Gallbladder agenesis is a very rare congenital abnormality of the biliary tract. The diagnosis is made during surgery, because all preoperative studies have failed to identify this malformation.
The purpose of this article is to present a case of gallbladder agenesis diagnosed during surgery, its management, and a review of the literature.
Clinical caseThe case involves a sixty-two year-old female, referring to repeated biliary colic symptoms. The abdominal ultrasound diagnosed cholelithiasis. It was impossible to identify the gallbladder during surgery. Diagnosis was confirmed by intra-operative cholangiography.
DiscussionPreoperative diagnostic workup has failed to recognise patients with gallbladder agenesis. It is currently recommended to abandon the surgery once this diagnosis is suspected and confirm it by a cholangio-magnetic resonance scan in order to avoid a bile duct injury.
ConclusionsAgenesis of the gallbladder is a rare congenital abnormality of the biliary tree. Every surgeon must keep this rare entity in mind when a “difficult dissection” or an anatomic variant is identified during surgery, and make use of an intra-operative cholangiography, mainly to prevent a bile duct injury.
La agenesia de la vesícula biliar es la malformación menos frecuente de las vías biliares. Su diagnóstico suele realizarse en el transoperatorio. Los estudios de imagen son poco efectivos para detectar esta malformación congénita.
ObjetivoPresentar un caso clínico diagnosticado en el transoperatorio de agenesia de la vesícula biliar, su manejo y una revisión de la literatura.
Caso clínicoMujer de 62 años de edad, la cual acude a consulta por presentar cólicos biliares de repetición. El reporte de ultrasonido abdominal describe datos compatibles con colecistolitiasis. Al realizar la laparoscopia, no se identificó la vesícula biliar. Se confirmó el diagnóstico por colangiografía transoperatoria.
DiscusiónDurante el preoperatorio es difícil identificar a pacientes con agenesia vesicular. Actualmente se recomienda abandonar la laparoscopia cuando se sospecha agenesia vesicular para evitar lesionar las vías biliares, y confirmar el diagnóstico en el postoperatorio por colangiorresonancia magnética.
ConclusionesLa agenesia de la vesícula biliar es una malformación poco frecuente de la vía biliar y el cirujano debe sospechar esta entidad, o bien una variante anatómica, cuando una disección es difícil o bien durante la colecistectomía por laparoscopia en la que se requiere hacer uso de la colangiografía transoperatoria, sobre todo para prevenir una lesión de la vía biliar.
According to Beuran,1 gallbladder agenesis was reported for the first time in 1702 by Bergman, and since then, only 413 cases have been reported in medical literature world-wide. The rarity and low incidence of this condition is a reason for it to be published in a Mexican journal, as there are no more than 3 reported cases in Latin American medical journals.2–4 It is the least common congenital malformation of the bile duct. The average age at which it presents is 46. It has a prevalence of 0.007–0.13%, with a variation between surgical series and autopsy series. The female to male ratio is 2–3:1 and it is 40–65% associated with other congenital malformations, such as: xantomatosis cerebrotendinosa, Opitz syndrome, Klippel-Feil syndrome, amongst others.5 The malformation occurs during the third week of gestation, when the hepatic diverticular bud fails to develop as the gallbladder is being formed.6
We present a clinical case diagnosed with gallbladder agenesis during the intraoperative period; we also describe its management, and evolution and perform a review of medical literature.
Clinical caseA female patient, aged 62, from Monterrey, Nuevo León, attended the surgery with a 3-week history of moderately intense, colic-type abdominal pain in the right hypochondrium radiating to the ipsilateral back, which presented after intake of cholecystokinetics; no fever, jaundice, choluria or acholia. On physical examination: haemodynamically stable and afebrile. Abdomen: rounded abdomen due to the adipose panicle, peristalsis active, soft, palpable, not painful on palpation, with a negative Murphy's sign.
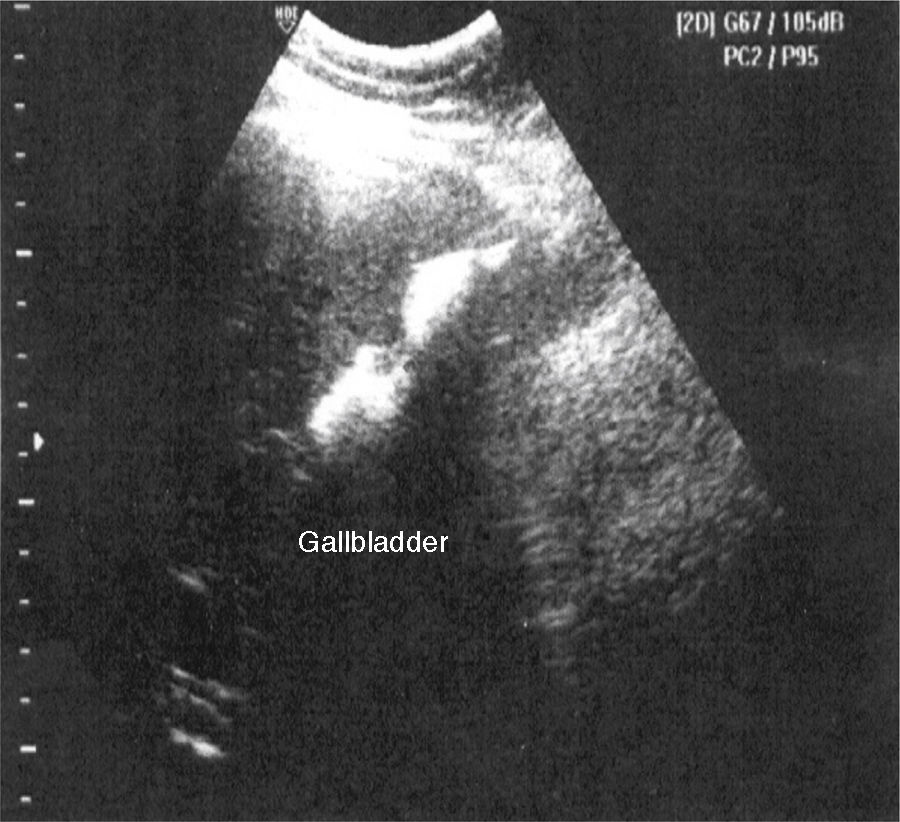
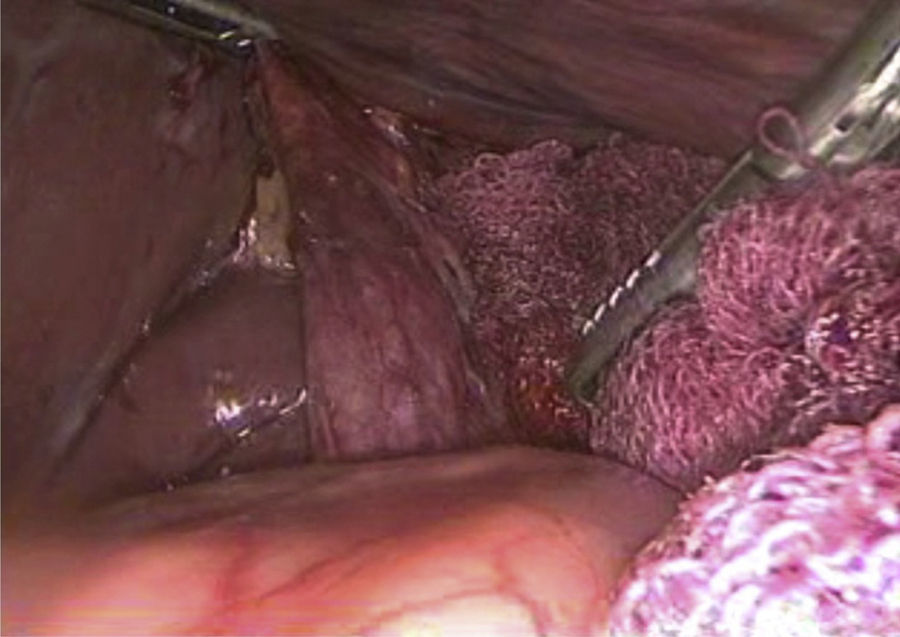
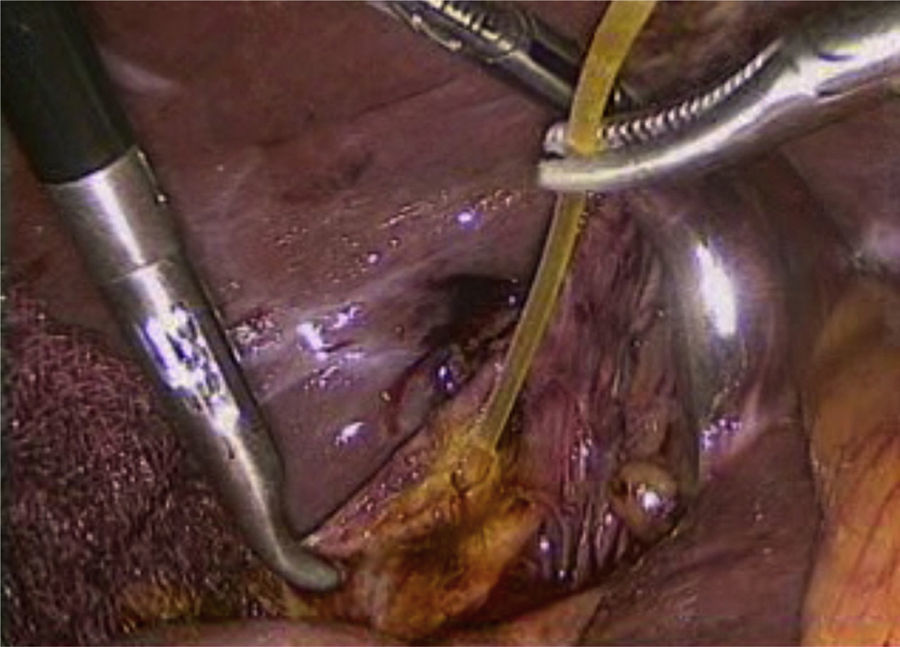
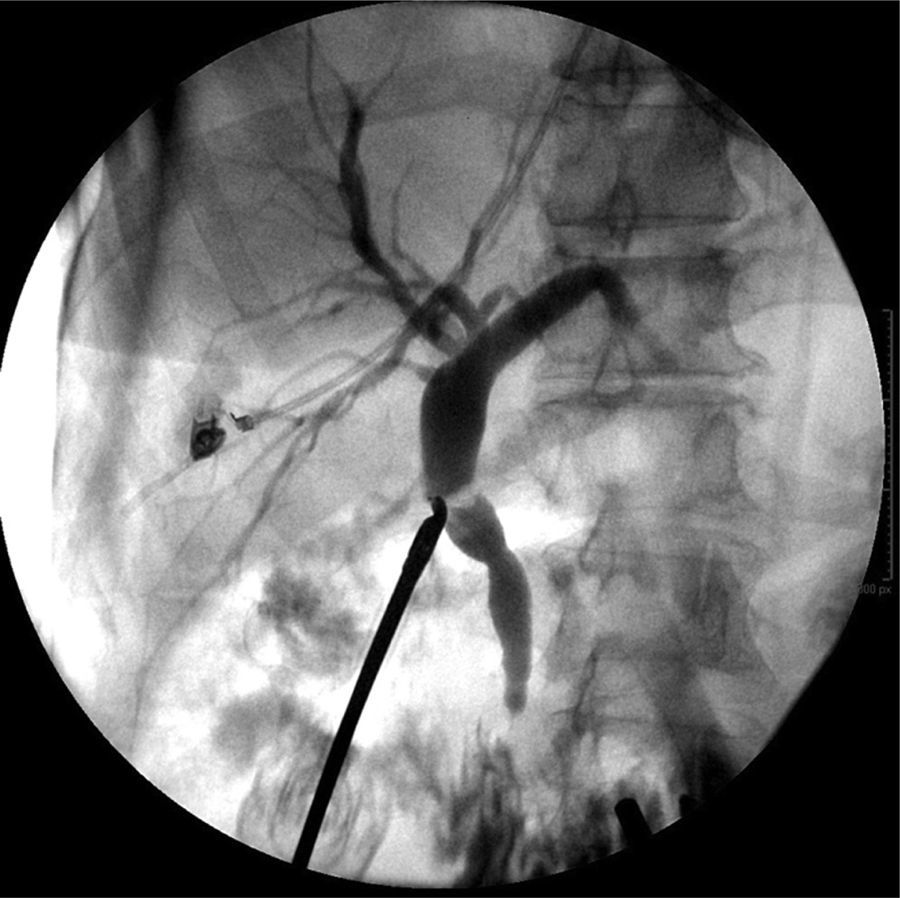
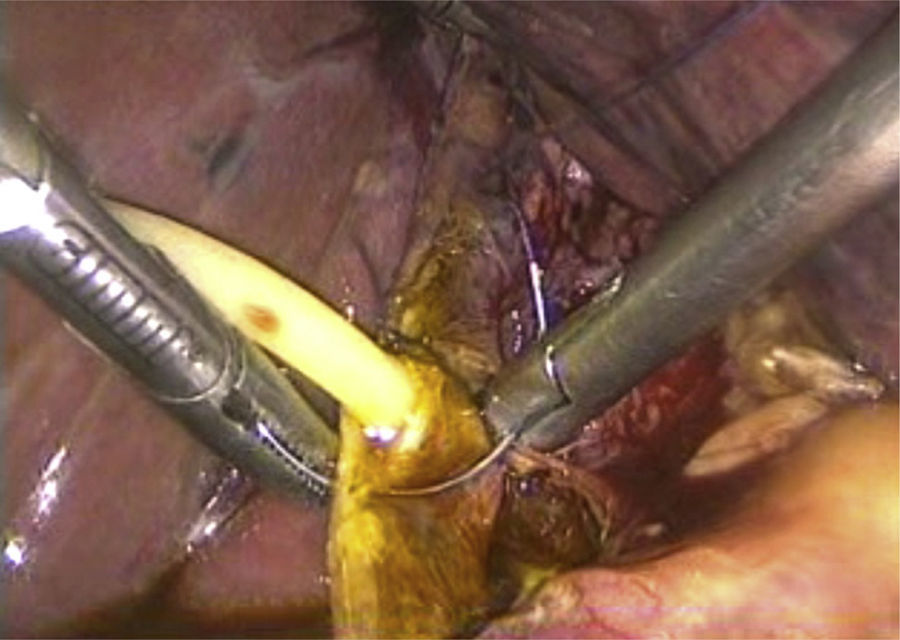
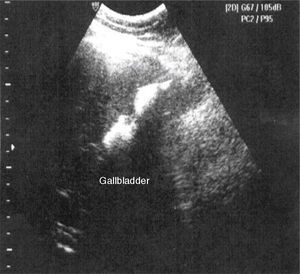
Laboratory tests were within normal parameters. An abdominal ultrasound was performed which reported a partially-assessable gallbladder due to the presence of multiple echogenic images, poorly defined in relation to stones, projecting a posterior acoustic shadow and impeding assessment of the wall; cholecystolithiasis was concluded (Fig. 1). The patient was scheduled for cholecystectomy by laparoscopy with a diagnosis of cholecystolithiasis. On dissection of what appeared to be the gallbladder, we observed the tubular shape of this structure (Fig. 2). An intraoperative cholangiography was performed (Fig. 3) which showed agenesis of the cystic duct and gallbladder, with adequate passage of contrast to the duodenum and no evidence of stones (Fig. 4). A search for the gallbladder was made throughout the abdomen without success. A #10 Fr T-tube was placed (Fig. 5) in the common bile duct and a #10 Fr Jackson-Pratt drain to the gallbladder bed.
The patient evolved favourably postoperatively, and there was no evidence of bile leakage through the Jackson-Pratt drain. The patient's condition improved, and she was discharged on the third day post surgery, with instructions for care of the T-tube. She was given an outpatient appointment to assess removal of the T-tube after 6 weeks.
DiscussionIt is estimated that 23% of patients with gallbladder agenesis present with symptoms that are typical of biliary colic.5 Of these patients, 90.1% will present typical colicky pain in the right hypochondrium, 66.3% with nausea and vomiting after food, 37% with dyspepsia and 27% choledocolithiasis.5 But, why do these symptoms present if there is no gallbladder? This is explained by the theory of biliary dyskinesia, to be specific: sphincter of Oddi dysfunction. It has been found in animals that gallbladder agenesis involves anomalies of the sphincter of Oddi. Similarly, it is well acknowledged that when a spasm of the sphincter of Oddi is induced, the symptoms of biliary colic are reproduced. The prevalence of choledocolithiasis and dilation of the common bile duct is greater in these patients as well, at 22% and 32% respectively, which affirms this theory.5
Pre-operative investigations have failed to identify patients with gallbladder agenesis. It is well known that ultrasound is the imaging technique of choice to assess the gallbladder; however, it is difficult when a report is given of a gallbladder which is small, sclero-atrophic (this is a histopathological diagnosis) or contracted over stones. In 1980, the WES triad was described in order to make a diagnosis of cholecystolithiasis in these types of gallbladders. WES is the acronym for “Wall, Echo and acoustic Shadow”; when the radiologists identifies these 3 components on an ultrasound of the gallbladder, sensitivity of 95% is estimated in making a diagnosis of cholecystolithiasis.7 However, the great majority of ultrasounds performed on patients with gallbladder agenesis report cholecystolithiasis. The explanation for this is that the radiologist can confuse the periportal tissue, the subhepatic peritoneal folds, the duodenum or calcified hepatic lesions with the WES triad, resulting in false positives.5 Gammagraphy and retrograde endoscopic cholangiopancreatography usually conclude obstructions of the cystic duct, and do not report gallbladder agenesis.5 Magnetic cholangioresonance is an effective method for assessing the bile duct, it is not invasive and it does not require contrast medium. Unfortunately it is expensive, and it does not replace the ultrasound as the first technique of choice for disorders of the gallbladder. Even so, it should be used to complement inconclusive ultrasounds.8 Peloponissios et al.5 in their bibliographic review from 1960 to 2003, specify that all but 2 cases reviewed were diagnosed intraoperatively or in the post-operative period. This is why “preoperative diagnosis is probably impossible”8 and is made intraoperatively or in the post-operative period in most cases.5 With a suspected diagnosis of gallbladder agenesis, in 1967 Frey proposed fulfilling certain criteria intraoperatively, which comprised checking for the absence of inflammatory signs or fibrosis in the gallbladder bed, converting to laparotomy and making a thorough search for an ectopic gallbladder with complete Kocherisation, making an intentional search intrahepatically and retrohepatically, and in the left hemiabdomen, between the 2 layers of the minor omentum, in the falciform ligament, retropancreatically, retroperitoneally, and in the anterior wall. If not found, an intraoperative cholangiograph should be performed with exploration of the bile duct, if the common bile duct is dilated more than 2cm or if there is choledocolithiasis.9
The current recommendation is that laparoscopy should be abandoned when there is a suspicion of gallbladder agenesis, above all to prevent injury to the bile ducts, and that diagnosis should be confirmed in the post-operative period by magnetic cholangioresonance.10 Thus Frey's criteria are met, in that extensive dissection is avoided, and the morbidity that this entails, intraoperative cholangiography, exploration of the bile ducts, and if choledocolithiasis is found, retrograde endoscopic cholangiopancreatography with sphincterotomy and stone extraction can be undertaken. Likewise, if the patient continues to have symptoms in the post-operative period, they can be managed medically using smooth muscle relaxants. If the biliary colic does not subside, a retrograde endoscopic cholangiopancreatography and sphincterotomy can be performed to relieve symptoms.9,11 According to the diagnostic and therapeutic flow chart proposed by Malde, if after preoperative investigations of the bile duct the radiologist reports an unidentified, contracted or sclero-atrophic gallbladder, a further radiological study should be requested depending on local availability: magnetic cholangioresonance, computed tomography, retrograde endoscopic or endoscopic ultrasound. If a diagnosis of gallbladder agenesis is confirmed using any of these studies, the conservative management described above should be offered. If diagnosis remains uncertain, Malde advocates repeating the imaging study when the acute episode has subsided.9
We recommend performing intraoperative cholangiography using the puncture technique, to be able to solve the diagnostic dilemma intraoperatively and rule out the presence of any other disorder which might require surgical treatment (for example: ectopic, intrahepatic gallbladder, choledocoliathisis). Although some authors decide not to do this,12 intraoperative cholangiography has low morbidity when it is undertaken appropriately using the puncture technique and laparoscopy, as in this case.
ConclusionGallbladder agenesis is the least common malformation of the bile duct. However, it is the surgeon who has to deal with this disorder intra-operatively, since as we mention above, all preoperative studies have failed to establish this diagnosis. The surgeon needs to take this disorder into account when encountering a “difficult dissection”, scleroatrophic gallbladder or anatomical variants when performing a laparoscopic cholecystectomy. Intraoperative cholangiography should be used to confirm diagnosis, treat or rule out disorders which require intervention, and above all to prevent injury to the bile tract.
Please cite this article as: Cavazos-García R, Díaz-Elizondo JA, Flores-Villalba E, Rodríguez-García HA. Agenesia de la vesícula biliar. Reporte de caso. Cir Cir. 2015;83:424–428.