Patients with acute type A aortic dissection often present with malperfusion, which occurs when the dissection flap compromises blood flow through an aortic branch vessel. In prior study, between 20.5% and 33.6% of patients with acute type A aortic dissection had preoperative malperfusion, which was identified as a significant predictor of early mortality after surgery.1–3 In 2009, our group developed a grading system for preoperative malperfusion known as the Penn classification4 which has become a commonly utilized tool to determine the impact of malperfusion on surgical outcomes.
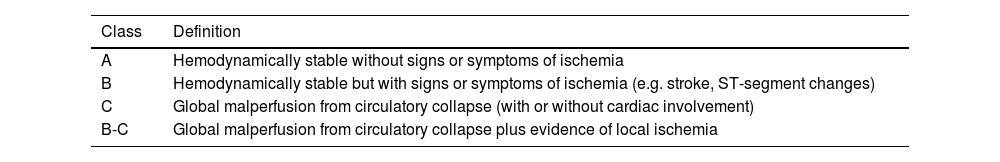
The Penn classification categorizes patients by the extent of malperfusion affecting the body—none, local, global, or a combination of local and global (Table 1). Importantly, this system is based on malperfusion syndrome, or the constellation of signs and symptoms of organ ischemia that results from branch vessel occlusion, rather than radiographic evidence of malperfusion alone.
Penn classification for Type A aortic dissection.
| Class | Definition |
|---|---|
| A | Hemodynamically stable without signs or symptoms of ischemia |
| B | Hemodynamically stable but with signs or symptoms of ischemia (e.g. stroke, ST-segment changes) |
| C | Global malperfusion from circulatory collapse (with or without cardiac involvement) |
| B-C | Global malperfusion from circulatory collapse plus evidence of local ischemia |
The Penn class was initially created using data from 221 patients who underwent surgical repair for acute type A aortic dissection between 1993 and 2004 at our center.4 More recently, this system has been validated on an expanded cohort of 1192 patients who underwent surgery at our institution over a span of 27 years, from 1993 to 2020.5 This study demonstrated that the Penn classification was a strong predictor of 30-day mortality with values of 5.2%, 10.3%, 15.2% and 35.3% for Penn Class A, B, C and B-C, respectively. After adjustment, the odds of 30-day mortality increased significantly with class B (odds ratio [OR], 2.43; 95% CI, 1.38–4.27), class C (OR, 3.39; 95% CI, 1.90–6.03), and class B-C (OR, 13.08; 95% CI, 7.90–22.15) compared with class A.5 These findings have been confirmed by others in the United States,6 Europe7,8 and Asia.9
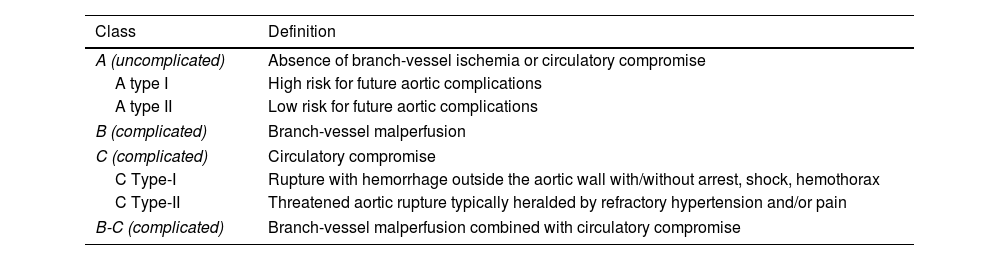
This classification has been also applied and adapted in type B dissections (Table 2),5 which essentially share with their type A cousin the possibility of presenting different types of malperfusion, making emergent surgical management necessary in these cases. In its adjusted form, uncomplicated presentations are subdivided into subcategories I or II (Table 2), based on the risk of progression to future aortic complications (aneurysm progression, rupture), with regards mostly to the morphology of the false lumen.10
Penn classification for Type B aortic dissection.
| Class | Definition |
|---|---|
| A (uncomplicated) | Absence of branch-vessel ischemia or circulatory compromise |
| A type I | High risk for future aortic complications |
| A type II | Low risk for future aortic complications |
| B (complicated) | Branch-vessel malperfusion |
| C (complicated) | Circulatory compromise |
| C Type-I | Rupture with hemorrhage outside the aortic wall with/without arrest, shock, hemothorax |
| C Type-II | Threatened aortic rupture typically heralded by refractory hypertension and/or pain |
| B-C (complicated) | Branch-vessel malperfusion combined with circulatory compromise |
Over the years, a few new classification systems and risk estimation models have been introduced. Sievers et al. proposed a well-designed system addressing the Type of dissection according to Stanford classification, location of the primary Entry tear, and malperfusion with its location (TEM).11 Although it addresses localization of malperfusion and discriminates whether it is clinical or only radiographic, it does not account for hemodynamic instability (global malperfusion). The GERAADA score, a recently introduced and validated risk calculator for 30-day mortality derived from the German Registry of Acute Aortic Dissection Type A, incorporates an extensive range of preoperative characteristics, encompassing both local and global malperfusion.12 Due to its complexity, which includes the evaluation of 11 parameters encompassing clinical, echocardiographic, and radiological factors, this scoring system, unlike the Penn classification, provides a numerical estimation of mortality risk but requires a lengthier calculation time, potentially making it unsuitable for the most emergent situations.
The aforementioned tools are instrumental in assisting physicians to thoroughly assess the key aspects of aortic dissection, ensuring an accurate and comprehensive evaluation of the condition. The Penn classification was developed to serve as a straightforward and efficient tool that prioritizes physiological factors, aligning with our institution's direct-to-operating-room approach for treating acute type A aortic dissection. Due to its practical and simple to use, it remains a well-recognized and widely adopted tool for bedside evaluation of patients with acute aortic dissection. Recently, we reported that the Penn classification has significantly higher discrimination power for 30-day mortality than other more anatomically based classification systems.5
As explained earlier, malperfusion is a critical factor for the survival of patients. Historically, acute Type A aortic dissection has been treated surgically with a proximal-first approach. However, the debate over primary distal management in patients presenting with mesenteric malperfusion is still subject to discussion and is gaining traction within the cardiothoracic surgery community, so that the American Heart Association (AHA) has issued a class 2a recommendation for a primary distal approach in case of mesenteric malperfusion in its 2022 guidelines.13 Also, for the most stable patients, the same guidelines recommend with class 2a a transfer to high-volume aortic surgery centers to improve the survival of patients sufficiently stable for such a transfer. Given the above, we will probably see a paradigm change in the management of acute aortic syndromes over the next few years, during which it will be extremely important for all involved parties to speak the same language when defining malperfusion. The Penn classification enables a quick evaluation of risk, in these critical situations where urgency and efficiency are of utmost importance and time is of the essence. Prognostic information can be communicated to patients and their families to facilitate informed consent and set appropriate expectations. Additionally, the Penn classification offers a simple and reproducible approach for outcome adjustment, aiding in quality improvement efforts.
We advocate for the widespread adoption of the Penn classification by healthcare professionals treating aortic dissections. Its application can lead to a more standardized approach in managing these complex cases, potentially improving surgical outcomes and patient survival rates. As the medical community continues to strive for excellence in patient care, integrating such evidence-based tools into clinical practice is essential for advancing the field and ensuring the best possible outcomes for patients with acute aortic syndromes.