Pneumoperitoneum is defined as the existence of extraluminal air in the abdominal cavity. In 80–90% of cases is due to perforation of a hollow organ. However, in 10–15% of cases, it is nonsurgical pneumoperitoneum.
ObjectiveThe case of a patient undergoing mechanical ventilation, developing abdominal compartment syndrome tension pneumoperitoneum is reported.
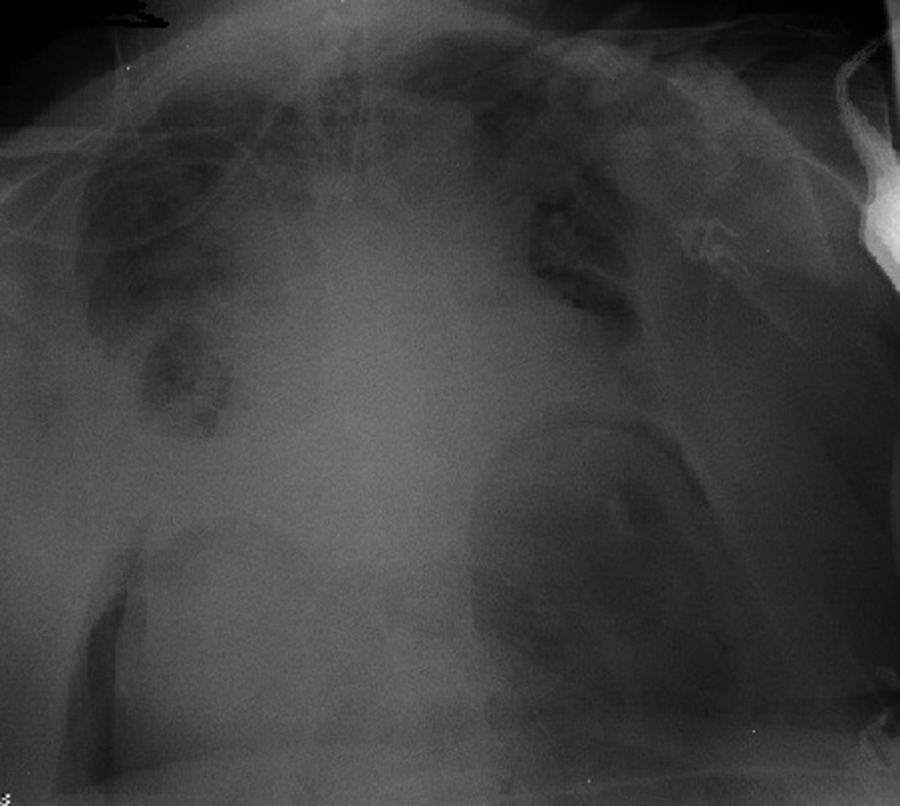
Clinical caseFemale, 75 years old asking for advise due to flu of long term duration. Given her respiratory instability, admission to the Intensive Care Unit is decided. It is then intubated and mechanically ventilated. Chest X-ray revealed a large pneumoperitoneum but no pneumothorax neither mediastinum, and due to the suspicion of viscera perforation with clinical instability secondary to intra-abdominal hypertension box, emergency surgery was decided.
ConclusionsWhen discarded medical history as a cause of pneumoperitoneum, it is considered that ventilation is the most common cause.
Benign idiopathic or nonsurgical pneumoperitoneum, can be treated conservatively if the patient agrees. But if intraabdominal hypertension prevails, it can result in severe respiratory and haemodynamic deterioration, sometimes requiring abdominal decompression to immediately get lower abdominal pressure and thus improve haemodynamic function.
El neumoperitoneo se define como la existencia de aire extraluminal en la cavidad abdominal. En el 80-90% de las ocasiones se debe a la perforación de una víscera hueca. No obstante, en un 10-15% de los casos se trata de neumoperitoneos no quirúrgicos.
ObjetivoPresentamos el caso de una paciente sometida a ventilación mecánica que desarrolla un síndrome compartimental abdominal por neumoperitoneo a tensión.
Caso clínicoPaciente mujer de 75años que consulta por síndrome gripal de días de evolución. Dada su inestabilidad respiratoria se decide su ingreso en la unidad de cuidados intensivos y se procede a su intubación orotraqueal con conexión a ventilación mecánica. En la radiografía de tórax se observa un gran neumoperitoneo sin neumotórax ni neumomediastino, por lo que, con la sospecha de perforación de víscera hueca y ante la inestabilidad clínica secundaria al cuadro de hipertensión intraabdominal, se decide su intervención quirúrgica urgente.
ConclusionesCuando se descartan antecedentes médicos como causa de neumoperitoneo, se considera que la ventilación es la causa más frecuente.
El neumoperitoneo benigno, idiopático o no quirúrgico, puede tratarse de forma conservadora si la clínica del paciente lo permite. Pero si existe un cuadro de hipertensión intraabdominal, puede producirse un grave deterioro hemodinámico y respiratorio que en ocasiones obliga a la descompresión abdominal de forma inmediata para conseguir disminuir la presión intraabdominal y, por tanto, mejorar la función hemodinámica del paciente.
Pneumoperitoneum is defined as the existence of extraluminal air in the peritoneal cavity. The first cause to be ruled out is hollow visceral perforation, which requires emergency surgical intervention.1
The condition referred to as a primary, idiopathic or benign pneumoperitoneum occurs in 10% to 15% of cases, and is not caused by intra-abdominal lesions. This condition is also called non-surgical pneumoperitoneum, because a wait-and-see approach can be taken with conservative treatment, avoiding unnecessary laparotomies, which increase morbidity and mortality.2
ObjectiveWe present the case of a patient who underwent mechanical ventilation, and who developed an abdominal compartment syndrome caused by tension pneumoperitoneum. Surgical decompression was decided, without demonstrating the abdominal cause responsible.
Clinical caseA 75-year-old woman with no medical history of interest attended the emergency department with flu-like symptoms of several days’ duration. The patient reported asthenia and dyspnoea, which were gradually increasing. On physical examination the patient was agitated, she was normotensive but tachycardic (108 beats/min), tachypneic (35 respirations/min), with oxygen saturation of 84% and a fever of 39°C. She presented mucocutaneous cyanosis and oedema to the middle third of the leg. Pulmonary auscultation showed hypoventilation in the base of the right lung, and there were no significant pathological findings in the other organs and systems.
Arterial gasometry was compatible with respiratory acidosis (pCO2 90, pH 7.14, HCO3 30, pO2 88). The chest X-ray showed findings compatible with pneumonic syndrome, and fibrobronchoscopy did not show significant lesions.
Given the patient's respiratory instability, it was decided that she should be admitted to the intensive care unit with a clinical diagnosis of acute respiratory failure secondary to a possible pneumonia acquired in the community. Treatment with corticosteroids was started and non-invasive ventilation with bilevel positive airway pressure (BiPAP).
Because this ventilation failed, the patient was intubated orotracheally and connected to mechanical ventilation. Twenty-four hours later she developed haemodynamic compromise (hypotension and tachycardia), and respiratory compromise (hypoxia and metabolic acidosis), and oligoanuria. On examination the patient had a very distended abdomen with tympanism and reduced bowel sounds. A chest X-ray showed findings compatible with a major pneumoperitoneum (Fig. 1). Neither a pneumothorax nor a pneumomediastinum were observed, with the suspicion of hollow visceral perforation, and given the patient's clinical instability secondary to symptoms of intra-abdominal hypertension, urgent surgical intervention was decided. Measures were not taken to deal with the intra-abdominal pressure as the patient's haemodynamic instability made emergency intervention necessary.
Surgical decompression caused an improvement in the patient's haemodynamic and respiratory parameters. The integrity of the intestinal loops was checked, and no lesions or findings suggestive of hollow visceral perforation were found.
There were no complications in the postoperative period, and after 12 days in the intensive care unit she was transferred to the ward, where the patient was kept haemodynamically stable until she recovered.
DiscussionThe most common cause of pneumoperitoneum is previous surgery, either laparotomy or laparoscopy. Air gradually reabsorbs and it resolves a week after surgery in more than 90% of patients.3
Once recent surgery has been ruled out as the cause of a pneumoperitoneum, hollow visceral perforation is responsible for 80% to 90% of cases, and gastric and duodenal ulcers are the most prevalent origin.4
Gastro-intestinal endoscopic procedures, the insertion of catheters for peritoneal dialysis, endoscopic postpolypectomy syndrome or intestinal cystic pneumatosis are other abdominal conditions which should be taken into consideration.5,6
Gynaecological origin or oropharyngeal manipulation are considered anecdotal and receive little mention in medical literature.7
Once abdominal pathology has been ruled out, the chest is the usual location. Chest causes have not been as well defined as abdominal causes, but ventilation is usually considered the most common cause.8,9
Barotrauma is defined as the presence of interstitial alveolar emphysema, pneumothorax, pneumomediastinum, pneumoperitoneum and subcutaneous emphysema. It develops in 15% to 25% of patients who have undergone mechanical ventilation, and mortality reaches levels of up to 35%.10
The transfer mechanism of air from the chest cavity to the abdomen was studied by Macklin and Macklin.11 The application of air under pressure on the trachea ruptures the alveoli, and the passage of air through the perivascular space to the mediastinum causes pneumomediastinum, and in some cases the air dissects the mediastinum until it reaches the retroperitoneum causing a pneumoretroperitoneum, when the air is applied at greater pressure this causes alveolar rupture into the pleural space which causes a pneumothorax, and due to small pleuroperitoneal anatomical defects, this increase in pressure allows the bidirectional flow of air between the chest and the abdomen, causing a pneumoperitoneum.
This is why there can be a clinical picture of pneumoperitoneum associated with signs of barotrauma such as pneumothorax, pneumomediastinum or subcutaneous emphysema.11–13
The case reported here is special because of the presence of a tension pneumoperitoneum causing an abdominal compartment syndrome not accompanied by the typical signs of barotrauma. Therefore, the first therapeutic measure chosen was a decompressive exploratory laparotomy to look for an abdominal cause for this clinical picture.
Most cases described in medical literature on tension pneumoperitoneum secondary to barotrauma, occur in patients who have undergone mechanical ventilation for various respiratory conditions, such as: bronchial asthma, respiratory distress, chronic bronchopneumonia, pulmonary emphysema or pneumonia. Intra-abdominal hypertension secondary to a pneumoperitoneum causes decreased venous return due to direct compression on the inferior vena cava, and due to increased cardiac after load. There is also a reduction of respiratory volume and pulmonary distensibility, along with renal compression which will culminate in aligoanuria.14,15
The severity of these system mechanisms requires intra-abdominal pressure to be reduced immediately, and thus improve haemodynamic function, as in the case of our patient.
Treatment of barotrauma will depend on the clinical repercussions, decompressive manoeuvres will be necessary if there is a tension pneumothorax.
The approach to be taken will also be dictated by the clinical manifestations. A tension pneumoperitoneum with haemodynamic and respiratory repercussions will require emergency abdominal decompression to prevent abdominal compartment syndrome, using either peritoneal puncture-lavage or laparotomy. Medical literature and experience demonstrate that these manoeuvres, performed as an emergency, achieve rapid improvement in the patient. Intraperitoneal drainage systems are used to reduce the morbimortality which surgical aggression entails.16–19
A simple pneumoperitoneum with no clinical repercussions can be treated conservatively with a wait-and-see approach, avoiding the increased morbidity and mortality implied by surgery.
ConclusionsWhen medical history has been ruled out as the cause of a pneumoperitoneum, ventilation is considered to be the most common cause.
A benign, idiopathic or non-surgical pneumoperitoneum can be treated conservatively if the patient's symptoms allow. But if there is a clinical picture of intra-abdominal hypertension, serious haemodynamic and respiratory deterioration can occur, which occasionally requires immediate abdominal decompression to reduce intra-abdominal pressure, and therefore, improve the patient's haemodynamic function.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: García-Santos E, Puerto-Puerto A, Sánchez-García S, Ruescas-García FJ, Alberca-Páramo A, Martín-Fernández J. Síndrome compartimental abdominal por neumoperitoneo a tensión secundario a barotrauma. Presentación de un caso. Cir Cir. 2015;83:429–432.