Foreign body ingestion is the second cause of endoscopic emergency in the elderly, and dentures are the most frequent accidentally ingested objects. Once in the stomach, their expulsion can be expected in 4–6 days. The treatment is wait and see in asymptomatic patients, but preventive endoscopic removal can also be performed.
ObjectiveTo present 2 scenarios of the outcome and treatment in patients with foreign body ingestion.
Case reportPatient under study due to weight loss, with a denture detected by abdominal X-ray, ingested inadvertently a year ago. A laparotomy was required as extraction by colonoscopy failed, due to excessive inflammation. The second case, of 24-h onset, was due to the ingestion of a partial denture. As duodenal endoscopy extraction was unsuccessful, the patient was kept under observation. When it did not pass the caecum, it was extracted by colonoscopy, with no further complications and shorter hospital stay.
ConclusionsFollow-up can be by simple abdominal X-ray, with endoscopic management if there is insufficient progress. In one of our cases, the outcome was unfavourable due to time of ingestion, and endoscopic management was not possible, whereas in the second case colonoscopy was performed early with success. Proper diagnostic and timely treatment mark the difference in the progression and outcome of the ingestion of foreign bodies.
La ingestión de cuerpos extraños es la segunda causa de urgencia endoscópica en adultos mayores. Las prótesis dentales son los objetos más frecuentemente ingeridos de forma accidental. Una vez en el estómago, se puede esperar su expulsión de 4 a 6 días. El tratamiento es la conducta expectante en pacientes asintomáticos, pero puede hacerse la remoción preventiva endoscópica.
ObjetivoMostrar 2 panoramas distintos en la evolución y manejo endoscópico de la ingesta accidental de prótesis dental.
Caso clínicoPaciente estudiada por pérdida de peso. Se detectó en radiografía abdominal prótesis dental, ingerida inadvertidamente hace un año. Falló manejo con colonoscopia por intensa inflamación y requirió laparotomía para la extracción. Segundo caso, con 24 h de evolución de ingesta de prótesis dental, en un primer intento falló la extracción endoscópica del duodeno, se dejó a libre evolución y, al no progresar en el ciego, se realizó colonoscopia, extrayendo prótesis dental con éxito, sin complicaciones y con menor estancia intrahospitalaria.
ConclusionesEl seguimiento de la ingesta de prótesis dental puede ser con radiografías simples de abdomen; de no haber progresión, debe considerarse un manejo endoscópico. Uno de nuestros casos presentó desenlace desfavorable por el largo tiempo de evolución, sin que pudiese ser manejada endoscópicamente, mientras que la otra pudo ser manejada con colonoscopia. Una sospecha diagnóstica y un tratamiento oportuno pueden ser la diferencia en la evolución y resultado final de la ingesta de cuerpos extraños.
The ingestion of foreign bodies is the second cause of endoscopic emergencies in Spain.1 In older adults, the most frequent accidentally ingested objects are dental prostheses, particularly partial, removable dentures.2,3 Approximately 80–90% of ingested foreign bodies will pass through the entire digestive tract and be expelled rectally, without causing any problems.4
Foreign bodies can be classified as, (1) “food bolus” (fibrous poorly-chewed food), (2) blunt objects, (3) cutting or stabbing objects, (4) foreign bodies with a particularly dangerous content (drugs or batteries) and (5) medical material that has become dislodged (dental and enteric prostheses, retained endoscopy capsule, etc.).1 The clinical manifestations vary, and can include dysphagia and neck discomfort when the object is located in the oesophagus. Once it reaches the stomach it can take from 4 to 6 days to be expelled.5
Once ingestion has been established, the proposed management is wait and see, especially if there are no symptoms.2 The object would be expected to be expelled within approximately the following 48h.6 Preventive endoscopic removal is also possible in the likelihood of an obstruction.7 It is estimated that 76% of patients will require endoscopy and 16%, surgical intervention.5
The anatomic sites of obstruction in descending order are the upper oesophageal sphincter, the aortic arch and diaphragmatic hiatus. Once the object reaches the stomach it can continue to pass through to the ileocaecal region almost without difficulty.5 This is the area most commonly perforated, which is reported in up to 75% of cases. In addition to narrow areas, areas of angulation or retrovesical pouches, they can also lodge in flange areas or surgical anastomotic openings.8
Dentures cannot replace real teeth and compromise the discriminatory tactile sensitivity of the oral cavity,1 and can be inadvertently ingested. Management of this situation, although similar, can have a different outcome. Therefore we compared the clinical presentation, management and outcome of 2 cases of ingestion of a dental prosthesis.
ObjectiveOur aim was to show 2 different scenarios in terms of outcome and the endoscopic management of accidental ingestion of a dental prosthesis.
Clinical casesA retrospective revision was carried out from 2014 of 2 patients admitted to the General Surgery Department of the Hospital Central Norte de Petróleos Mexicanos, diagnosed with accidental ingestion of a foreign body (denture) and managed with the support of the gastroenterology and proctology Departments.
Case 1A 61-year-old woman, with a history of cystopexia and hysterectomy more than 20 years earlier, under medical follow-up for episodes of diarrhoea, involuntary weight loss and haematochezia on one occasion and abdominal pain, presenting sporadic episodes of fever. The patient was under study due to stenosis of the sigmoid colon with colonoscopy and biopsies, which reported chronic follicular inflammation. The study continued for 9 months. Abdominal tomography only reported diverticulosis and interference in the colon caused by foreign bodies was visualised (Fig. 1) when the initial barium X-ray of the colon found a radiopaque image compatible with a foreign body in addition to diverticulosis (Fig. 2). When the patient was interviewed again, she mentioned losing a denture, without having noticed that she had ingested it. Clinically her vital signs were stable; she was asymptomatic and her blood count was within normal parameters. She was hospitalised for removal of the foreign body by colonoscopy which found a dental prosthesis lodged at both ends towards the sigmoid mucosa approximately 28cm from the anal margin. It was not possible to remove the denture and therefore an exploratory laparotomy with sigmoidostomy was performed and repair of the sigmoid colon with closure on 2 planes. The patient made torpid progress with fever and intestinal loss through the drain. She was reoperated and a perforation was found on the posterior face of the sigmoid colon, the closure was intact. The laboratory report concluded acute diverticulitis with perforation. A sigmoidectomy and descending colostomy were performed. The patient progressed satisfactorily and was discharged with a surgical plan for intestinal anastomosis.
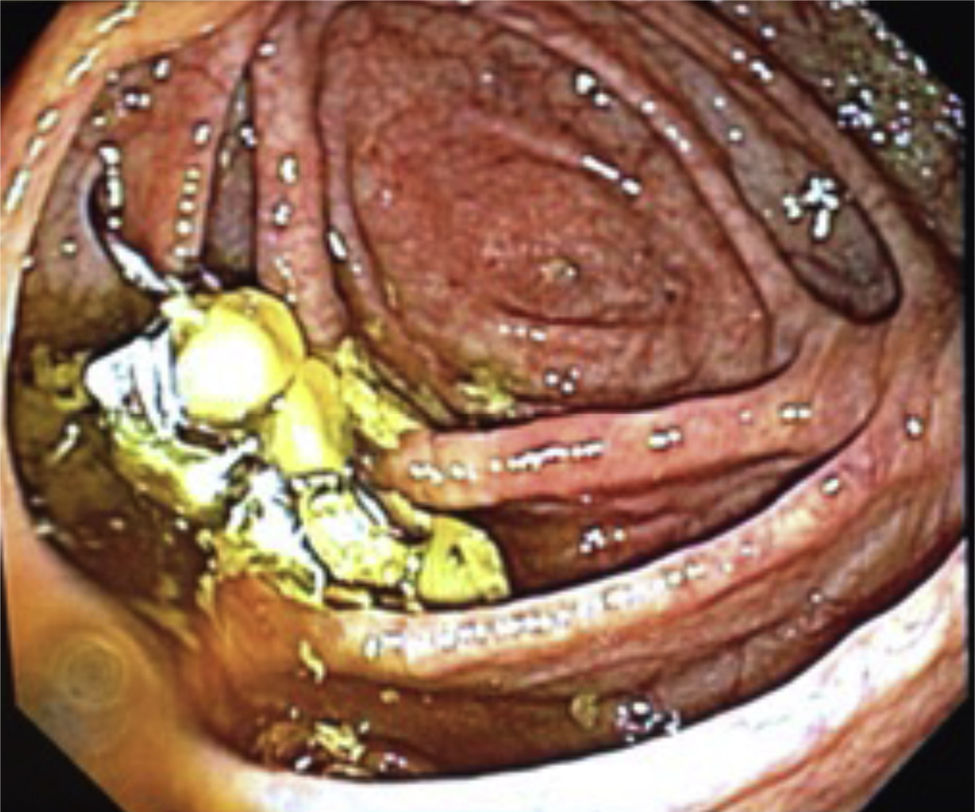
A 62-year-old woman, with a history of high blood pressure, hysterectomy and left inguinal hernioplasty more than 20 years previously, attended the emergency department 5h after accidentally ingesting a denture. On admission she presented dysphagia with no clinical disorders on physical examination or blood count, and her vital signs were stable. An endoscopy was performed that reported a foreign body (metal dental bridge) in the third duodenal portion. Extraction failed because one of the edges had lodged in the duodenal bulb and, on attempting to pick it up, it advanced beyond the third portion of the duodenum, and could not be visualised again. The patient was followed up with serial X-rays that showed how the denture was advancing. On the third day it was located in the right lower quadrant and had not moved (Figs. 3 and 4). Therefore the patient was prepared for colonoscopy which was performed successfully. A dental prosthesis in the caecum with 2 proximal and 2 distal hooks was reported and removed with polypectomy forceps under direct vision (Figs. 5 and 6).
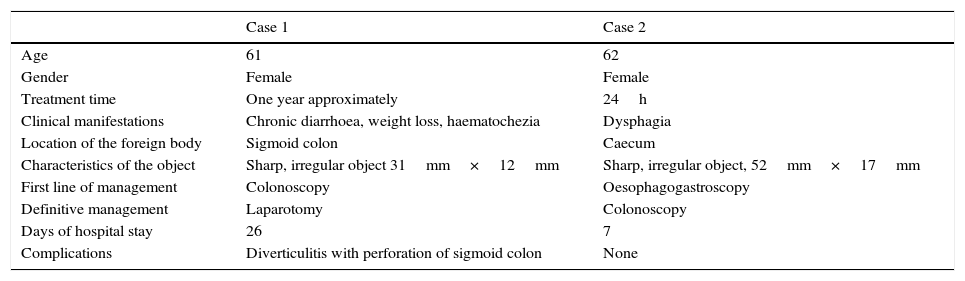
Both patients were assessed with abdominal X-rays. Endoscopic extraction was the first line of management for both of the patients. In the first case by colonoscopy, which proved impossible due to the time since ingestion and the intense inflammation of the mucosa, and because the prosthesis had become lodged. In the second case by oesophagogastroscopy, however extraction was impossible because the prosthesis had become lodged in the walls of the duodenal bulb. Finally, in the first case a laparotomy with sigmoidotomy, extraction of the prosthesis and closure on two planes were performed. In the second case removal was by colonoscopy, with no complications and therefore a shorter hospital stay. Curiously, the ingestion coincided with a picture of diverticulitis in the first patient which complicated the outcome (Table 1).
Comparison of cases of accidental dental prosthesis ingestion.
| Case 1 | Case 2 | |
|---|---|---|
| Age | 61 | 62 |
| Gender | Female | Female |
| Treatment time | One year approximately | 24h |
| Clinical manifestations | Chronic diarrhoea, weight loss, haematochezia | Dysphagia |
| Location of the foreign body | Sigmoid colon | Caecum |
| Characteristics of the object | Sharp, irregular object 31mm×12mm | Sharp, irregular object, 52mm×17mm |
| First line of management | Colonoscopy | Oesophagogastroscopy |
| Definitive management | Laparotomy | Colonoscopy |
| Days of hospital stay | 26 | 7 |
| Complications | Diverticulitis with perforation of sigmoid colon | None |
Follow-up of patients after ingestion of a foreign body, in this case a dental prosthesis, should be undertaken with serial plain abdominal X-rays9 and, if there is no progression, endoscopic management should be considered (colonoscopy or oesophagogastroscopy) if possible. The indications for emergency endoscopy after ingestion of a foreign body detected in the oesophagus are ingestion of batteries, obvious oesophageal obstruction and the ingestion of a sharp object, since complications of up to 35% have been reported. For the endoscopic extraction of sharp objects, such as dental prostheses in the stomach, an endoscopic cover should be used, to prevent tears.5,10 Colonoscopy is an important tool in managing foreign bodies in the colon. However there can be complications such as massive haemorrhage and intestinal perforation.9 Surgery should be considered if the object has not advanced from the oesophagus after 3 consecutive days or if there are symptoms of abdominal pain, vomiting, fever or melaena.5
The perforation that occurred after removing the dental prosthesis was caused by the diverticulitis, added to the chronic inflammation caused by the dental prosthesis. For this reason appropriate treatment needs to be given to avoid oedema of the mucosa with subsequent micronecrosis and perforation.11
In cases of ingestion of a foreign body, the type of object, its clinical presentation and above all, the time since ingestion need to be considered in order to prescribe treatment. In the 11 year revision by Park et al.12 there was no relationship between the form, location and endoscopic complications presented. They report an endoscopic removal success rate of 92.5%, up to 94.7% in other series13 and the main risk factor detected was the time since ingestion,12 as we found in our case. Manifestations can vary from remaining asymptomatic for a long period of time to presenting diffuse low intestinal symptoms, which can lead to a suspicion of different diagnoses.14,15 In an intestinal obstruction with a foreign body, neoplasms should be considered a likelihood, due to the advanced age of the patients and the unusual behaviour in not expelling the object spontaneously.16 Patients should be intentionally asked for any history of wearing dentures, symptoms of diarrhoea, fever, intermittent haematochezia, since as we show, our patient was unaware of the ingestion and only reported the loss of a dental prosthesis which she did not associate with her condition.
ConclusionsWe suggest that, as soon as a diagnosis of an accidentally ingested dental prosthesis has been made, and if it is accessible to high or low endoscopy, an attempt should be made to remove it to prevent subsequent complications or the complications inherent to open surgery. But open surgery must always be kept as the first therapeutic option, if there has been prolonged time since ingestion (more than 6 days without the object being expelled), and signs of obstruction, systemic inflammatory response or pain. Risk factors for conversion to open surgery include: patients aged over 70 years, higher location in the oesophagus, large sized foreign body and longer time since ingestion of the object.13 Diagnostic suspicion and prompt treatment, by endoscopy or surgery and strict follow-up can mark the difference in terms of progress and outcome after ingestion of a foreign body.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interest to report.
We would like to thank the colonoscopy department of the Hospital Central Norte de Petróleos Mexicanos for their collaboration.
Please cite this article as: Santander-Flores SA, Mata-Quintero CJ, O’Farrill-Anzures R, González-Villegas P, Calvo-Vázquez I, Campos-Serna EI. Ingestión accidental de prótesis dental, 2 panoramas en el manejo y evolución. Reporte de casos. Cir Cir. 2017;85:350–355.