Laparoscopic surgery has begun to replace a great number of procedures that were previously practiced using open or conventional techniques. This is due to the minimal invasion, small incisions, and short time recovery. However, it has come to knowledge, that the increase in intra-abdominal pressure due to carbon dioxide pneumoperitoneum during laparoscopic surgery causes cardiovascular, respiratory, endocrine, and renal alterations.
ObjectiveTo evaluate the nephroprotective effect of Telmisartan, an angiotensin II AT1 receptor antagonist, on glomerular filtration in laparoscopic surgery.
Material and methodsAnalytical prospective, randomised, double-blind study was conducted on patients undergoing elective laparoscopic cholecystectomy. They were randomised into 2 groups, with the treatment group receiving a single dose of 40mg Telmisartan orally 2h prior to surgery, and the placebo group.
ResultsThere were 20 patients in each group (n=40), with a mean age of 32.65 years in the treatment group. Plasma creatinine did not show any significant change in the different time lapse in which blood samples were taken, but creatinine clearance at the end of surgery (196.415±56.507 vs. 150.1995±75.081; p=0.034), and at 2h postoperative period (162.105±44.756 vs. 113.235±31.228; p≤0.001) was statistically significant, which supports an increase in renal function in the Telmisartan group.
ConclusionThe use of Telmisartan, an angiotensin II AT1 receptor antagonist, offers renal protection during laparoscopic surgery.
La cirugía laparoscópica ha remplazado gran variedad de procedimientos que anteriormente se realizaban con técnica abierta o convencional, debido a su mínima invasión, incisiones pequeñas y rápida recuperación. Sin embargo, el aumento de la presión intraabdominal por el neumoperitoneo con dióxido de carbono causa alteraciones: cardiovasculares, respiratorias, endocrinas y renales.
ObjetivoEvaluar el efecto nefroprotector del telmisartán, un antagonista de los receptores AT1 de la angiotensina II, en la filtración glomerular en cirugía laparoscópica.
Material y métodosEstudio analítico prospectivo, aleatorizado, doble ciego, en pacientes intervenidos mediante colecistectomía laparoscópica electiva. Se aleatorizaron en 2 grupos, el grupo de tratamiento recibió 40mg de telmisartán por vía oral en dosis única 2 h antes de la cirugía y el otro grupo, placebo.
ResultadosSe analizaron 20 pacientes por grupo (n=40) con una media de edad de 32.65 en el grupo de tratamiento. La creatinina plasmática no mostró cambios significativos en los distintos tiempos en los que se tomó la muestra, pero la depuración de creatinina al final de la cirugía (196.415±56.507 vs. 150.1995±75.081; p=0.034) y a las 2 h potsoperatorias (162.105±44.756 vs. 113.235±31.228; p=≤ 0.001) presentaron datos estadísticamente significativos, que apoyan el aumento de la función renal con el grupo de telmisartán.
ConclusionesEl uso de telmisartán, un antagonista de los receptores AT1 de la angiotensina II, ofrece medidas nefroprotectoras durante la cirugía laparoscópica.
The role of laparoscopic surgery has broadened in recent years. This minimally invasive technique for complex surgical procedures with a short recovery time is now in widespread use. The annual incidence of cholecystolithiasis is approximately 1/200 people. Cholecystectomy is the treatment of choice for symptomatic cholecystectomy. Every year more than 500,000 cholecystectomies are performed in the United States, while 600,000 are performed in the United Kingdom. Approximately 80% of cholecystectomies are performed laparoscopically.1,2
Pneumoperitoneum is a non-physiological condition that brings about an increase in intra-abdominal pressure; this pressure increase is transmitted to the intra-abdominal organs, including the kidneys. An intra-abdominal pressure above 10mm/Hg leads to a transitory state of oliguria, a reduction in glomerular filtration and renal blood flow.1,3
The CO2 insufflated during laparoscopic surgery is quickly absorbed into the circulation, leading to respiratory acidosis and haemodynamic changes. It also compromises capillary circulation in the intra-abdominal organs. The increase in intra-abdominal pressure causes respiratory, cardiovascular and renal alterations. The flow of blood in the mesenteric, splenic and hepatic artery falls, as does renal perfusion with the increase in intra-abdominal pressure.3–5
ObjectiveTo evaluate the effect of Telmisartan, an AT1 angiotensin II receptor antagonist, in glomerular filtration in patients operated using elective laparoscopic surgery with carbon dioxide pneumoperitoneum.
Material and methodsThis analytical study is prospective, longitudinal, randomised, controlled and double-blind, in patients subjected to elective laparoscopic cholecystectomy, who were admitted to hospital in the period from September 2015 to January 2016, in the University Hospital, Universidad Autónoma Nuevo León (UANL), in Monterrey (Nuevo León, México).
The population studied consisted of patients over the age of 18 years old, ASA I and II (the American Society of Anesthesiologists classification), operated by laparoscopic cholecystectomy in the General Surgery Department of the University Hospital (UANL). Patients with kidney disease, diabetes mellitus or liver disease were excluded, as were those taking antihypertensive drugs or those in whom cholecystectomy was converted to open technique.
They were divided at random into 2 groups with the aid of the Microsoft Excel 2007 program; group 1, the treatment group, received a single oral dose of 40mg Telmisartan 2h before surgery, while group 2 received a placebo. They were randomly divided into 2 groups on admission using a sealed envelope, and they were given a capsule to take orally in a single dose 2h before surgery. This study was approved by the Ethics and Research Committee of the Institution, and the informed consent of each patient was obtained.
General and demographic data were recorded: patient weight, height, body mass index and ASA classification.
The patients received standard general anaesthesia for laparoscopic cholecystectomy. They were given 0.05–0.15mg/kg Midazolam and 2–20μg/kg Fentanyl, followed by 1.7–2.4mg/kg Propofol. Muscle relaxation was sought using Atracurium at 0.4–0.5mg/kg. Anaesthesia was maintained by Isoflurane (0.8–1.2vol/%) and a mixture of air and oxygen (rate 0.40). Ventilation was in assist-control mode with frequency and tidal volume sufficient to maintain normocapnia (35–38mmHg). After general anaesthesia a Foley tube and nasogastric tube were inserted. Patient monitoring included: capnography, pulse oxymetry, electrocardiograph and non-invasive measurements of arterial pressure. The laparoscopic cholecystectomy was performed with carbon dioxide pneumoperitoneum at a maintained pressure of 15mmHg and at a rate of from 1 to 1.5l/min.
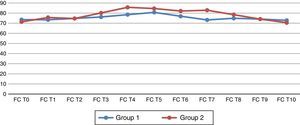
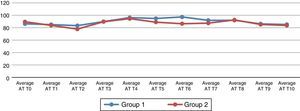
The haemodynamic variables included heart rate and average arterial pressure. These were recorded at the following times: (T0) before the induction of the anaesthesia; (T1) after the induction of anaesthesia but before tracheal intubation; (T2) 5min after tracheal intubation, (T3) immediately after creating the pneumoperitoneum; (T4) 15min after creating the pneumoperitoneum; (T5) 30min after creating the pneumoperitoneum; (T6) 45min after creating the pneumoperitoneum; (T7) after ending the pneumoperitoneum; (T8) 30min after ending the pneumoperitoneum; (T9) 24h after the operation and (T10) 48h after the operation.
Creatinine levels were measured before surgery, at the end of the pneumoperitoneum and 2, 24, and 48h after the operation.
Diuresis, corrected creatinine clearance or filtration (CrCl) and sodium excretion fraction (FENA) were calculated at the end of the pneumoperitoneum and 2h after the operation.
Diuresis was calculated by dividing the volume of urine and the time during which it was collected. Corrected creatinine clearance was calculated according to the formula CrCl=(UCr×UVol)/(PCr×Tmin), where UCr is the concentration of urinary creatinine, UVol is the volume of urine, PCr is the concentration of creatinine in plasma and Tmin is the time during which urine was collected. CrCl was corrected according to body surface area, CrCl×1.73m2/area of body surface. The sodium excretion fraction (FENA) was calculated by using the following formula: FENA=(UNa×PCr)/(PNa×UCr)×100, where UNa is the concentration of sodium in the urine and PNa is the concentration of sodium in plasma.
Creatinine clearance before surgery and at 24h and 48h after surgery was calculated using the modified Cockcroft-Gault equation, corrected by body surface area (Cockcroft-Gault formula×1.73m2/body surface area). Cockcroft-Gault formula: for men CrCl=[(140−age)×weight×1.2]/Cr in plasma, and for women CrCl=[(140−age)×weight]/Cr in plasma.
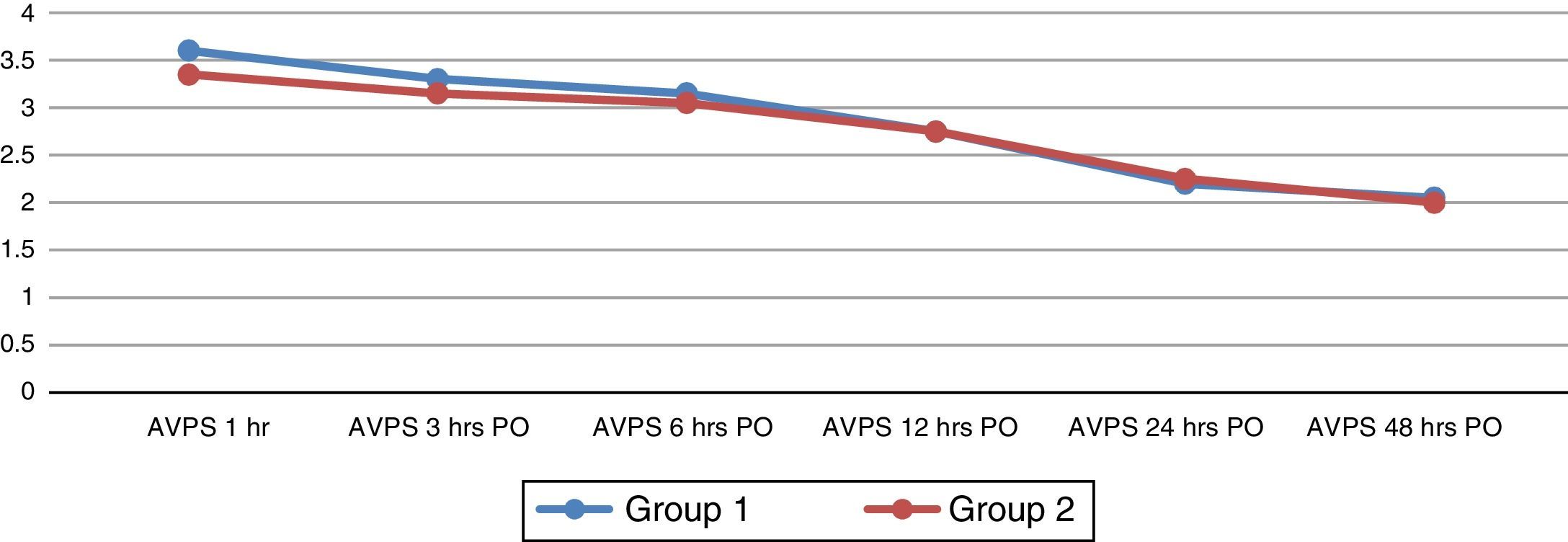
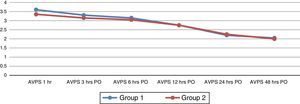
The duration of anaesthesia, transoperative hydration and the duration of surgery were recorded. The intensity of postoperative pain was evaluated using the 10 point visual-analogue pain scale. This was recorded at 1, 3, 6, 12, 24 and 48h after surgery.
Statistical analysis. The variables were evaluated separately using Pearson's chi-squared test and coefficient for categorical variables and Student's t-test for continuous variables. A value of p<0.05 was considered significant.
Using a formula to test the hypothesis and difference between 2 means, with a zα value of 1.96 and a 95% level of significance for 2 tails, and a zβ value of 0.84 with a power of 80%, a sample of 20 participants per group was obtained. Statistical analysis was carried out using the SPSS version 20 program (SPSS, Inc., Armon, NY, USA).
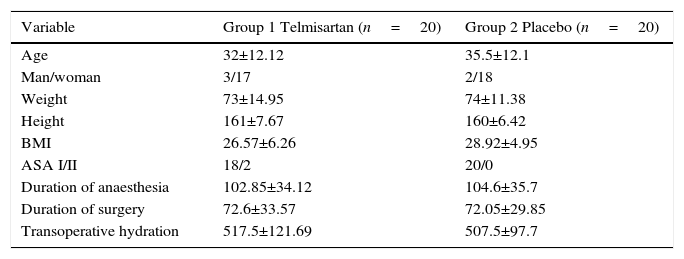
Results43 patients were included, of which 3 were excluded due to conversion to conventional surgery. 20 patients were analysed per group (n=40). The basal characteristics of the patients and the surgical variables were comparables and homogeneous (Table 1).
Biometric and surgical characteristics.
| Variable | Group 1 Telmisartan (n=20) | Group 2 Placebo (n=20) |
|---|---|---|
| Age | 32±12.12 | 35.5±12.1 |
| Man/woman | 3/17 | 2/18 |
| Weight | 73±14.95 | 74±11.38 |
| Height | 161±7.67 | 160±6.42 |
| BMI | 26.57±6.26 | 28.92±4.95 |
| ASA I/II | 18/2 | 20/0 |
| Duration of anaesthesia | 102.85±34.12 | 104.6±35.7 |
| Duration of surgery | 72.6±33.57 | 72.05±29.85 |
| Transoperative hydration | 517.5±121.69 | 507.5±97.7 |
ASA: American Society of Anesthesiologists classification; BMI: body mass index.
Data are shown as medians and standard deviations.
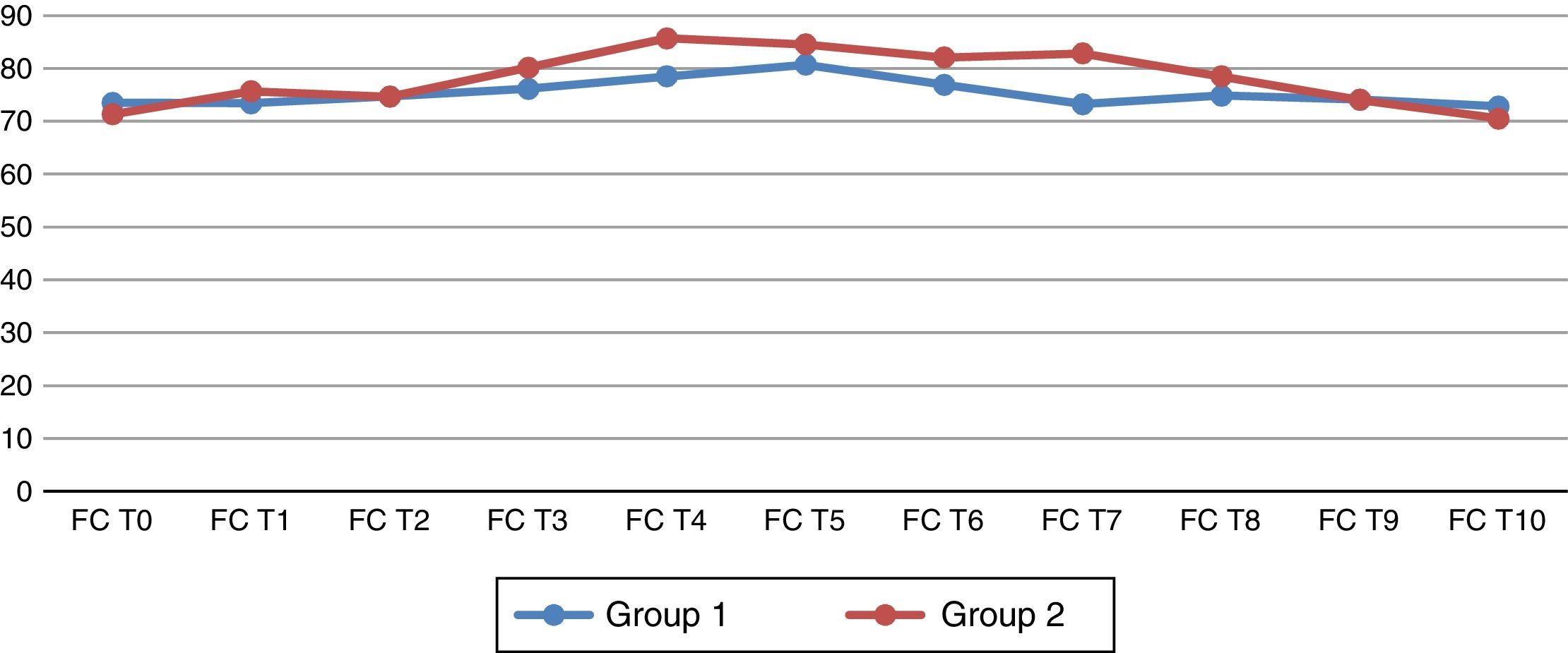
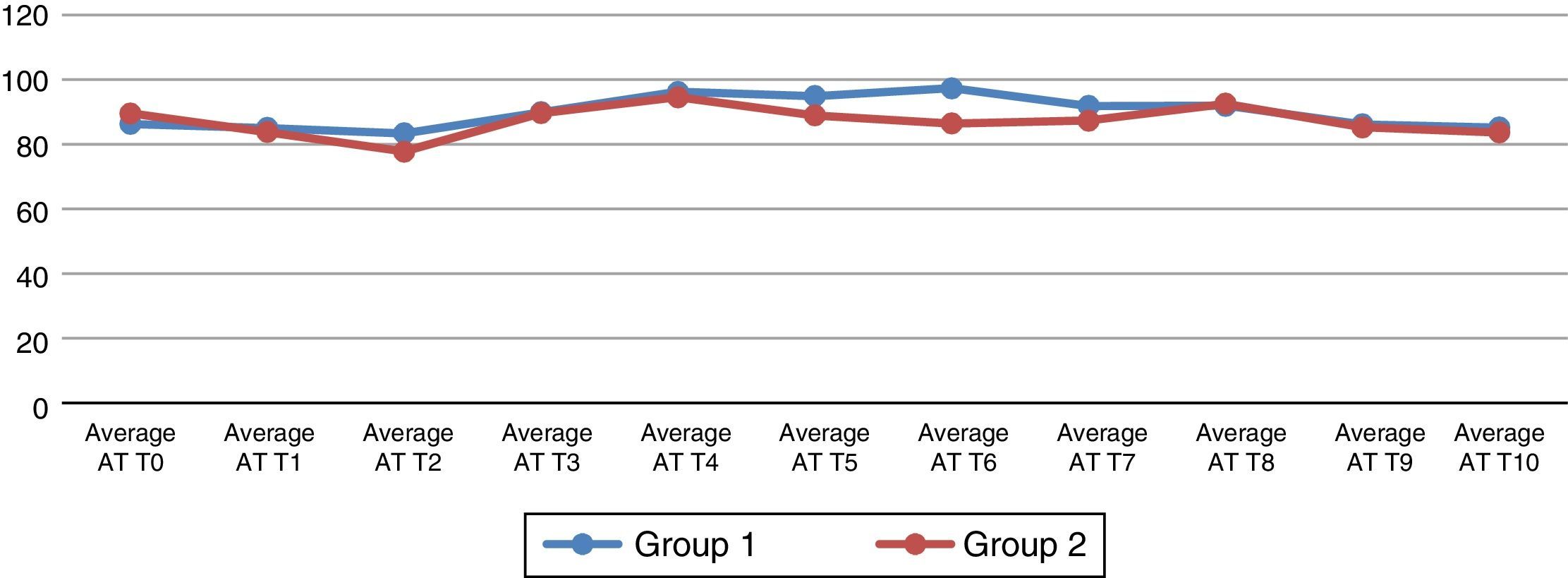
When the haemodynamic variables were analysed, statistically significant changes in the Telmisartan group were found in the heart rate when the pneumoperitoneum was ended (T7) (p=0.026) (Fig. 1). The average arterial pressure (AAP) 45min after pneumoperitoneum (T6) showed statistically significant changes in comparison with group 2 (p=0.044) (Fig. 2).
Basal heart rate and at different times during the study. (T0) before the induction of the anaesthesia; (T1) after the induction of anaesthesia but before tracheal intubation; (T2) 5min after tracheal intubation, (T3) immediately after creating the pneumoperitoneum; (T4) 15min after creating the pneumoperitoneum; (T5) 30min after creating the pneumoperitoneum; (T6) 45min after creating the pneumoperitoneum; (T7) after ending the pneumoperitoneum; (T8) 30min after ending the pneumoperitoneum; (T9) 24h after the operation and (T10) 48h after the operation.
Average basal arterial pressure (AAP) and at different times during the study. (T0) before the induction of the anaesthesia; (T1) after the induction of anaesthesia but before tracheal intubation; (T2) 5min after tracheal intubation, (T3) immediately after creating the pneumoperitoneum; (T4) 15min after creating the pneumoperitoneum; (T5) 30min after creating the pneumoperitoneum; (T6) 45min after creating the pneumoperitoneum; (T7) after ending the pneumoperitoneum; (T8) 30min after ending the pneumoperitoneum; (T9) 24h after the operation and (T10) 48h after the operation.
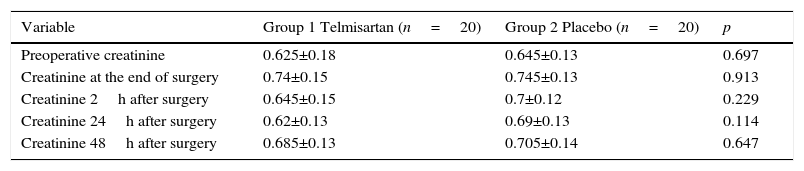
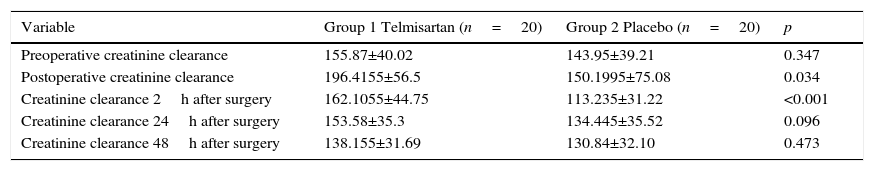
When plasmatic creatinine was analysed, this showed no significant changes at the different times when samples were taken (p=0.114), although creatinine clearance at the end of surgery (p=0.034) and 2h after the operation (p≤0.001) showed statistically significant changes in the Telmisartan group (Tables 2 and 3).
Plasmatic creatinine values at the different times data were recorded in the study.
| Variable | Group 1 Telmisartan (n=20) | Group 2 Placebo (n=20) | p |
|---|---|---|---|
| Preoperative creatinine | 0.625±0.18 | 0.645±0.13 | 0.697 |
| Creatinine at the end of surgery | 0.74±0.15 | 0.745±0.13 | 0.913 |
| Creatinine 2h after surgery | 0.645±0.15 | 0.7±0.12 | 0.229 |
| Creatinine 24h after surgery | 0.62±0.13 | 0.69±0.13 | 0.114 |
| Creatinine 48h after surgery | 0.685±0.13 | 0.705±0.14 | 0.647 |
Data are shown as medians and standard deviations.
Creatinine clearance values at the different times data were recorded in the study.
| Variable | Group 1 Telmisartan (n=20) | Group 2 Placebo (n=20) | p |
|---|---|---|---|
| Preoperative creatinine clearance | 155.87±40.02 | 143.95±39.21 | 0.347 |
| Postoperative creatinine clearance | 196.4155±56.5 | 150.1995±75.08 | 0.034 |
| Creatinine clearance 2h after surgery | 162.1055±44.75 | 113.235±31.22 | <0.001 |
| Creatinine clearance 24h after surgery | 153.58±35.3 | 134.445±35.52 | 0.096 |
| Creatinine clearance 48h after surgery | 138.155±31.69 | 130.84±32.10 | 0.473 |
Data are shown as medians and standard deviations.
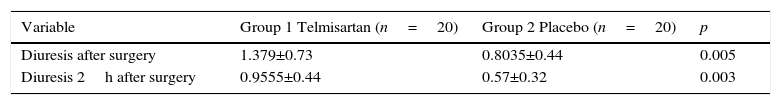
Diuresis at the end of surgery (p=0.005) and at 2h after surgery (p=0.003) showed significant changes in the Telmisartan group (Table 4).
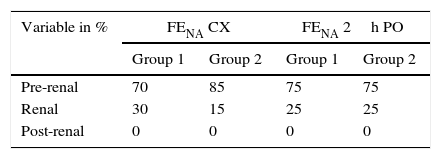
The sodium excretion fraction (FENA) was found in 70% of the patients in group 1 and in 85% of those in group 2 to show a pre-renal lesion at the end of surgery, while 75% of the patients in both groups presented a pre-renal lesion 2h after the operation. This shows a functional or physiological change that was possibly influenced by the surgical procedure (Table 5).
There is no significant evidence in the results of the analogue visual pain scale in both groups at the different times when it was applied (Fig. 3). No association was found between the groups and the variables analysed using the chi-squared test at 95% confidence. No complications or adverse effects were recorded during the study.
DiscussionAngiotensin II (ARA II) receptor antagonists are a group of antihypertensive drugs that have appeared recently for the treatment of arterial hypertension and heart failure. The main ones commercialised are Candesartan, Eprosartan, Irbesartan, Telmisartan and Valsartan. They act by blocking the binding of angiotensin II to type 1 angiotensin II receptors (AT1), which are present in many tissues such as smooth muscle tissue, the adrenal gland and myocardium. As a result they inhibit its vasopressor and aldosterone liberating effect.6–8
Pneumoperitoneum gives rise to a reduction in total lung volume, residual capacity and pulmonary compliance, facilitating the development of atelectasias. CO2 insufflation into the abdominal cavity leads to hypercapnia due to diffusion of the gas through the peritoneum, causing hypoxaemia, hypercapnia and respiratory acidosis; it also causes significant haemodynamic alterations and reduces cardiac output by 10–30%.9
In our study the groups analysed were homogeneous, and it is interesting that the heart rate when the pneumoperitoneum was removed (T7), showed favourable and cardioprotective haemodynamic changes, as the heart rate fell (73.25±11.70 vs. 82.85±14.33; p=0.026).
When average arterial pressure (AAP) is analysed 45min after the pneumoperitoneum (T6) in the Telmisartan group, it shows an increase in the AAP (97.31±20.100 vs. 86.435±11.549; p=0.044). The AAP is considered to be the perfusion pressure of the bodily organs, and a value of >60mmHg is sufficient to satisfy their demand. Although the exact mechanism which raised the AAP in the treatment group is not fully clear, we know that pneumoperitoneum and the Trendelenburg position cause an increase in the AAP, central venous pressure, average pulmonary pressure, pulmonary capillary wedge pressure and systemic vascular resistance. The perioperative administration of ARA II leads to a risk of severe hypotension under the effects of anaesthesia, particularly following induction. However, some studies show that sympatic activity may cause an increase in arterial pressure and an increase in the heart rate in normotensive individuals during the surgical procedure.10 Nevertheless, the clinical importance of these actions may in the future be the basis for the selection of a specific ARA II, as we lack comparative studies in normotensive patients with the use of the different ARA II, and which would allow us to know all of their properties. Nor do we know if any of them has advantages over the others.
Renal blood flow and glomerular filtration fell by at least 50% during laparoscopic surgery. This fall in the blood flow has also been detected in the mesenteric vessels and in other organs, such as the liver, pancreas, stomach, spleen and intestine.
Diuresis falls, and this is attributed to the increase in rennin activity and the direct compression of the lower cava vein, renal vasculature and parenchyma by the pneumoperitoneum. This was found in the study by Koivusalo et al.3 which compared the reduction in kidney function which occurs when using a method for the retraction of the abdominal wall versus a conventional method of pneumoperitoneum.11
When using Telmisartan during laparoscopic surgery we find that diuresis and creatinine clearance show significant changes as a nephroprotector at the end of surgery and 2h after the procedure.
The importance of renal perfusion and pathological physiological after-effects during pneumoperitoneum have increased, especially with the introduction of kidney donation using laparoscopic nephrectomy.5,12,13
The ARA II drugs have a good safety profile. Telmisartan is swiftly absorbed when taken orally, attaining its Cmax after 0.5–1h. It reduces renal vascular resistance, especially the resistance of the afferent arterioles, resulting in an increase in renal blood flow.14–16
ConclusionsThe early detection of altered or borderline kidney function is important in patients who will be treated using laparoscopic procedures, so that they can be offered nephroprotective measures. Some studies show the effects of pneumoperitoneum on haemodynamic changes and visceral perfusion during laparoscopic surgery, and many of these are spontaneously reversible.
To conclude, we show that the use of Telmisartan, an angiotensin II (ARA II) AT1 receptor antagonist, offers nephroprotective effects during laparoscopic surgery. Future studies will be necessary to determine the degrees to which different medications in the market have a nephroprotective effect, as well as in patients with kidney pathologies who have been operated using laparoscopic surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to especially thank the team of nurses and surgeons in the Outpatient Surgery Department of Hospital Universitario UANL for their patience and help in undertaking this study.
Please cite this article as: Fuentes-Reyes RA, Pacheco-Patiño MF, Ponce-Escobedo AN, Muñoz-Maldonado GE, Hernandez-Guedea MA. Impacto de telmisartán en la filtración glomerular en cirugía laparoscópica. Estudio aleatorizado doble ciego. Cir Cir. 2017;85:34–40.