The acute scrotum is an emergency. Testicular torsion represents approximately 25% of the causes. The annual incidence of testicular torsion is approximately 1/4000 persons under 25 years, with highest prevalence between 12 and 18 years old. It usually occurs without apparent cause, but it has been associated with anatomical, traumatic, and environmental factors, among others.
Clinical caseA male 15 year-old male, with no history of importance, was seen in the Emergency Department, presenting with a sudden and continuous pain in the left testicle. It was accompanied by a pain that radiated to the abdomen and left inguinal area, with nausea and vomiting of more than 12h onset. Doppler ultrasound showed changes suggestive of testicular torsion. Surgery was performed that showed findings of a necrotic left testicle with rotation of the spermatic cord of 360°. A left orchiectomy was performed.
ConclusionsTesticular torsion should always be considered one of the leading causes of acute scrotal pain. Delays in diagnosis should be avoided as this is directly related to the percentage of testicular salvage or loss.
El escroto agudo es una urgencia y la torsión testicular representa aproximadamente el 25% de las causas. La incidencia anual de torsión testicular es aproximadamente 1/4,000 menores de 25 años, con mayor prevalencia entre los 12 y 18 años de edad. Generalmente ocurre sin causa aparente; sin embargo, se han asociado factores anatómicos, traumáticos, ambientales, entre otros.
Caso clínicoAcude al servicio de urgencias un varón de 15 años de edad, sin antecedentes de importancia. Inició su padecimiento al presentar dolor súbito y continuo en testículo izquierdo, progresivo, con irradiación a la región abdominal e inguinal izquierda, acompañado de náuseas y vómitos, con más de 12 h de evolución a su llegada. El ultrasonido doppler reportó cambios sugestivos de torsión testicular, por lo cual, se realizó tratamiento quirúrgico. Los hallazgos fueron un testículo izquierdo necrótico, con rotación del cordón espermático de 360°, por lo cual se realizó orquiectomía izquierda.
ConclusiónLa torsión testicular siempre debe ser considerada como una de las causas principales de dolor escrotal agudo. Se deben evitar retrasos en el diagnóstico, ya que el retraso en su atención está directamente relacionado con el porcentaje de salvamento testicular y con su pérdida.
The acute scrotum is an emergency condition. It is defined as scrotal pain, oedema and reddening. Testicular torsion represents approximately 25% of cases. The annual incidence of testicular torsion is approximately 1/4000 persons under 25 years, with highest prevalence between 12 and 18 years old.1,2 In general there is no apparent causes, but several factors relating to the deformity have been described in “bell clapper testis”, where there is an abnormal adherence of the tunica vaginalis to the testicle, and this results in an increase in the mobility of the testicle inside the tunica vaginalis.3
Other associated factors are: the increase in testicular volume, testicular tumours, testicle with a horizontal position, a history of cryptorchidism, spermatic cord with a long intrascrotal section, high or proximal insertion of the tunica vaginalis to the spermatic cord, trauma and recent exercise. Environmental factors, such as low temperatures,4,5 have also been associated with testicular torsion.
ObjectiveTo highlight the importance of making the correct diagnosis and administering immediate treatment for this painful condition, since delay in diagnosis is directly related to testicular salvage or loss.
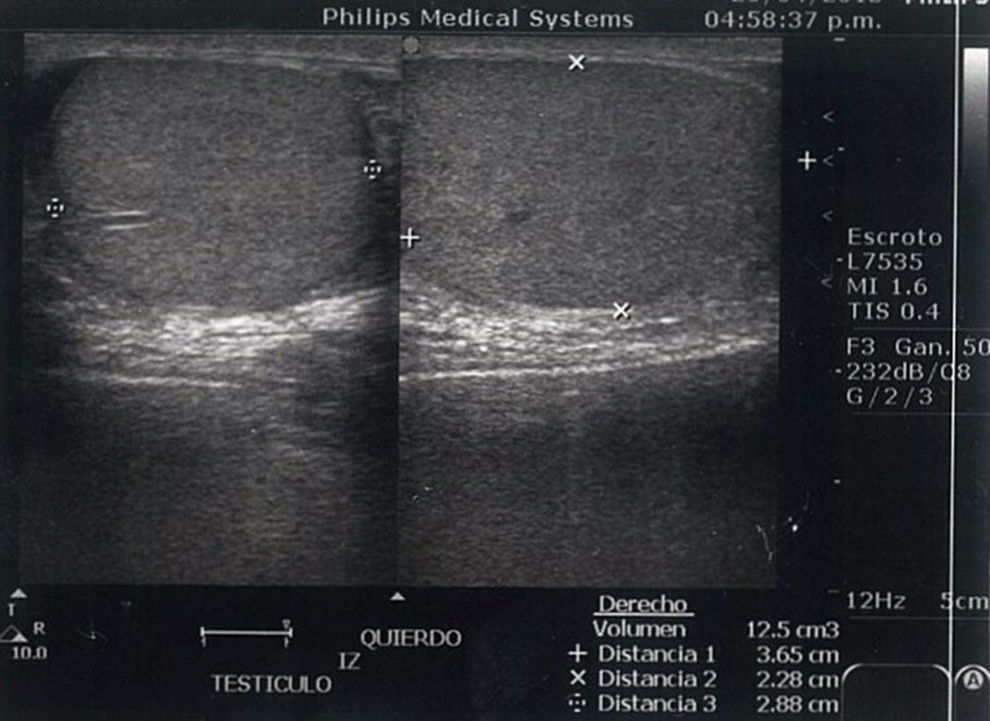
Clinical caseA 15 year-old male, with no history of importance, was admitted to the Emergency Department of the High Speciality Regional Hospital Dr. Gustavo A. Rovirosa Pérez, presenting with a sudden and continuous pain in the left testicle. The pain was progressive, accompanied by a pain that radiated to the abdomen and left inguinal area, with nausea and vomiting of more than 12h onset. On physical examination the left testicle was found to be larger in volume to the right one, was painful, local temperature had risen and there was a positive Prehn sign which helped to improve pain on raising the affected testicle. There was also an absence of the cremasteric reflex (Fig. 1).
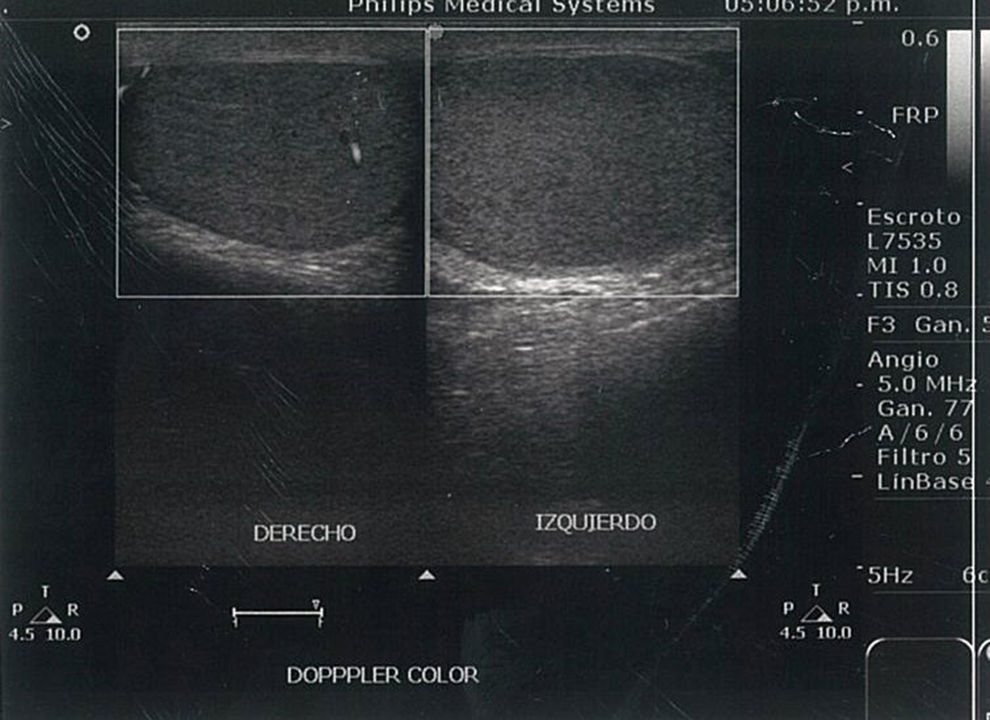
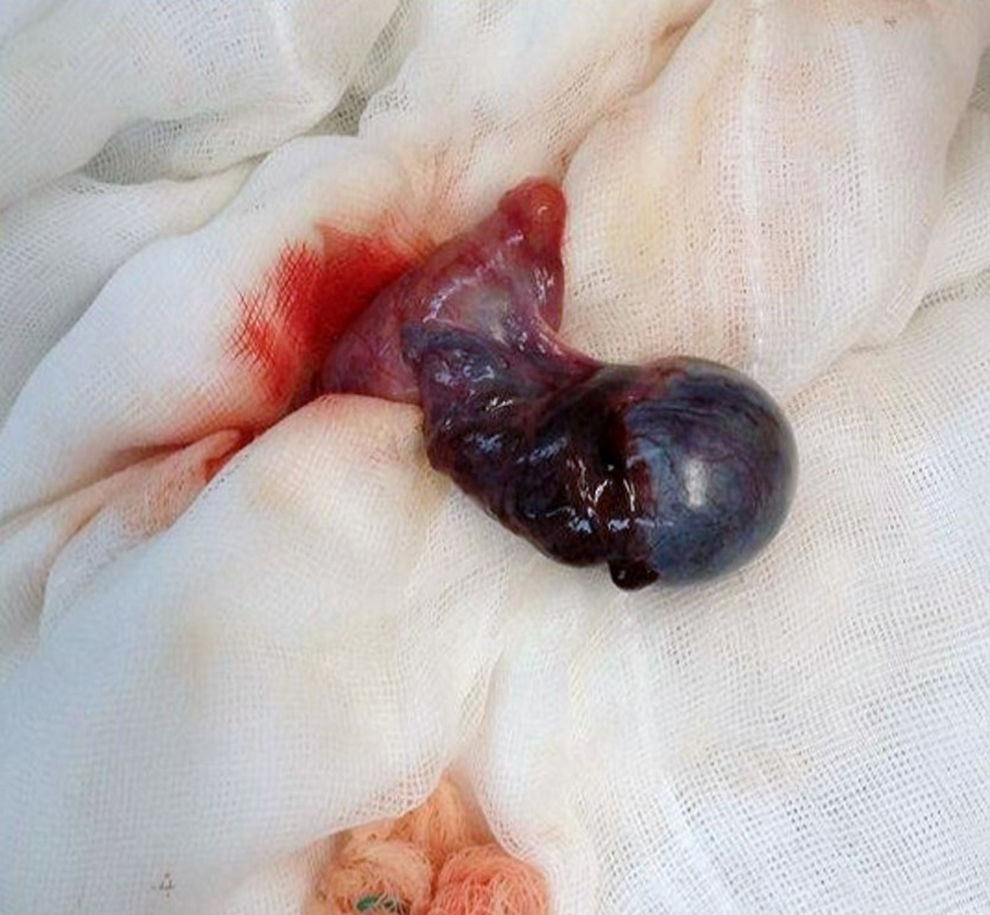
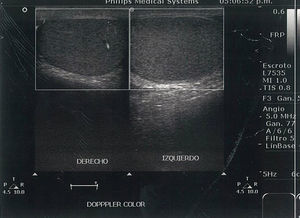
Lab tests were only performed for leukocytosis. Doppler ultrasound showed changes suggestive of testicular torsion (Figs. 1–3). Emergency surgery was performed the same day as admittance. This showed findings of a necrotic left testicle with a 360° rotation of the spermatic cord (Fig. 4), for which a left orchiectomy was performed. The pathology study reported haemorrhagic testicular infarction. There were no complications during convalescence and the patient was discharged the day after surgery.
The High Speciality Regional Hospital Dr. Gustavo A. Rovirosa Pérez is considered to be the emergency state centre in the State of Tabasco. The incidence of testicular torsion is low, with 2 cases annually and it is of vital importance to consider this diagnosis as one of the most common causes of acute scrotum, as it represents up to 25% of causes. Correct diagnosis is essential since its delay from the time of evolution from when symptoms begin to the search for medical attention and the time until surgical treatment is performed is directly related to the percentage of testicular recovery or salvage. If surgery is performed within the first 6h from when symptoms begin, there is up to 90% chance of recovery. This drops to 50% if it is after 12h and to 10% after 24h, as described by Davenport6 (Fig. 2).
Physical examination plays an important role in the diagnosis of testicular torsion. In a study involving 245 boys with acute scrotum, Rabinowitz et al.7 observed a 100% correlation between the presence of the cremasteric reflex and the absence of testicular torsion, and concluded that the presence of the cremasteric reflex is the most valuable clinical finding for ruling out testicular torsion whilst its absence increases suspected diagnosis. The imaging study used in our hospital for confirming diagnosis was the Doppler ultrasound, which has a 96.8% sensitivity, a 97.8% specificity, a positive predictive value of 92.3% and a negative predictive value of 99.1%. We therefore conclude that clinical assessment, combined with Doppler ultrasound is a reliable technique in the identification of testicular torsion.8 These two tools led us to diagnosis in the case presented here. If there is high suspicion of testicular torsion, despite the fact clinical history, physical examination and imaging studies are normal, we would recommend carrying out a surgical examination to avoid more significant complications such as the loss of the testicle.9 The outcome of the case we present was not one we would have wished for, since the patient presented at our hospital department with over 12h of symptom onset and lost the affected testicle. Some literature reports that the rate of orchiectomy in Mexico to be up to 95%, which is an extremely high figure.10 This is a reflection of high testicular loss in Mexico.
It is important to underline that this condition may also present in the perinatal period, which represents 12% of all testicular torsions in infancy. It is divided up into 2 main categories, one prenatal or intrauterine and one postnatal, where presentation is within the first month of life. The most appropriate management is still under controversy, but when suspicion exists it is recommended that immediate surgical treatment be carried out, since imaging studies have limitations in this age group. A surgical examination of the affected side is recommended and contralateral orchiopexy, due to the risk of presenting with contralateral asynchronic testicular torsion11,12 (Fig. 3).
ConclusionTesticular torsion should always be considered as one of the main causes of acute scrotal pain. Delayed diagnosis should be avoided and the patient should always be referred for a further level of treatment since its delay is directly related to the percentage of testicular salvage or loss (Fig. 4).
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Fernández G, Bravo-Hernández A, Bautista-Cruz R. Torsión testicular: reporte de un caso. Cirugía y Cirujanos. 2017;85:432–435.