Splenic abscess is a rare clinic entity, its incidence has increased due to the rising number of clinical conditions involving immunosuppression. Endocarditis is the most frequent cause, and gram-positive aerobes are the main causal agents. Its clinical presentation is non-specific and delays diagnosis. Computed tomography scan is the method of choice, and the treatment is based on antibiotics and drainage, radiological or surgical, involving splenectomy in special cases that require it.
Clinical caseA 55-year-old man with abdominal pain and fever. The analysis revealed leukocytosis 14,000/mm3, prothrombin activity 53%, and metabolic acidosis. Computed tomography scan showed a peri-hepatic pneumoperitoneum, liquid fluid, and peri-splenic bubbles, and slight trabeculation of fat around the duodenal bulb with pneumoperitoneum in this area. Patient underwent a median laparotomy, finding a purulent peritonitis due to a ruptured abscess in the spleen, splenectomy was performed. Fluid culture showed polymorphonuclears, with no microorganisms identified. The patient progressed and was discharged on the 5th post-operative day.
ConclusionsSplenic abscess is an uncommon condition, in which the diagnosis is delayed and mortality, in untreated patients, is high. Its association with pneumoperitoneum may confuse the diagnosis towards viscera perforation. Thus it must be suspected in the finding of unknown cause of pneumoperitoneum by complementary examinations. The treatment of choice is splenectomy, because the capsular rupture is the norm in all of them.
El absceso esplénico es una entidad clínica poco frecuente que ha incrementado su incidencia por el aumento de condiciones clínicas de inmunosupresión. La endocarditis es la causa más frecuente, y las infecciones por grampositivos son los gérmenes más frecuentemente aislados. Su presentación clínica es inespecífica, lo que retrasa el diagnóstico. La tomografía es el método de elección, y el tratamiento se basa en antibioterapia y drenaje, asociando esplenectomía en casos especiales que lo precisan.
Caso clínicoHombre de 55 años que acude por dolor abdominal y fiebre. En el reporte de laboratorio destaca: leucocitosis de 14,000/mm3, actividad de protrombina 53% y acidosis metabólica. La tomografía muestra neumoperitoneo perihepático, líquido libre, burbujas periesplénicas y trabeculación de la grasa alrededor del bulbo duodenal, que se continúa con neumoperitoneo en la región antepilórica. El paciente es intervenido quirúrgicamente, hallando una peritonitis purulenta por rotura de absceso esplénico, realizándose esplenectomía. El cultivo muestra polimorfonucleares sin germen identificado. El paciente evoluciona favorablemente y es egresado al 5.°día del postoperatorio.
ConclusionesEl absceso esplénico es una patología poco frecuente cuyo diagnóstico es tardío, y su mortalidad es elevada en pacientes no tratados. Su asociación con neumoperitoneo puede confundir el diagnóstico hacia perforación de víscera hueca, por lo que hay que sospecharlo ante un neumoperitoneo de causa no aclarada, por las exploraciones complementarias. El tratamiento de elección es la esplenectomía, ya que la rotura capsular es la norma en todos ellos.
Splenic abscess is a rare clinical entity with a documented incidence of between 0.14% and 0.7% in autopsies.1,2 This pathology generally presents in patients with neoplasias, immunodeficiency, trauma, metastatic infection, splenic infarction, or diabetes.3 Endocarditis is the most frequent cause, and gram-positive aerobes are the main causal agents, with gram-negative aerobes and enteric bacteria generally being associated with other intra-abdominal foci.4 Incidence is believed to be increasing particularly due to the growing number of immune-compromised patients, who are more likely to present with this pathology and also to the fact that there is greater availability and use of imaging techniques such as computed tomography and ultrasound.5 The management of splenic abscesses is based on antibiotics and assessing the possibility of percutaneous or surgical drainage, plus the possible involvement of splenectomy, depending on each case. Failure rates in percutaneous drainage are high (14.3–75%), whilst surgery remains the most effective treatment when drainage is not possible, is ineffective or the al condition of the patient will not allow it.5–11 Although treatment results are good, mortality remains high. This is attributed to delayed diagnosis, due to non-specific symptoms and signs in over half of all cases.12
The aim of this report is to provide information about this rare infectious complication and its association with the radiological finding of pneumoperitoneum, which may lead us to establish an incorrect diagnosis and thus delay necessary treatment.
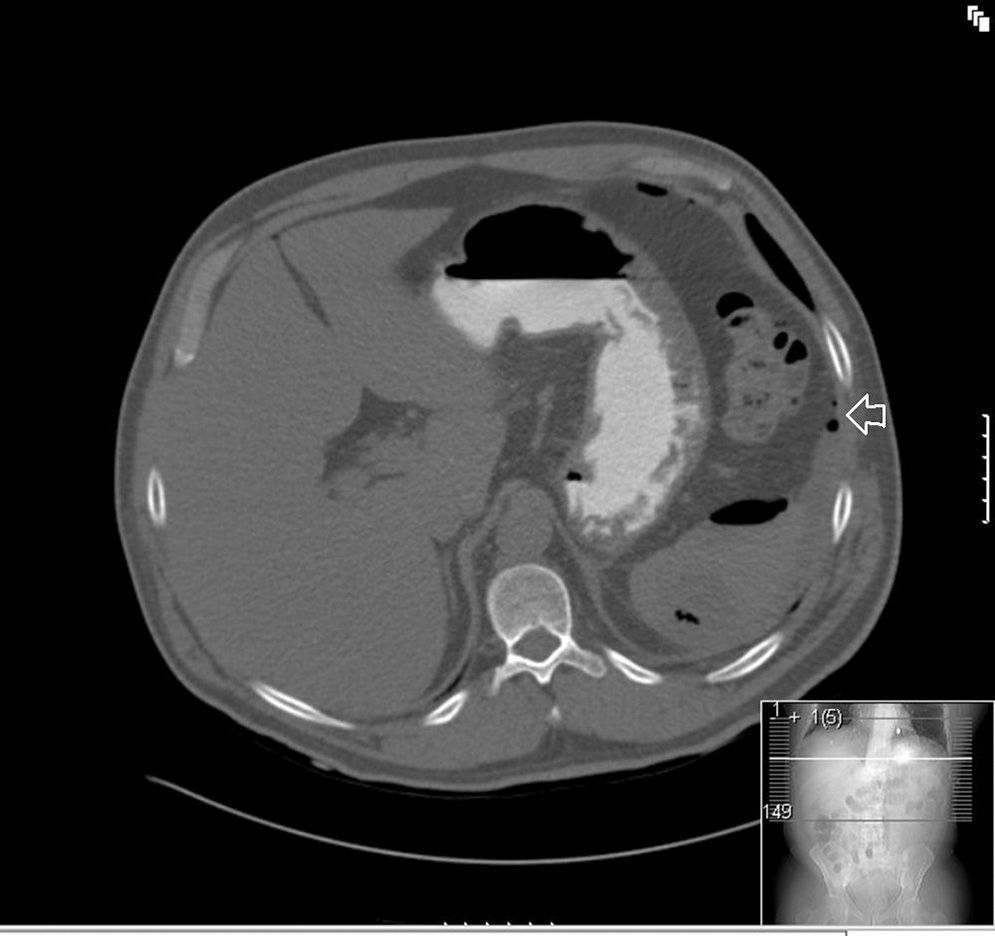
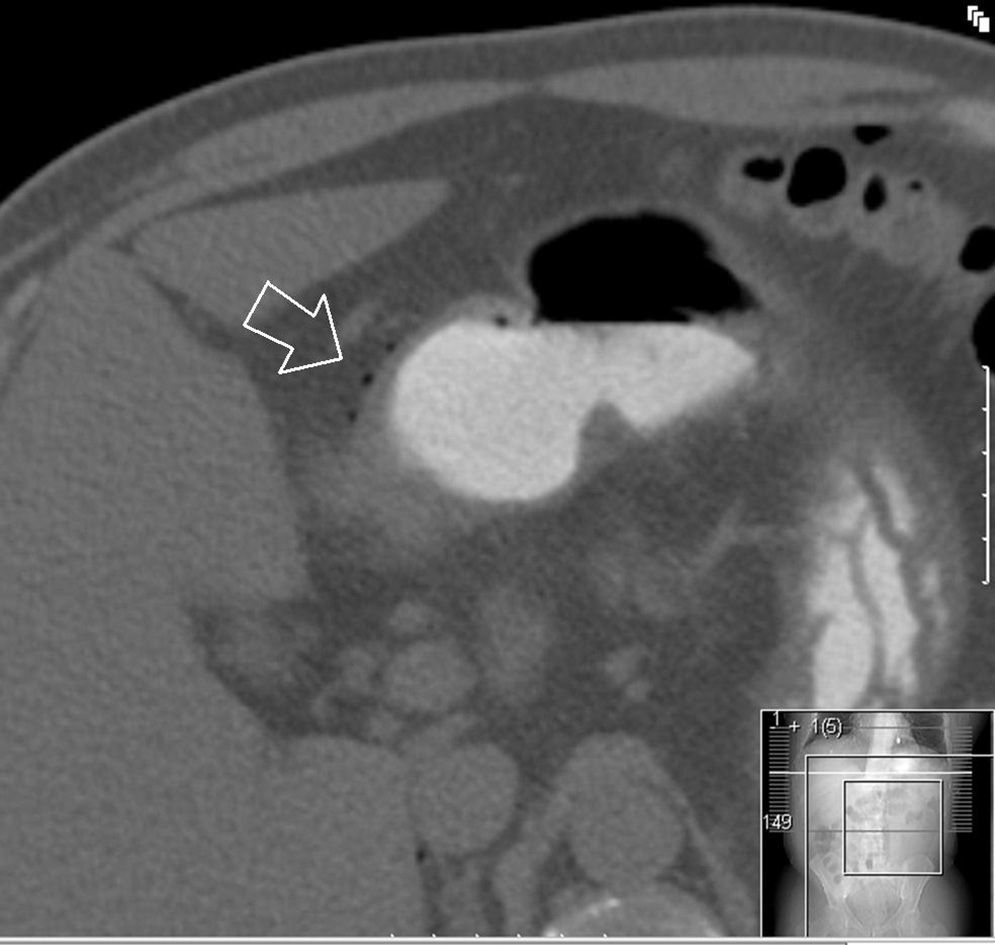
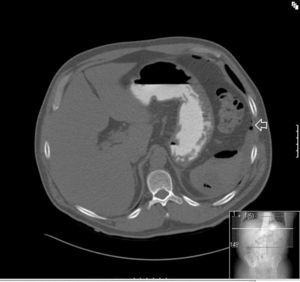
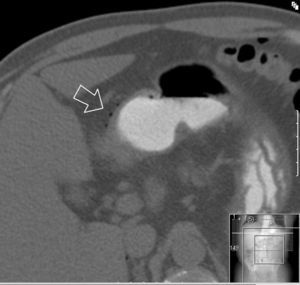
Clinical caseA 55 year old male presented at the emergency services with a 10-day history of abdominal pain, located in the epigastrium and fever of up to 40°C. He had a clinical history of diabetes mellitus type 2, coronary heart disease, and was the bearer of three coronary stents. He had received surgery for neoplasia of the tongue with radical excision and postoperative radiotherapy 13 years previously. On examination sharp abdominal pain in the upper abdomen was noted, with signs of peritoneal irritation and abdominal guarding, which did not improve with intravenous (i.v.) analgesics. On arrival at the emergency services he presented with a temperature of 38.7°C, a heartbeat of 110bpm with blood pressure of 90/40mmHg. Laboratory results showed leucocytosis of 14,000/mm3 with 88% white blood cells, prothrombin activity of 53% and a D-dimer test level of 2000. Blood gases showed a pH of 7.30, with a lactic acid level of 2.5mmol/l. The chest X-ray showed right subdiaphragmatic pneumoperitoneum (Fig. 1), and in the X-ray of the abdomen swelling of the small intestinal loops was observed. Computed tomography of the abdomen was performed which showed a perihepatic pneumoperitoneum, liquid fluid and peri-splenic bubbles (Fig. 2), and slight trabeculation of fat around the duodenal bulb with pneumoperitoneum in the ante pyloric region (Fig. 3), compatible with a splenic abscess or duodenal perforation. Antibiotic prophylaxis with amoxycillin-clavulanic acid (2g/200mg i.v.) was administered prior to surgery. The patient underwent median laparotomy, with the finding of purulent peritonitis in the supramesocolic space due to a ruptured abscess in the upper pole of the spleen. Splenectomy was performed, with aspiration drainage left at the splenectomy site. Postoperative antibiotic treatment with 1g of meropenem was administered intravenously every 8hours. Fluid culture showed few polymorphonuclears with no gas-producing microorganisms identified. Anatomic pathology report findings were: spleen weighing 245g, friable consistency, with abscessed and necrotic inflammation in its upper pole, with traces of fluid from the splenic capsule. The patient evolved favourably, and drainage was removed on the third day after surgery. A transesophageal echocardiogram was performed which ruled out the presence of endocarditis. The patient was discharged from hospital 5 days after the procedure with oral antibiotic therapy of amoxicillin/clavulanic acid (200/135mg every 12hours) to be taken at home.
Although splenic abscess is an infrequent clinical entity, it should be included in the differential diagnosis of patients presenting at hospital with sharp abdominal pain or for those who are found on examination to have pneumoperitoneum. This should be particularly noted in immune-compromised patients with comorbidities such as neoplasia, diabetes, trauma or a clinical history of splenic infarction or splenic embolism.13
The aetiology of splenic abscesses is divided into 5 major groups: haematogenous metastatic infection (bacterial endocarditis being the most frequent), infection by contiguity, infection secondary to splenic infarction, splenic trauma, or immunodepression.2
The microorganisms identified in the majority of the series are most frequently aerobes (streptococcus, staphylococcus, Escherichia coli, enterococci, Pseudomonas, etc.), although geographical variations exist,14 and in immuno-depressed patients the presence of anaerobic microorganisms, microbacteria and fungal infections increases.15 In the Ooi and Leong16 series, 287 pacients were reported as having 11.4% negative cultures, as occurred in our series.
Regarding clinical presentation, fever is the most common symptom, followed by abdominal pain and shivering. The typical triad of fever, pain in the left hypochondrium and palpable mass was identified by Sarr and Zuidema17; however, it only presents in 32%-59% of cases, and is even rarer in immune-compromised patients,18 with a delay of up to 2 weeks in diagnosis following the onset of symptoms.2 In the other diagnostic tests leucocytosis appears in two thirds of cases16; chest and abdomen X-rays may show a mass in the upper left quadrant, a displacement of the gastric chamber and the presence of pneumoperitoneum, in addition to ipsilateral pleural effusion and elevation of the left hemidiaphragm. Computed tomography and ultrasound are the method of choice, with the former being the gold standard due to its greater sensitivity.16
Regarding treatment, the series published chose antibiotic therapy alone or with percutaneous drainage or splenectomy. Mortality rates did not differ in the 3 groups and appears to be more related to the underlying situation of the patient. Mortality has been greatly reduced with the use of wide spectrum antibiotics4 and antibiotic combinations, with radiologic drainage being used for those patients with safe anatomical accesses, a stable condition or at high surgical risk, and reserving splenectomy for those who have not responded to treatment or where the ruptured abscess has invaded the abdominal cavity.16,19,20 The aforementioned management has lowered mortality to under 10%,19 and to 25% in immune-depressed patients.16
Possible complications in percutaneous drainage are: haemorrhaging due to spleen puncture, injury to other organs and leakage of purulent material from the catheter when it is detached,16,19,21 and it is contraindicated when abscesses are small and multiple, when there are septa between them, bleeding diathesis, haemoperitoneum or anatomical inaccessibility. Absolute contraindication is when the abscess perforates the abdominal cavity, which occurs in up to 6.6% cases.16,19
In our case the only identifiable risk factor for the appearance of a splenic abscess was the presence of diabetes in the patient. Although he had undergone surgery for a tongue tumour, this took place a long time previously and the patient was tumour-free. Regarding disease aetiology, bacterial endocarditis, trauma or resultant infection were rejected and the immune-depressive status of the diabetic patient was the most plausible cause, be it associated with some type of haematogenous spread (urosepsis, dental infection, etc.) or not. This was not determined in our case.
In our patient, the presence of pneumoperitoneum led to a differential diagnosis where the hollow viscera perforation was considered the most probable option and not even computed tomography of the abdomen was able to offer a clear diagnosis of splenic abscess, with confirmation thus left to surgery. If duodenal perforation had been exclusively suspected, our approach would initially have been to use laparoscopy, but the diagnostic uncertainty led to a surgical approach using laparotomy. Treatment of splenic abscesses may involve laparoscopy in patient groups where the outcome is predicted as being favourable,8 or it may involve laparotomy. We believe, however, that in cases with capsular rupture and established peritonitis, an open surgical approach enables better visualisation and emptying of the cavity.
ConclusionsThe real incidence of splenic abscesses is as yet unknown, and we visualise an increase in its prevalence in upcoming years, due to the increase of immune-depression. Despite the diagnostic arsenal and almost universal availability of imaging methods, diagnosis is usually delayed, and mortality in untreated cases is approximately 100%. A suspected differential diagnosis of sharp abdominal pain must therefore exist for accurate and early treatment.
If the cause of pneumoperitoneum is unascertained, we must not forget how splenic abscess through gas producing germs may be a possibility, although hollow viscera perforation would be the first suspected cause; computed tomography may guide us on occasions as it may reveal spleen cell changes. The treatment of choice, however, continues to be surgery, since the presence of pneumoperitoneum suggests capsular rupture.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Peña-Ros E, Méndez-Martínez M, Vicente-Ruiz M, Sánchez-Cifuentes Á, Martínez-Sanz N, Marín-Blázquez AA. Neumoperitoneo por absceso esplénico: un reto diagnóstico. Reporte de un caso. Cir Cir. 2015;83:433–437.