In recent years, several publications have shown that new adhesives and sealants, like Tissucol®, applied in thyroid space reduce local complications after thyroidectomies.
Study aimsTo demonstrate the effectiveness of fibrin glue Tissucol® in reducing the post-operative hospital stay of patients operated on for differentiated thyroid carcinoma in which total thyroidectomy with central and unilateral node neck dissection was performed (due to the debit drains decrease), with consequent cost savings.
Material and methodsA prospective randomised study was conducted during the period between May 2009 and October 2013 on patients with differentiated thyroid carcinoma with cervical nodal metastases, and subjected to elective surgery. Two groups were formed: one in which Tissucol® was used (case group) and another where it was not used (control group). Patients were operated on by surgeons specifically dedicated to endocrine surgical pathology, using the same surgical technique in all cases.
ResultsA total of 60 total thyroidectomies with lymph node dissection were performed, with 30 patients in the case group, and 30 patients in control group. No statistically significant differences were observed in most of the studied variables. However, the case group had a shorter hospital stay than the control group with a statistically significant difference (p<0.05).
ConclusionImplementation of Tissucol® has statistically and significantly reduced the hospital stay of patients undergoing total thyroidectomy with neck dissection, which represents a significant reduction in hospital costs. This decrease in hospital stay has no influence on the occurrence of major complications related to the intervention.
En los últimos años han aparecido diferentes publicaciones que demuestran que los nuevos sellantes adhesivos, como Tissucol®, que son aplicados en el espacio tiroideo reducen las complicaciones locales tras tiroidectomías complejas.
ObjetivosMostrar la eficacia del adhesivo de fibrina Tissucol® en la reducción de la estancia hospitalaria postoperatoria de los pacientes intervenidos de carcinoma diferenciado de tiroides en quienes se realizó tiroidectomía total con vaciamiento ganglionar central y unilateral.
Material y métodosRealizamos un estudio prospectivo y aleatorizado, durante el periodo comprendido entre mayo de 2009 y octubre de 2013, en pacientes con carcinoma diferenciado de tiroides con metástasis ganglionares cervicales, para la realización de cirugía programada. Se formaron 2 grupos: en los que se utilizó Tissucol® (grupo caso) y en los que no (grupo control). Los pacientes fueron operados por cirujanos especialmente dedicados a patología quirúrgica endocrina, utilizando la misma técnica en todos ellos.
ResultadosRealizamos 60 tiroidectomías totales con vaciamiento ganglionar: 30 en el grupo caso, que se compararon con 30 del grupo control. No observamos diferencias significativas en la mayoría de las variables estudiadas; no obstante, el grupo caso presentó una menor estancia hospitalaria respecto al grupo control, con una diferencia estadísticamente significativa (p<0.05).
ConclusiónLa aplicación del Tissucol® ha permitido reducir la estancia hospitalaria de los pacientes operados de tiroidectomía total con vaciamiento cervical, lo que representa para el hospital una reducción de costos, sin que ello influya en la aparición de complicaciones relacionadas con la intervención.
The incidence of differentiated thyroid cancer is increasing worldwide (0.3–8.1 new cases/100,000 inhabitants per year), and represents 90% of endocrine tumours.1–4 As we know, the initial therapeutic approach for differentiated thyroid cancer is total thyroidectomy.5–8 In the case of advanced papillary carcinoma, the American Thyroid Association (ATA) also recommends performing a prophylactic lymphadenectomy of the central compartment of the neck,7,9,10 as this is the first step of lymphatic drainage and, if necessary, therapeutic lymphadenectomy of the lateral cervical compartment. Therefore it is important to mention that the thyroid is in a site where complications can present as feared as recurrent lesion, definitive hypoparathyroidism and, of course, haemorrhage, asphyxiating haematoma and seroma. With regard to these latter events, some surgeons advocate systematically placing drains in the wound.11 However, there are arguments against the use of drains, as they often become blocked with coagulated blood, and even when they are in place collections of blood or tissue fluid can form.12–15 Furthermore, placing drains implies a more lengthy hospital stay and can even increase the likelihood of infection and pain.15,16 In recent years various publications have demonstrated that the new haemostatic agents and adhesive sealants (which include Tissucol Duo®) can reduce local complications after thyroidectomy and hemithyroidectomy when applied in the thyroid space,17–28 associated with decreased drainage debit and reduction of dead space. Fibrin adhesives such as Tissucol Duo® also promote wound healing, stimulating the microphages and fibroblasts, thus promoting homeostasis and angiogenesis.21
The main objective of this work was to demonstrate the efficacy of the Tissucol® fibrin glue in reducing the postoperative hospital stay of patients operated for differentiated thyroid carcinoma who have undergone total thyroidectomy with central and unilateral lymph node emptying.
Our secondary objective was to demonstrate a reduction in local complications.
Material and methodsA prospective, randomised study was performed, of cases and controls, of adult patients referred to the General and Endocrine Unit of Barcelona's Hospital Clínic with a diagnosis of differentiated thyroid carcinoma with cervical lymph node metastases, for total thyroidectomy with central and unilateral lymph node emptying. The study was performed between 4 May 2009 and 31 October 2013.
The diagnosis of differentiated thyroid carcinoma was based on each patient's history and clinical examination, with complementary examinations using laboratory studies, chest X-ray and cervical ultrasound.
The criteria for inclusion in the study were: no medical anaesthesia contraindications (ASA), body mass index (BMI)<30, with no contraindications for Tissucol Duo® fibrin adhesives.
All the patients were operated by the same team: 2 surgeons specialists in cervical endocrine disorders with experience of more than 1000 cases. Demographic variables were collected (age, sex, BMI) and the clinical characteristics of the patients (date of admission, date of discharge, surgery time, length of incision, the anatomopathological type of the tumour, intraoperative complications, wound haematoma, seroma, postoperative pain (visual analogue scale 0–10), hypocalcaemia (serum calcium <8mg/dl) transient dysphonia and hospital stay) following the Clinical Guidelines for Endocrine Surgery of the Spanish Association of Surgeons, and the average cost of hospital stay per day (in euros).
A total of 60 consecutive patients were included in the study who had undergone total thyroidectomy with central and unilateral lymph node emptying.
The sample size of each group was calculated based on the criteria for comparison of means in a significance test, with safety level (0.05), power of the trial (95%), variance of the quantitative variable of the control group (4.35 according to previous references),14 minimum value of the difference to be detected.
Randomisation was by numbered sealed envelopes which were opened just before the incision was closed and the Tissucol® fibrin glue applied to the patients in the case group. Postoperative follow-up was blind for the evaluators.
Tissucol® fibrin glue (Baxter, Hyland Inmuno Reg. No.: 60426 and 60427 of the Spanish Medicines Agency. Kit used for wounds in general) was used in the case group without spraying over the surgical bed (Baxter, Hyland Inmuno).
The study was evaluated and tested by the Research Committee, the Ethical Committee and the Management of the Surgical Ward of our institution. The patients received informed consent forms which were signed at the visit to the clinic, prior to being entered on the waiting list for surgery. All the patients were informed of the possibility of other therapeutic options.
Once the information had been gathered, a descriptive analysis of the variables was made (mean, median, standard deviation).
The same surgical technique and the same preoperative protocol were used in all the patients.
Pain was controlled with the usual analgesic regimen (paracetamol+Enantyum® alternated every 8h).
Surgical techniqueThe surgeon stood on the right side of the patient with their assistant opposite. A transversal cervical incision was made 2cm from the sternal notch, from 5cm to 8cm long (depending on whether or not central, latero-cervical lymph node emptying was required). The external limits were marked by the posterior edge of the sternocleidomastoid muscle (Fig. 1). Then the planes were opened with the creation of upper and lower myocutaneous flaps, section of the midline of the deep cervical fascia and separation of the infrahyoid musculature, to expose both thyroid lobes, with systematic partial section of the sternothyroid muscle at the level of its insertion into the thyroid cartilage. Then the upper pedicle was sealed and sectioned, close to the thyroid surface, to prevent injury to the external branch of the upper laryngeal nerve. The parathyroid glands were identified and preserved. The recurrent laryngeal nerve was identified below its intersection with the lower thyroid artery. Resection of the corresponding lobule was completed, separating it from the traquea, and the same manoeuvres performed on the contralateral lobule until the total thyroidectomy was completed.
When the thyroidectomy was completed, we performed central, bilateral lymph node emptying of the neck or level vi and we associated functional therapeutic laterocervical lymph node emptying or levels IIA–IIB–III–IV on the side of the tumour, as described in the guidelines of the Spanish Association of Surgeons, after confirming the presence of pathological lymph nodes by ultrasound and/or finding them intraoperatively (Fig. 2). The entire operation was performed with the help of Ligasure Precise®. Finally, the haemostasis of the thyroid cell and laterocervical spaces was checked.
A Redon No.8 type suction drain was placed in all cases in the corresponding laterocervical vascular space. Then 2–4ml of Tissucol® (Baxter, Hyland Inmuno) fibrin glue were applied without spraying over the surgical bed in the case group (Fig. 3) (Baxter, Hyland Inmuno (Baxter, Hyland Inmuno. Reg. No. Reg.: 60426 and 60427) of the Spanish Medicines Agency Kit used for wounds in general).
In the post-operative period, following the protocol established in our unit, the criteria to remove the drain was when the debit was ≤20ml/24h and serous in appearance, for both the case group and the control group, and when the patient was taking a normal diet. All the patients were discharged from hospital after the surgical drain was removed.
Statistical analysisFirst a data validation, an analysis of consistency and of missing values or possible erroneous data was performed.
A variance analysis test (ANOVA) was performed in order to analyse the continuous variables or a non-parametric test (Wilcoxon) if the criteria for applying the ANOVA test were not met. A chi-squared test was used to analyse the categorical variables or Fisher's exact test if the criteria for applying the Chi-square test were not met. The T-test was used to compare means for 2 related samples. SPSS 20.0 software was used for the statistical analysis. The statistical analysis was performed with a 95% confidence level.
ResultsA total of 60 patients were included. We performed 30 thyroidectomies+central emptying+unilateral laterocervical emptying, applying Tissucol® fibrin glue (case group) and we compared them with 30 patients where Tissucol® fibrin glue was not applied (control group). The intervention was successfully completed in all patients. They were all classified as ASA I–II.
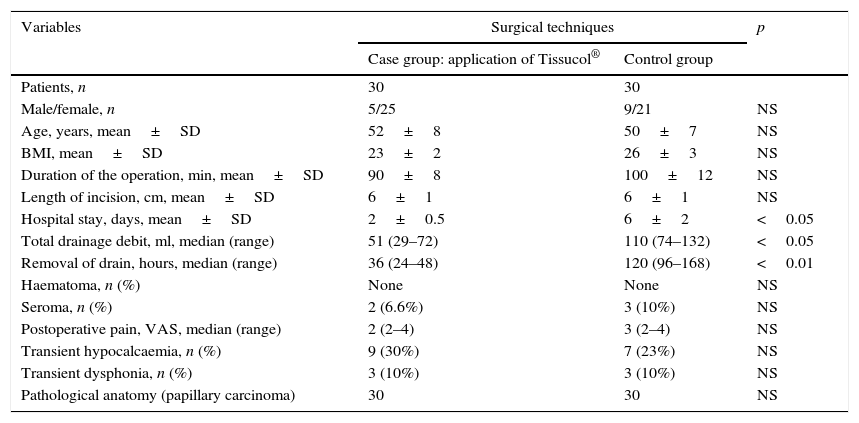
Most of the patients were female (46 women, 14 men). The mean age of the series was 50±8. No statistically significant differences were observed between the study groups. The mean surgery time of the total thyroidectomy+central lymph node emptying+unilateral lateral lymph node emptying was slightly less in the case group, without the difference being statistically significant (Table 1). No intraoperative complications were detected.
Comparison of the clinicopathological variables between the groups.
| Variables | Surgical techniques | p | |
|---|---|---|---|
| Case group: application of Tissucol® | Control group | ||
| Patients, n | 30 | 30 | |
| Male/female, n | 5/25 | 9/21 | NS |
| Age, years, mean±SD | 52±8 | 50±7 | NS |
| BMI, mean±SD | 23±2 | 26±3 | NS |
| Duration of the operation, min, mean±SD | 90±8 | 100±12 | NS |
| Length of incision, cm, mean±SD | 6±1 | 6±1 | NS |
| Hospital stay, days, mean±SD | 2±0.5 | 6±2 | <0.05 |
| Total drainage debit, ml, median (range) | 51 (29–72) | 110 (74–132) | <0.05 |
| Removal of drain, hours, median (range) | 36 (24–48) | 120 (96–168) | <0.01 |
| Haematoma, n (%) | None | None | NS |
| Seroma, n (%) | 2 (6.6%) | 3 (10%) | NS |
| Postoperative pain, VAS, median (range) | 2 (2–4) | 3 (2–4) | NS |
| Transient hypocalcaemia, n (%) | 9 (30%) | 7 (23%) | NS |
| Transient dysphonia, n (%) | 3 (10%) | 3 (10%) | NS |
| Pathological anatomy (papillary carcinoma) | 30 | 30 | NS |
cm: centimetres; SD: standard deviation; VAS: visual analogue scale; BMI: body mass index; min: minutes; ml: millilitres; n: number.
With regard to the days of hospitalisation, the mean stay was 2±0.5 days for the case group and 6±2 days for the control group, with a p<0.05. As we mentioned earlier, following our postoperative protocol, all the patients were discharged after their surgical drain had been removed (when the debit was ≤20ml/24h and serous in appearance, both for the case group and the control group). The median of the total quantity of drainage debit was significantly higher for the control group. The median time that the drain was removed was 36h after surgery for the group with Tissucol® and 120h for the group without Tissucol® (Table 1).
We found 5 seromas: 2 in the case group and 3 in the control group. Dysphonia presented in 6 patients, at their follow-up, transient in all cases. The onset of postoperative dysphonia was diagnosed through the clinical symptoms; we do not perform systematic laryngoscopies on our patients (Table 1).
If we consider that the daily cost of hospitalisation for one patient after thyroidectomy is 188.86€ in our institution, the resulting average cost per patient for the case group was 377.72€. By contrast, it was significantly higher for the control group: 1133.16€ (p<0.05).
DiscussionNew adhesives and sealants have appeared in recent years,17–28 such as Tissucol®, widely used in many fields of surgery in order to achieve complete haemostasis, and which when applied in the thyroid space can reduce local complications after thyroidectomy and hemithyroidectomy. This fibrin glue comprises 2 components of human origin: freeze-dried adhesive protein concentrate to be dissolved with aprotinin solution, and freeze-dried thrombin.
When these substances are combined, immediately before application, they form fibrin. The fibrin produced adheres to the tissues that are exposed by the surgical intervention, forming a mesh which serves as a support for the proliferation of fibroblasts and capillaries which proliferate during the healing process. In the final healing process of the wound, the solidified fibrin glue is completely reabsorbed over a period of 6–8 weeks.
The application of Tissucol® is indicated in the treatment of oozing, sealing and/or adhesion of tissue in surgical interventions, enabling reduced bleeding and lymphorragia.17,23,24 In our case we used Tissucol® for its adhesive properties, rather than its haemostatic properties, in order to reduce lymphorrhagia in the virtual space created by dissection and lymphadenectomy.
Despite the fact that placing drains in neck surgery has always been controversial, our group advocates their systematic use after total thyroidectomy+central lymph node emptying+lateral emptying.7,13,14,16 As we explained in previous paragraphs, we placed a drain in all the patients, and this was removed before discharge from hospital when it had fulfilled the aforementioned criteria (debit<20ml/24h, serous in appearance, after starting a normal diet).
Bearing in mind that both the case group and the control group were homogeneous with regard to age, sex and BMI, we found no statistically significant differences in terms of the variables studied: surgery time, length of incision, anatomopathological type of the tumour, intraoperative complications, postoperative complications, hypoparathyroidism and recurrent transient paralysis.
Our study shows that in the group of patients in whom the Tissucol® fibrin glue was used, the mean stay was 2±0.5 days, compared to 6±2 days for the control group (p<0.05). We put this reduction in the patients’ hospital stay down to the reduced drainage debit which enabled the drain to be removed early: a mean of 1.5 days after surgery in the Tissucol®, group compared to a mean of 5 days in the control group. However, in our case this was not accompanied by the consequent reduced risk of infection and pain, which has been reported in other published series.16 In other words, the application of fibrin glue did not reduce the rate of complications, but it did reduce the number of days of drainage, achieving an earlier debit of ≤20ml/24h.
It is important that the patients’ shortened hospital stay results in a significant reduction of hospital costs which implies a significant financial saving. As we mentioned, the mean daily stay for these types of patients is 188.86€ in our hospital, which means that the average cost per patient for the case group was significantly less compared to the control group (377.72€ vs. 1133.16€), with p<0.05.
We can conclude therefore that in our environment the application of Tissucol® fibrin glue statistically significantly reduced the hospital stay of the operated patients, without affecting the onset of complications associated with the intervention and with the consequent financial saving for the institution.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Vidal-Pérez O, Flores-Siguenza L, Valentini M, Astudillo-Pombo E, Fernández-Cruz L, García-Valdecasas JC. Aplicación de sellante de fibrina en pacientes operados por cáncer diferenciado de tiroides. ¿Qué mejoramos?. Cir Cir. 2016;84:282–287.