Obesity is a public health problem, for which the prevalence has increased worldwide at an alarming rate, affecting 1.7billion people in the world.
ObjectiveTo describe the technique employed in incomplete penetration of gastric band where endoscopic management and/or primary closure is not feasible.
Material and methodsLaparoscopic removal of gastric band was performed in five patients with incomplete penetrance using Foley catheterization in the perforation site that could lead to the development of a gastro-cutaneous fistula.
Clinical casesThe cases presented include a leak that required surgical lavage with satisfactory outcome, and one patient developed stenosis 3 years after surgical management, which was resolved endoscopically. In all cases, the penetration site closed spontaneously.
DiscussionGastric band erosion has been reported in 3.4% of cases. The reason for inserting a catheter is to create a controlled gastro-cutaneous fistula, allowing spontaneous closure.
ConclusionsVarious techniques have been described: the totally endoscopic, hybrid techniques (endoscopic/laparoscopic) and completely laparoscopic. A technique is described here that is useful and successful in cases where the above-described treatments are not viable.
La obesidad es un problema de salud pública cuya prevalencia se ha incrementado a nivel mundial de forma alarmante, afectando a 1.7 billones de personas en el mundo.
ObjetivoDescribir la técnica empleada en penetración incompleta de banda gástrica cuyo manejo endoscópico o cierre primario no es viable.
Material y métodosSe realizó retiro laparoscópico de banda gástrica en 5 pacientes con penetración incompleta y colocación de sonda Foley en el sitio de perforación, favoreciendo el desarrollo de una fístula gastrocutánea.
Casos clínicosSe presentó una fuga que requirió lavado quirúrgico con evolución satisfactoria; un paciente desarrolló estenosis 3 años después del manejo quirúrgico, que se resolvió con dilatación endoscópica. En todos los casos se logró el cierre espontáneo del sitio de penetración.
DiscusiónLa erosión por banda gástrica se ha reportado en un 3.4%. El razonamiento de poner una sonda consiste en crear una fístula gastrocutánea controlada que permita el cierre espontáneo.
ConclusionesSe han descrito diversas técnicas: las totalmente endoscópicas, técnicas híbridas (endoscópicas/laparoscópicas) y totalmente laparoscópicas. Se describe una técnica que resulta útil y exitosa en casos en los que los tratamientos antes descritos no son viables.
Obesity is a public health problem whose prevalence has increased at an alarming rate, affecting 1.7 billion people world-wide, and is associated with premature mortality, chronic morbidity, increased health services, reduced quality of life and social stigmatisation. According to data from the Organisation for Economic Cooperation and Development (OECD), Mexico is the second country, after the USA, with the highest prevalence of obesity at 24.2% of the population.1 Bariatric surgery has proved safe and effective in managing obesity, and it has benefits in improving or resolving the associated comorbidities. Among the current surgical techniques, the gastric band is a procedure with low mortality (0.02%) and morbidity, because it is not very invasive, it is reversible, it enables the size of the stomach to be controlled and is a technique which is easy to perform.2 According to Needleman and Happel, it was described by Belachew in 1993. It gained popularity world-wide and became the most frequently performed bariatric surgery in Europe, Australia and Latin America. The FDA approved it in 2001.3 Reported results vary in terms of efficacy. One of the late gastric band complications reported is erosion or intragastric migration, with a reported incidence which varies from 0% to 5.8%, with an average of between 0.6% and 3%,4 but there are series such as that of Suter et al. which report an incidence of up to 9.5%.5 On average this occurs 12 months after fitting the band, and is associated with the technique used to fit it. The pars flaccid technique is currently recommended as it has a lower rate of erosion.6–8 The causes of erosion are not precisely known but the following have been considered: injury to the serosa during surgery by cautery or on fitting the device, sutures to the gastric wall, overfilling the band causing ischaemia, peptic ulcer, alcohol and smoking.9,10
Reported symptoms are: vague stomach ache, obstruction, insufficient weight loss, recurrent port infection,11 while another review mentions that the most common symptom is loss of satiety.12 Diagnosis in all cases is made by endoscopy.13 Although cases diagnosed with a contrasted oesophagogastric series have been reported, in which the material is seen inside the stomach, encircling part of the band.14
Treatment consists of removing the band, and there are different ways of doing so, and subsequent management, but there is no evidence that erosion, even when minor, will heal itself. Removal by endoscopy has been suggested,15 as long as the buckle of the band is in the stomach lumen, otherwise, it is performed by laparoscopy with omental patch.16 Although there are groups who report the placement of stents to force the gastric band with incomplete penetration to migrate towards the gastric lumen to then be removed by endoscopy, with a 66% success rate.17 There is also a group who report endoscopic management with opening of the stomach to release intra-abdominal adherences or with incomplete penetration. Other authors, including the author who originally proposed removing the band and primary closure,18 propose immediate rebanding in cases of gastric band erosion, if the gastric wall has incurred little damage from inflammatory response.19 Others propose a period of 4 months after removing the band as a reasonable time to attempt rebanding.20 And conversion to another procedure is indicated by some, who postulate that simply removing the band results in a reduction of weight loss or even weight gain.21,22
The gastric band mortality rate is low (0.05–0.4%), and even lower than 0.05–0.4%, lower than other bariatric surgery procedures.23 The most frequent causes of mortality, in a review by Gagner et al.24 with 9682 patients, are: pulmonary embolism, myocardial infarction, and gastric perforation. Most present within the first 30 days post surgery.
At present, there is no consensus on how to manage erosion, which always depends on transoperative findings; there is no mention in medical literature of the grade of localised inflammation in the gastric wall or the average diameters of erosion. We believe that a major reaction in the gastric wall implies difficulty in properly closing the wall and the risk of leakage into the abdominal cavity. Therefore, we consider it of interest to mention the use of gastrostomy for gastric band erosion in patients with major inflammatory reactions in the gastric wall, even when there is added infection, erosions of a considerable size and complications such as fistulae.
ObjectiveTo describe in detail the technique used by our bariatric surgery team in 5 patients who required removal of their gastric bands due to incomplete penetration with associated symptoms, and for whom the endoscopic option was not successful.
HypothesisPlacing a gastrostomy tube in the penetration site of the band enables the formation of a controlled gastro-cutaneous fistula which closes spontaneously.
Materials and methodsAll the patients were given a detailed explanation of the procedure to be performed and its possible complications. This was recorded in the patients’ records with the signed informed consent form.
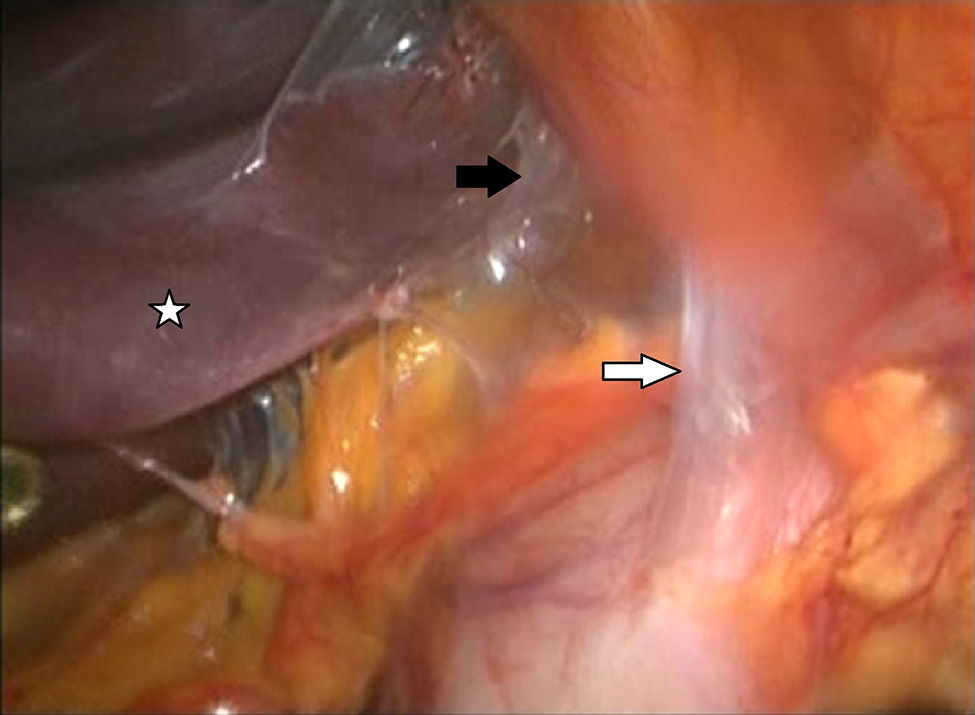
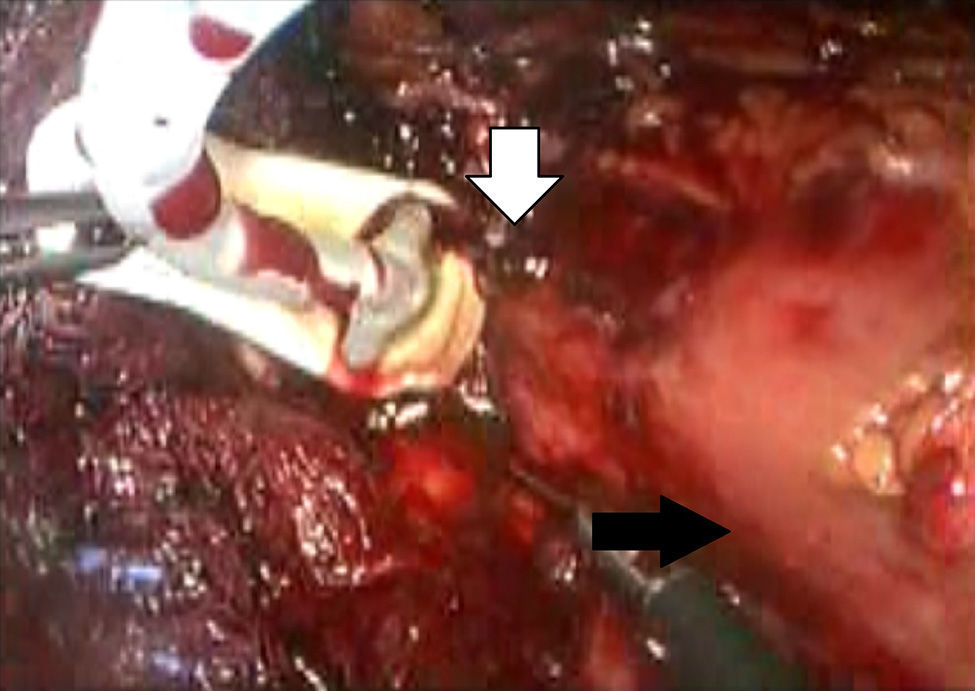
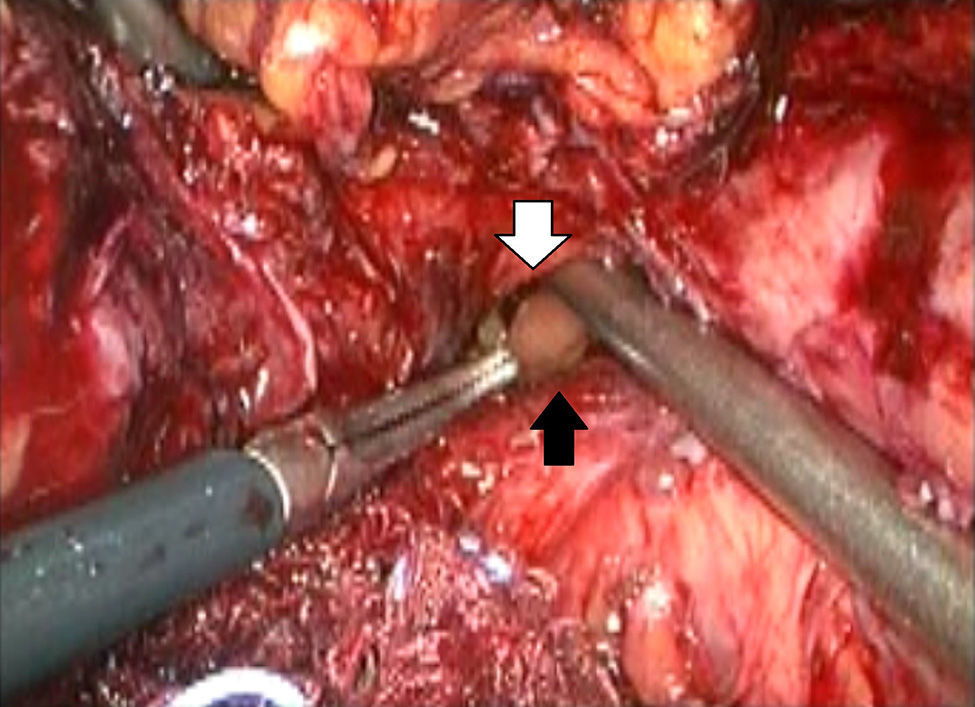
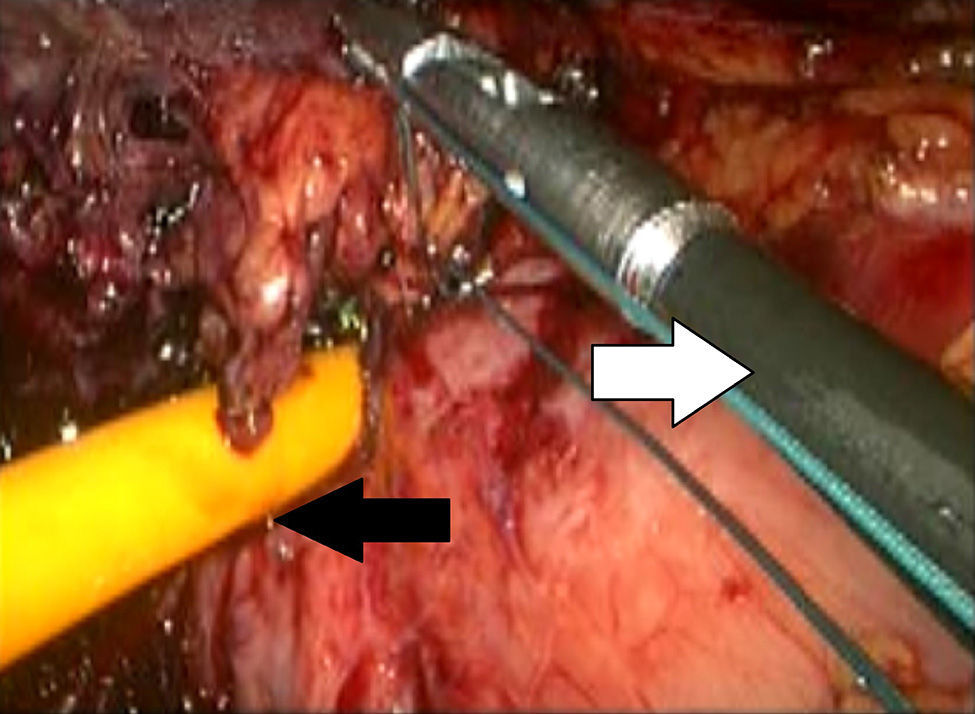
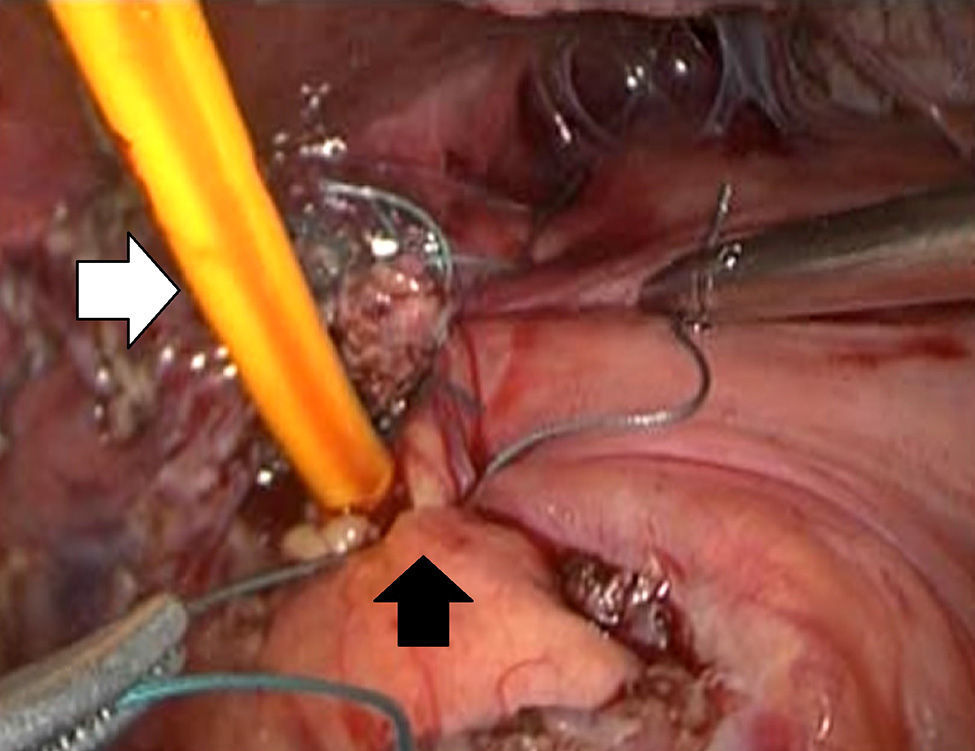
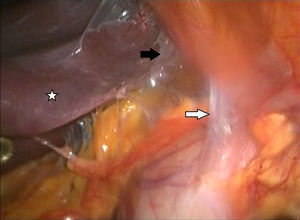
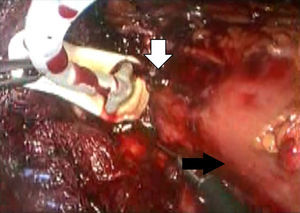
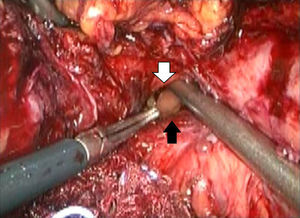
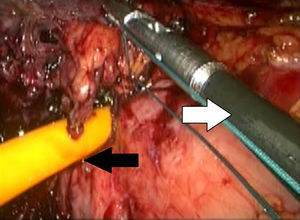
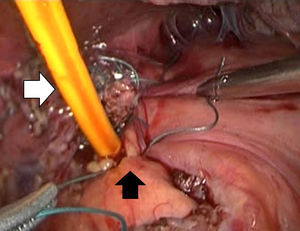
Description of the techniqueAfter endoscopic diagnosis of incomplete penetration of the band in the gastric chamber, it is removed by laparoscopy. 4 ports are used: one for the hepatic separator (5mm subxiphoid), a 10mm trocar in the left side, a 10mm supraumbilical trocar (vision 10mm 30° lens), a 5mm trocar in the right side. A diagnostic laparoscopy is performed, adherences from previous surgery are identified and released (Fig. 1) with a harmonic instrument, and the stitches securing the band are removed. Once it has been located, the buckle is released in order to remove the band (Fig. 2), on occasion cutting it with scissors, and it is removed ensuring that the buckle is the first part to be taken out. The connector which goes to the reservoir is cut off and removed through one of the ports. Subsequently the area of gastric erosion is located (Fig. 3), occasionally using methylene blue. Once the erosion has been located, a 21Fr Foley catheter is inserted and a purse string ligature (Fig. 4) made to adjust the catheter with the technique described for gastrostomy (Fig. 5). The balloon is inflated with 5mm of water and pulled until firm, there is no strain, and no visible leakage. The gastrostomy is exteriorised through the 5mm subxiphoid port; it is secured to the skin and a closed drain is left in the cavity, which is removed through the left port. The patient is discharged 72h later and restricted to a liquid diet for the first week, which is increased as tolerated. The drain is removed after 7 days if there is no evidence of leakage, and the gastrostomy catheter is removed 3–5 weeks later after fistulography with hydrosoluble contrast medium.
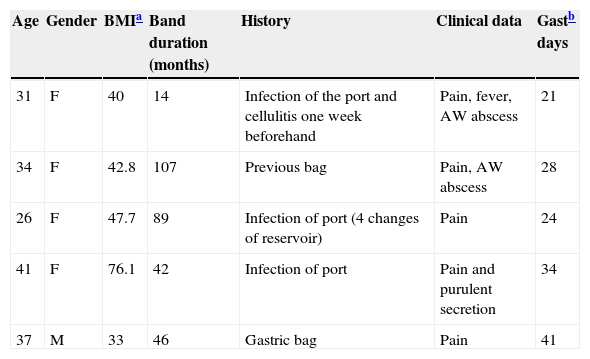
Four (80%) of the cases were female, and there was one (20%) male; 80% were morbidly obese with an average BMI of 47.92 (maximum 76.1, minimum 33). One of the patients had had the band for one year; the rest had had it for longer than 3 years. The penetration site of the band was in the minor curvature at the level of the oesophago-gastric union with an average diameter of 12mm. The average age was 33.8 (31–41). All the patients had symptoms of vague abdominal ache, occasionally located in the epigastrium; similarly, they all had a history of early problems with the band: 3 (60%) had had infections of the port, 2 (40%) with gastric bag and one patient developed a gastro-cutaneous fistula (Table 1).
Clinical data and history of the cases managed using the described technique.
| Age | Gender | BMIa | Band duration (months) | History | Clinical data | Gastb days |
|---|---|---|---|---|---|---|
| 31 | F | 40 | 14 | Infection of the port and cellulitis one week beforehand | Pain, fever, AW abscess | 21 |
| 34 | F | 42.8 | 107 | Previous bag | Pain, AW abscess | 28 |
| 26 | F | 47.7 | 89 | Infection of port (4 changes of reservoir) | Pain | 24 |
| 41 | F | 76.1 | 42 | Infection of port | Pain and purulent secretion | 34 |
| 37 | M | 33 | 46 | Gastric bag | Pain | 41 |
F: Female; Gast: gastrostomy; BMI: body mass index; M: male; AW: abdominal wall.
The patients were discharged stable and asymptomatic post surgery, the band was successfully removed laparoscopically in all of them. One patient presented with complications after the gastrostomy (leakage), which had to be resolved by surgical lavage, and fitting a closed drain with no further surgical treatment. The patient evolved favourably.
The average number of days with gastrostomy was 29.6 (21–41). There was one complication after removal of the gastrostomy, which required surgical drainage of an abscess 20 days post surgery; the patient subsequently evolved satisfactorily. One patient required dilatations as they developed stenosis in the gastric lumen 3 years post surgery, with satisfactory results.
During follow-up of the patients, using the technique described, morbidity was low despite the fact that the patients were experiencing severe inflammatory processes at the time that the band was removed, and therefore primary closure and omental patch were not feasible. All the patients presented closure of the perforation in an average of 29.6 days (maximum 41 days, minimum 21 days). One patient required laparotomy, removal of the catheter, and placement of a drain with no further surgery. Prior to removal of the gastrostomy tube, gastrography was performed on all the patients with water-soluble contrast medium to ensure medico-legal certainty and justification that there was no leakage. The 5 cases presented had an “American gastric band” of the brand Inamed/Allergan.
DiscussionThe causes of gastric band erosion are unknown. Continuous pressure on the area causing ischaemia and fibrosis have been reported amongst the numerous factors involved.25 Our group uses the pars flaccid technique, which is associated with fewer complications.26,27 The bands most often used are the SAGB and Lap Band. No significant difference has been demonstrated in the inflammatory reaction produced by either28 or in complications presented,29,30 despite the fact that one is high pressure, low volume (Lap Band) and the other is high volume, low pressure (SAGB). In terms of the erosion rate in patients with bands, in our group this is 2.6%, already reported in a previous article,2 although rates from 0.2%31 up to 32.65%7 are reported in medical literature. It is worth mentioning, in series such as that reported by O’Brien,32 that the erosion rate is 3.4% after follow-up of 17 years, very similar to that presented by the authors after almost 10 years. In another follow-up series after 9 years, only 53% of patients still had their original band, 17.8% had a new band, and 28.6% had their band removed, and their erosion rate was 20.5%, which occurs on average after 5 years.33
Of the cases reported in this article, only 2 were had their bands fitted by this team.
With regard to removal of the eroded band, the success rate to date is 100% with the technique employed. Although it is true that there is no consensus on the ideal way to manage erosion, there are groups who opt for completely endoscopic management.13,17 However not quite 100% of cases are successful due to the adherences that the device can present in the abdominal cavity, especially towards the liver. Others choose mixed endoscopic and laparoscopic management, and there are those who report endoscopic gastrostomy to release the adherences which occur around the device. Management by laparoscopic surgery has the advantage that it enables the band to be released and the extent of fibrosis generating in the erosion area to be assessed. The material we use is cheap and accessible, as a Foley catheter is used, which is available in practically any hospital in our country, and no additional costs are generated. The reasoning behind placing a catheter is the same as that behind making any gastrostomy: to encourage the development of a controlled gastro-cutaneous fistula which enables the subsequent removal of the catheter and spontaneous closure of the gastric fistula.
ConclusionsIn order to manage incomplete gastric penetration by gastric band, where endoscopic management is not feasible, and which also presents extensive fibrosis or infectious processes in the gastric wall which impede primary closure or omental patch, it is possible to remove the gastric band by laparoscopy and place a catheter in the area of penetration, causing a fistulous route with a good success rate, for spontaneous closure and resolution of this major complication presented by gastric bands.
Please cite this article as: Echaverry-Navarrete DJ, Maldonado-Vázquez A, Cortes-Romano P, Cabrera-Jardines R, Mondragón-Pinzón EE, Castillo-González FA. Banda gástrica penetrada. Una alternativa de tratamiento. Cir Cir. 2015;83:418–423.