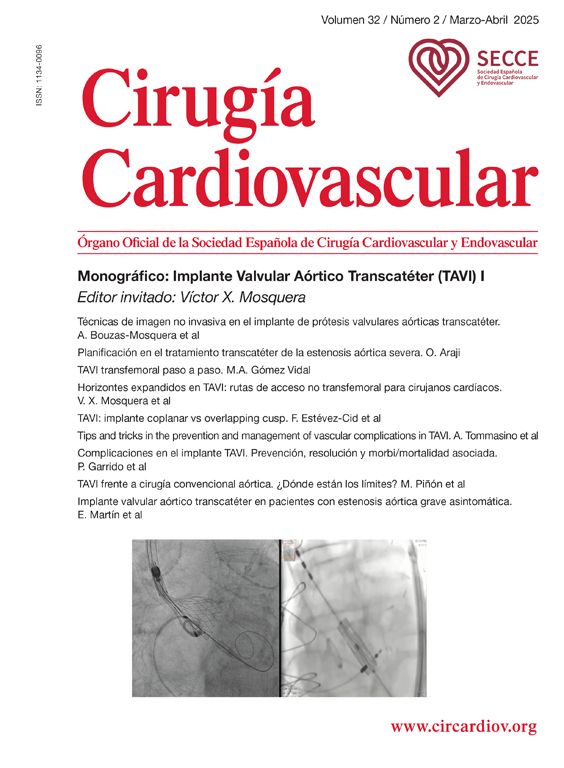
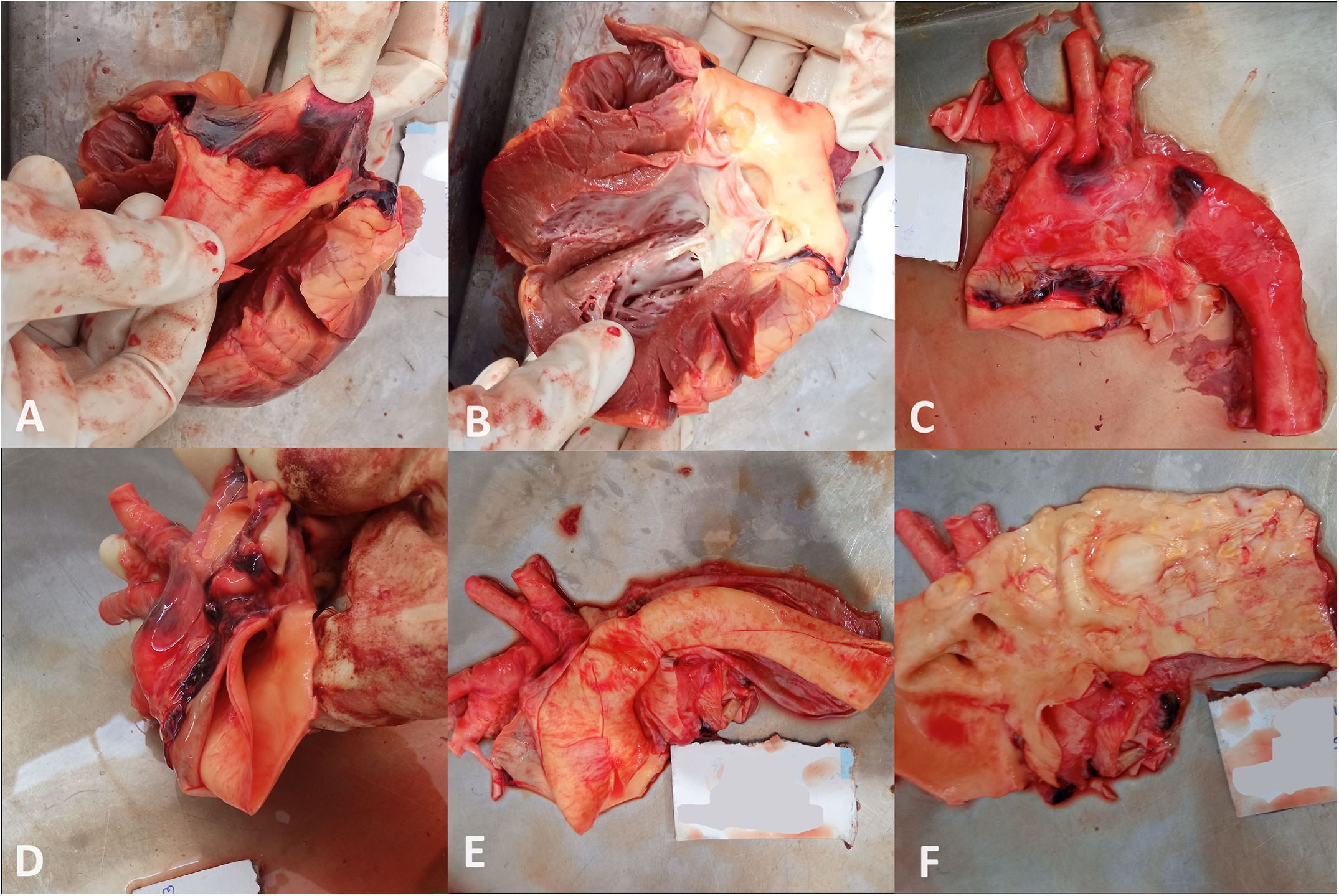
Internal examinationFluid and clotted blood of 580ml was present in the pericardial cavity. Upon careful dissection, a rupture of the ascending aorta was observed (Figs. 1A and 2B). The aorta showed a thick deposition of atheromatous patches up to the descending aorta (Fig. 1C).
Stanford classification: Type A
De Bakey classification: Type I
Case 2A 44-year-old male presented to the casualty with complaints of chest pain and feelings of unease after his evening meal. Despite rigorous treatment, the patient succumbed within a few minutes. He had a history of hypertension but no other chronic illnesses.
Postmortem findingsExternal examinationNo specific observations were made. The deceased weighed approximately 60kg and had a height of 168cm.
Internal examinationApproximately 400ml of fluid and clotted blood was found in the pericardial cavity (Fig. 2A, B). Rupture of the ascending aorta was noted, along with dilatation near the coronary ostia and deposition of atheromatous patches (Fig. 2C, D).
Stanford classification: Type A
De Bakey classification: Type II
Case 3A 38-year-old male was brought to the hospital deceased, with a history of chest pain and uneasiness. He suddenly collapsed at home and died. There was no history of diabetes, hypertension, or chronic illness. The deceased weighed approximately 67kg and had a height of 172cm.
Postmortem findingsExternal examinationFacial congestion and whitish froth at the mouth with no atypical smell.
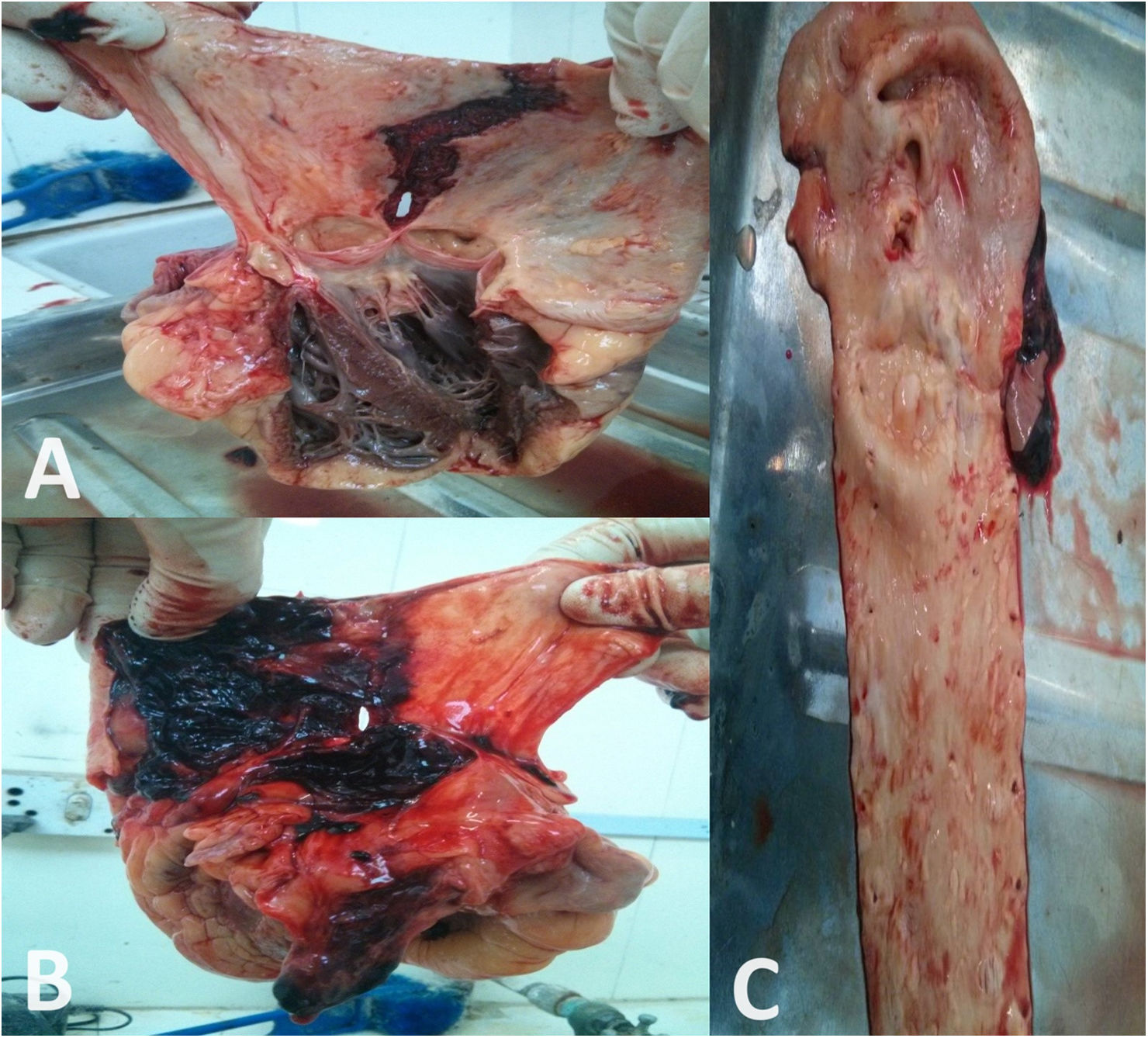
Internal examinationThe collection of fluid and clotted blood of 540ml were observed in the pericardial cavity (Fig. 3A, B). There was a transverse rupture of the ascending aorta and double-lumen appearance of the descending aorta (Fig. 3C, D).
Stanford classification: Type A
De Bakey classification: Type I
Case 4A 49-year-old female experienced sudden convulsions at home, followed by unconsciousness. She was transferred to a nearby private hospital, where she was pronounced dead upon arrival by the attending medical officer. She had a history of cerebrovascular stroke one year prior, with no history of diabetes or hypertension. The patient fully recovered and was on regular medication.
Postmortem findingsExternal examinationFacial congestion, reddish froth at the nostrils and mouth, and bluish discoloration of the nails and lips. The deceased weighed approximately 51kg and had a height of 146cm.
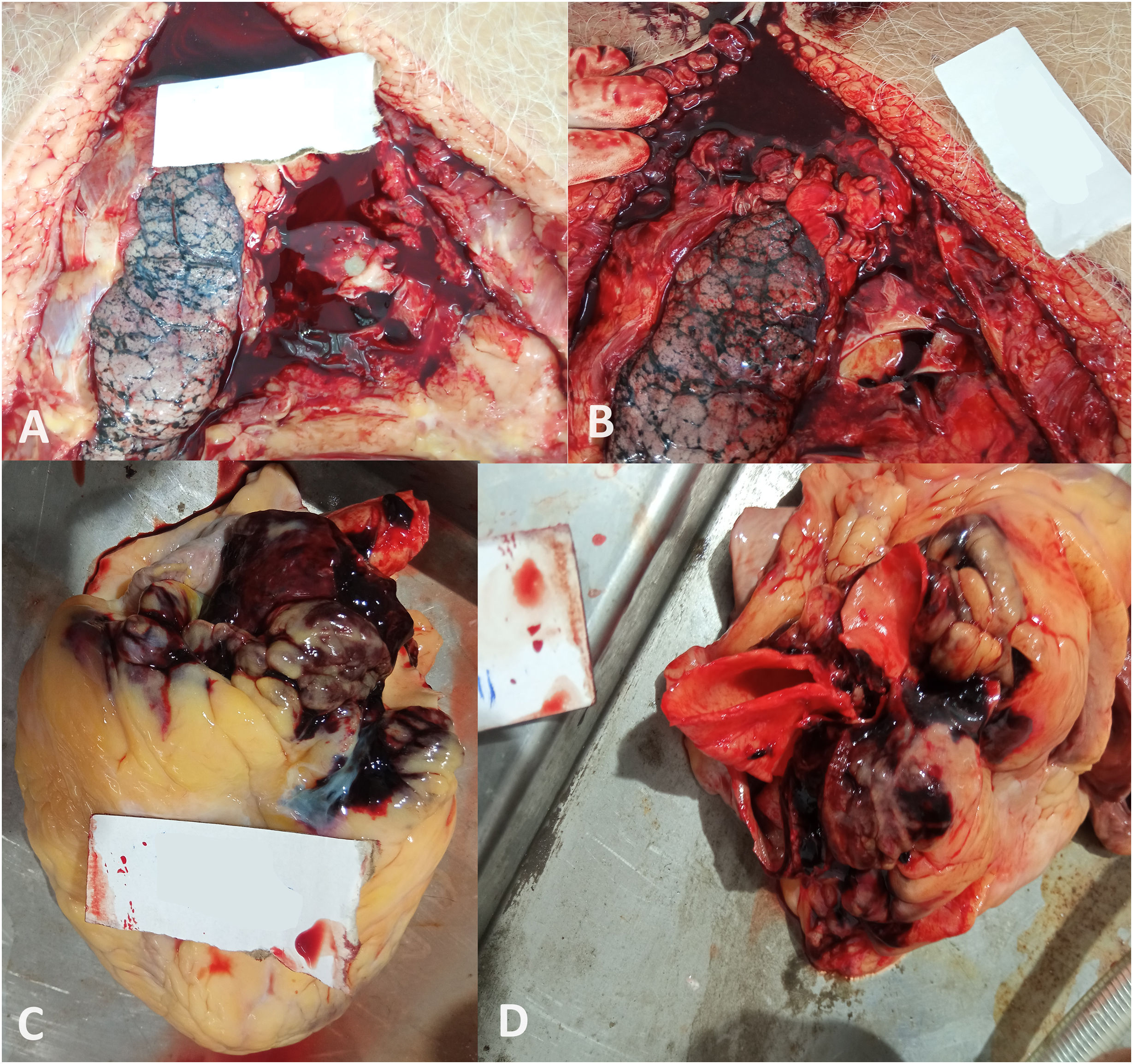
Internal examinationThe pericardial cavity contained 380ml of fluid and clotted blood. The ascending, arch, and descending aorta exhibited wall splitting into two layers, creating false canalization with atheromatous plaques present at various locations (Fig. 4C–F). There was rupture of the aortic wall near the origin of the right coronary artery, with extravasation of blood into the surrounding tissue (Fig. 4A, B). The aortic wall was soft and thinned out. Both coronaries showed thickening and calcification with atheromatous patches observed at some sites.
Stanford classification: Type A
De Bakey classification: Type I
Case 5A 51-year-old male had been experiencing chest pain for the past two days but did not take any medication. He suddenly lost consciousness and was transferred to a nearby hospital, where he was pronounced dead on arrival.
Postmortem findingsExternal examinationFacial congestion and bluish discoloration of the nails. The deceased weighed approximately 114kg and had a height of 170cm.
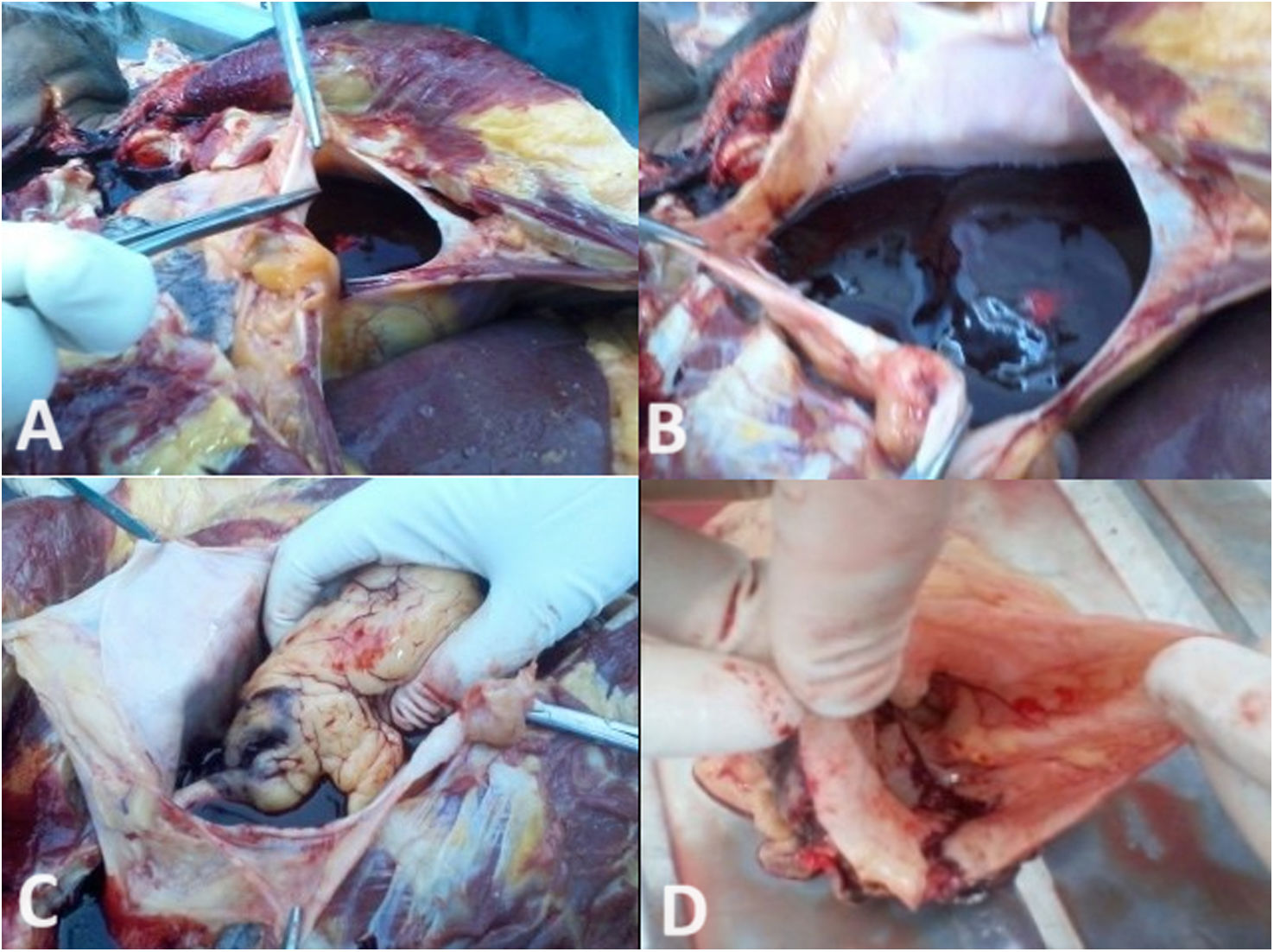
Internal examinationThe pericardial cavity contained 300ml of clotted blood and fluid (Fig. 5A, B). The ascending aorta and arch of the aorta up to the common carotid exhibited wall splitting into two layers, forming false canalization with atheromatous plaques present at various sites (Fig. 5D). There was a rupture of the outer wall of the aorta near the origin of the ascending aorta, with extravasation of blood present in the surrounding tissues (Fig. 5C).
Stanford classification: Type A
De Bakey classification: Type I
Case 6A 35-year-old male had been experiencing fever and vomiting for the past two days. Suddenly, the patient developed breathlessness and lost consciousness at home. He was rushed to a nearby hospital, where he was pronounced dead upon arrival.
Postmortem findingsExternal examinationFacial congestion with reddish froth at the nostrils. The deceased weighed approximately 69kg and had a height of 178cm.
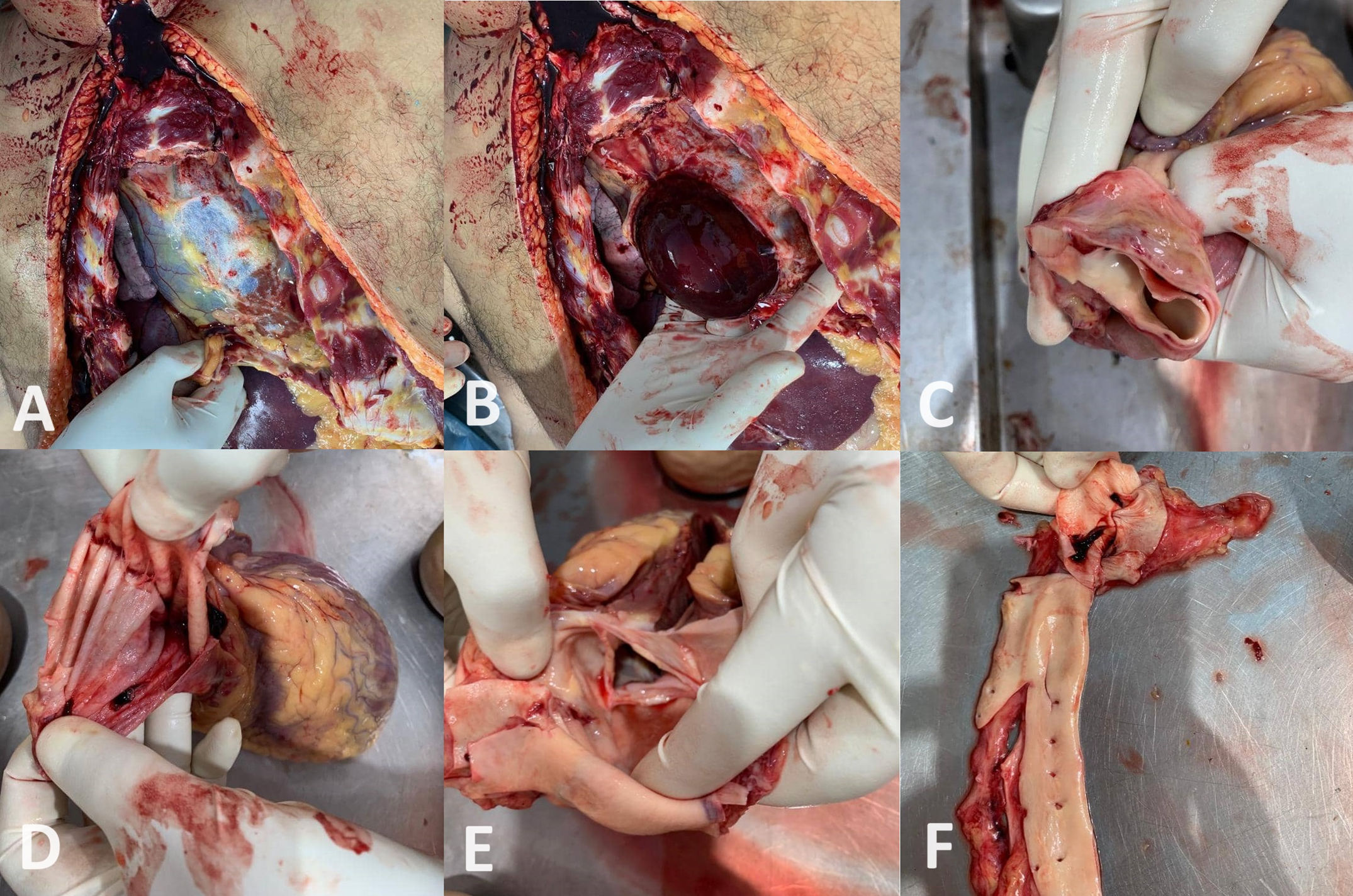
Internal examinationThe pericardial cavity contained 440ml of clotted blood and fluid (Fig. 6A, B). The ascending and arch of the aorta exhibited dissection and dilation, with rupture near the origin of the ascending aorta (Fig. 6C–6F).
Stanford classification: Type A
De Bakey classification: Type I
DiscussionSudden deaths among young and middle-aged adults, typically between the ages of 20 and 59, have become increasingly common. The prevalence of these occurrences underscores the importance of conducting detailed histories and thorough investigations to identify underlying conditions that may go unnoticed. Timely diagnosis and appropriate management are crucial to save the lives of young individuals affected by these conditions.
Aortic dissection is the most prevalent catastrophe affecting the aorta, occurring to 2–3 times more frequently in the thoracic region than in the abdominal aorta. Without treatment, approximately 33% of patients succumbed within the first 24h and 50% within 48h. The aortic wall comprises collagen, elastin, and smooth muscle cells in the intima, media, and adventitia. Degenerative changes associated with aging can lead to tissue breakdown, resulting in cystic medial necrosis and an increase in basophilic ground substances. Any condition that compromises the strength of the aortic wall can predispose an individual to aortic dissection. Shearing forces cause the layers of the media to separate, with intimal rupture typically occurring at points of fixation where hydraulic pressure is the greatest. The ascending aorta's initial few centimeters (90%) are the most common sites of rupture, followed by those just distal to the left subclavian artery.
The De Bakey classification divides dissections into three types11,15:
Type I – is ascending aorta, aortic arch, and descending aorta.
Type II – is confined to the ascending aorta.
Type III – is confined to the descending aorta distal to the left subclavian artery.
Type IIIa – dissections that originate distal to the left subclavian artery.
Type IIIb – originate distal to left subclavian artery may extend below diaphragm.
Stanford classification divides dissections into two types11,15:
Type A involves the ascending aorta (De Bakey types I and II)
Type B does not (De Bakey type III).
These classifications have significant clinical implications for treatment. Type A dissections typically require surgical intervention, given their involvement of the ascending aorta and associated complications. In contrast, Type B dissections are generally managed medically, focusing on blood pressure control to prevent progression.
In forensic practice, cardiovascular causes are frequently observed in cases of sudden natural deaths. The onset of cardiac tamponade is rapid and leads to rapid deterioration, often resulting in death within a short period, and is frequently identified during postmortem examinations.3 In this study, cardiac tamponade was observed at 4.25% during autopsies conducted in 2023. The most common cause was rupture of a dissecting aorta, with rupture at the aortic origin being the predominant finding (90%) in our observations. In this study, all six cases (100%) were classified as Type A according to the Stanford classification. Based on the DeBakey classification, five cases (83%) were identified as Type I, and one case (17%) as Type II. The affected individuals were typically between 35 and 55 years of age. In 66% (4/6) of the cases, chest pain was the primary symptom, while 16.5% (1/6) experienced seizures, and another 16.5% (1/6) presented with vomiting and fever. All individuals succumbed to their symptoms within 24h of onset. Aortic dissection, although less common, is a life-threatening condition that, if not promptly diagnosed, can lead to fatal complications, such as cardiac tamponade, aortic regurgitation, or acute myocardial infarction.7 Timely diagnosis and appropriate intervention are crucial in these cases. The sudden rise in cardiovascular cases observed in 2023, with individuals collapsing and dying during routine activities without prior major illnesses or symptoms, underscores the need for further research and targeted solutions. Undiagnosed deaths that occur annually impose a significant burden on the economy and result in financial losses for affected families. It is imperative to evaluate various factors contributing to the natural causes of cardiac tamponade, such as rupture of the aortic dissection, through extensive studies aimed at reducing the fatality rate associated with this condition.
ConclusionSudden natural deaths, particularly those related to cardiovascular causes such as cardiac tamponade and aortic dissection, pose significant challenges in forensic medicine and public health. Our study highlights an alarming increase in the incidence of cardiac tamponade, primarily attributed to the rupture of a dissecting aorta, observed during autopsies conducted in 2023. The predominance of cases involving the rupture of the aortic origin underscores the importance of identifying and addressing risk factors associated with aortic dissection. Efforts to improve diagnostic capabilities and raise awareness among healthcare professionals regarding the presentation and management of aortic dissection are essential for timely intervention and improved patient outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Ethics approval and consent to participateEthical approval and the need for informed consent were waived for this study as it utilized deidentified data and autopsy specimens. Institutional review board (IRB) approval was not required due to the use of existing deidentified data. All patient data used in this study were anonymized to protect patient privacy and confidentiality.
Conflict of interestThe authors declare that they have no conflict of interest.