The presence of deep neck abscesses is potentially serious; they can lead to death in a short period of time. The vacuum-assisted closure (V.A.C.) therapy has been used in many areas of surgery for complex wound healing. This treatment modality has recently been considered in the field of head and neck surgery.
ObjectiveEvaluate the efficacy of healing therapy using V.A.C. therapy in deep neck abscesses.
Material and methodsOpen-label trial. Patients with deep neck abscesses were included using V.A.C. therapy vs. conventional therapy. Cultures were taken before and during surgery, and prior to primary wound closure. The percentages of healing, viable tissue, wound healing time, and hospital stay were evaluated.
ResultsA total of 18 patients were included. Affected neck spaces: submaxilar 29%, parapharyngeal 22%, submental 21% and masticatory 13%. The final postsurgical culture was negative in 78%. Viable tissue of the wound for the V.A.C. group was 42%, and for the control group was 36% (p=0.025). Healing time was 22±6 days and 38±15.5, respectively (p=0.01). The mean number of hospital stay was 12 days for both groups.
ConclusionsTherapy with V.A.C. is useful in the treatment of deep neck abscesses; it decreased healing time as a result of more viable tissue allowing suture closure of the wound in a shorter period.
La presencia de abscesos profundos de cuello es potencialmente grave, incluso puede llevar a la muerte en un tiempo muy corto. El cierre asistido por vacío (V.A.C.) se ha utilizado en muchas áreas de la cirugía para la cicatrización de heridas complejas. Recientemente se ha considerado esta modalidad de tratamiento en el campo de la cirugía de cabeza y cuello.
ObjetivoEvaluar la eficacia de la cicatrización mediante terapia con V.A.C. en abscesos profundos de cuello.
Material y métodosEnsayo clínico abierto. Se incluyó a pacientes con abscesos profundos de cuello a tratarse con V.A.C., en comparación con terapia convencional. Se tomaron cultivos antes, durante y previamente al cierre primario de la herida. Se evaluó el porcentaje de cicatrización, tejido viable, tiempo de cicatrización y estancia hospitalaria.
ResultadosSe incluyó a 18 pacientes. Espacios de cuello afectados: submaxilar 29%, parafaríngeo 22%, submentoniano 21% y masticatorio 13%. Cultivo posquirúrgico final negativo en el 78%. Porcentaje de tejido viable de la herida para el grupo V.A.C. 42%, grupo control 36% (p=0.025). Tiempo de cicatrización 22±6 días y 38±15.5, respectivamente (p=0.01). La media de días de hospitalización fue de 12 para ambos grupos.
ConclusionesLa terapia con V.A.C. es útil en el tratamiento de los abscesos profundos de cuello, ya que disminuyó el tiempo de cicatrización como resultado de mayor tejido viable, lo que permitió el cierre con sutura de la herida en un periodo más corto.
Deep neck infections are singular among all infections due to major risk of complications. Treatment is aggressive and the monitoring of the airway is of extreme urgency, followed by correct antibiotic treatment and surgical drainage.1
The main cause of neck abscesses in adults is associated with odontogenic infections. Other causes are: trauma, oesophageal perforation, laryngocele, thyroglossal cyst, thyroiditis and Bezold abscess. In patients who are infected with human immunodeficiency virus and those with diabetes mellitus, cases are atypical and there is a higher rate of complications.1,2
First line treatment is surgical drainage when there is compromise of the airway, septicaemia, descendant strains of infection, absence of improvement in the first 48h of treatment with parenteral antibiotics, and in abscesses over 3cm in diameter which involve the prevertebral, anterior or carotid visceral space or which involve more than 2 spaces.3,4
Vacuum-assisted closure (V.A.C.) therapy is a non invasive healing system which uses local negative and controlled pressure to stimulate deep and chronic wound healing. It consists of applying a sponge bed over the wound, sealing the wound with an adhesive film and applying negative air pressure. The combination of the reticulated sponge and the negative pressure promotes cell division of growth factors and equivalent angiogenesis, enhances clearance of swelling and reduces bacterial colonisation. No complications related to its use have been reported.5–7
The aim of this study is to assess the efficacy of V.A.C. therapy as a healing treatment in contrast to standard therapy for wounds from surgical drainage of deep neck abscesses.
Material and methodsOpen-label trial. It included patients with deep neck abscesses, who were treated using surgical drainage, with previous informed consent and who were dependants of the Mexican Social Security Institute.
Inclusion criteriaPatients of any gender, over 18 with deep neck abscesses and unilateral or bilateral incision from the anterior edge of the sternocleidomastoid muscle to the paratracheal line and with a spread of infection to a space over 7cm. Patients with extensive necrosis of tissues which would have impeded wound suture were excluded from the study.
Study variablesThe study variables were the percentage of granulation tissues during the healing period, time of healing, the microorganisms present, hospital stay, complications, and mortality.
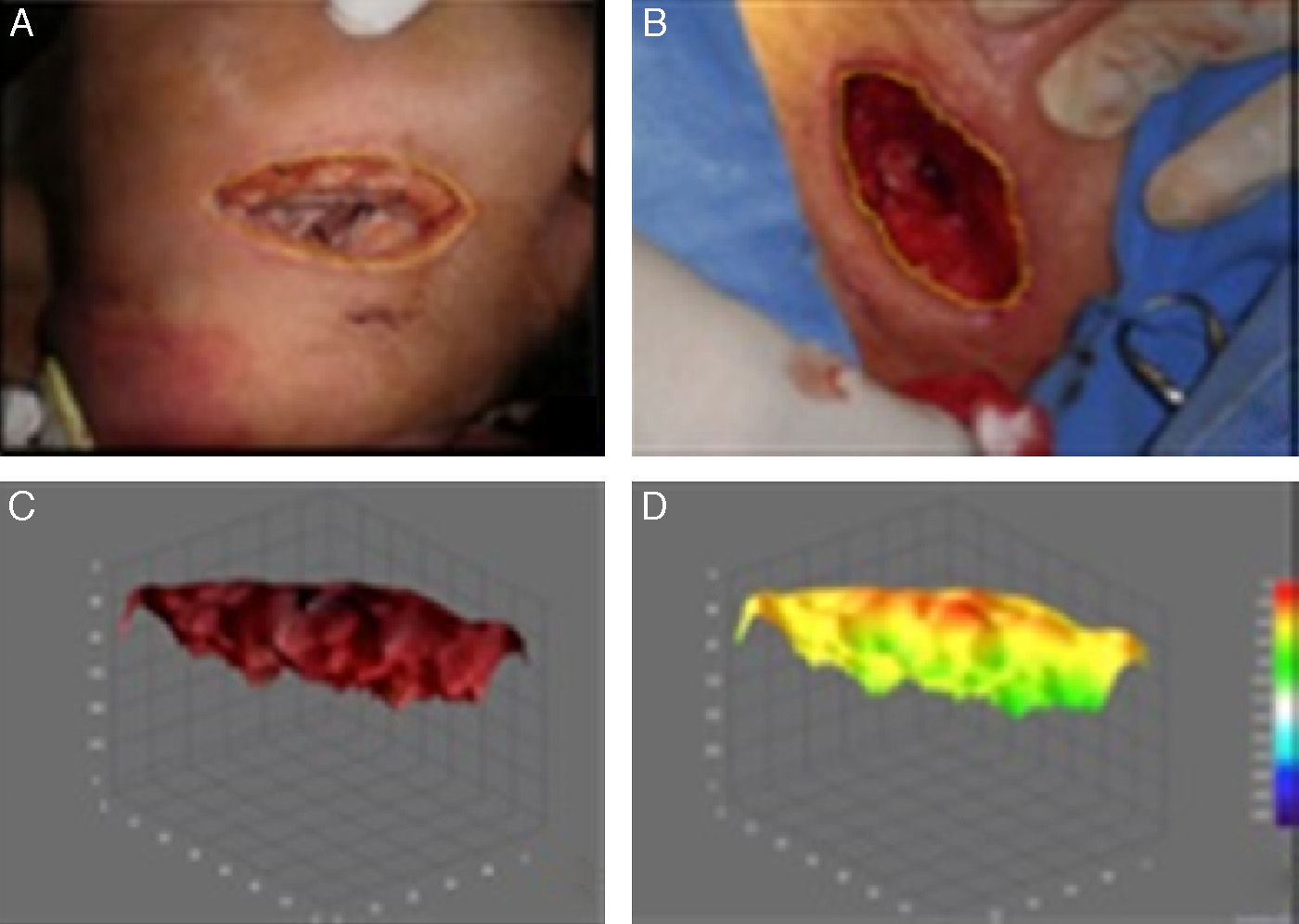
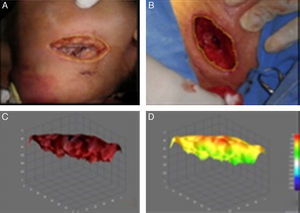
Granulation tissue was assessed using the Image J programme (Image Processing and Analysis in Java. Version 1.34s; National Institute of Health, Bethesda, MD, USA).
ProcedureOnce the patient had met the inclusion criteria and given their informed consent, they were split into 2 Groups: Group A, who were treated with V.A.C. therapy and Group B, who received conventional therapy.
Group ASurgical drainage was carried out, secretion cultures were taken and washed with saline solution to completely eliminate pus. The wound conditions were documented, prior to asepsis and antisepsis and a sponge was positioned (V.A.C.®, Kinetic Concepts Inc., San Antonio, TX, USA), which was contoured to wound size. A suction tube was then inserted and was covered with an adhesive film. The wound was inspected and the sponge was changed every 72h, assessing the percentage of granulation tissue. Secretion cultures were taken in each change, to assess evolution. When the wound showed no signs of pus or granulation tissues, primary closure was made.
Group BFollowing surgical drainage and the taking of secretion cultures, the wound was washed with a saline solution, to eliminate pus. Wound conditions were noted. Inspection of healing and changing of gauzes was carried out every 8h, during the first 48h and then after every 12h, until the percentage of viable granulation tissue was obtained. Secretion cultures were made every 72h. The therapy was continued until the granulation tissue completely covered the wound.
Statistical analysisThis was descriptive using: frequencies, percentages, means, standard deviation of the mean and standard error of the mean. Inferential studies for quantitative variables were carried out, using the Student's t-test for small samples and the Chi-square test or the exact Fisher test for qualitative variables. The SPSS (Package for the Social Science, SPSS Inc., Chicago, IL, USA) version 17.0 statistical programme for Windows was used.
Ethical considerationsThe ethical aspects in this study are based on the General Health Act in Research Material for Health and the 1975 Declaration of Helsinki and its amendments. They are also based on prevailing national and international codes for good practices in research. They were authorised with number 2011/1301/118 of the Research Committee registry.
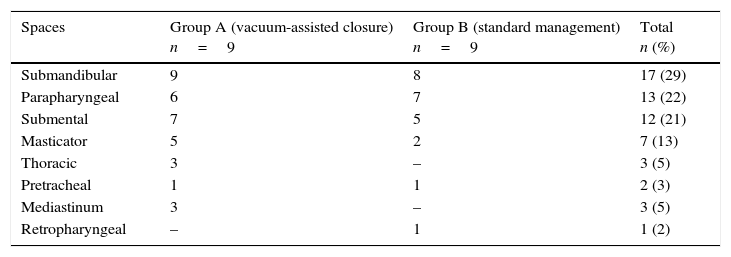
ResultsA total of 18 patients were included in the study. Males were more affected: 10 (55%). The associated diseases in the study group and the control group were as follows: overweight, 7 (77.7%) and 4 (44.4%); diabetes mellitus 5 (55.5%) and 4 (44.4%); systemic arterial hypertension, 4 (44.4%) and 2 (22.2%), and malnutrition in 6 (66.6%) patients in each group. The deep spaces of the neck affected are shown in Table 1. 6 (33.3%) patients underwent tracheostomy: 3 in each group. With regards to the aetiology of the deep neck abscesses, the most common cause in both the study and the control group was odontogenic (50% in both groups), infection of the upper airways (20% vs. 22%), followed by trauma (28% vs. 14%).
Deep spaces of neck involved in study and control groups.
| Spaces | Group A (vacuum-assisted closure) n=9 | Group B (standard management) n=9 | Total n (%) |
|---|---|---|---|
| Submandibular | 9 | 8 | 17 (29) |
| Parapharyngeal | 6 | 7 | 13 (22) |
| Submental | 7 | 5 | 12 (21) |
| Masticator | 5 | 2 | 7 (13) |
| Thoracic | 3 | – | 3 (5) |
| Pretracheal | 1 | 1 | 2 (3) |
| Mediastinum | 3 | – | 3 (5) |
| Retropharyngeal | – | 1 | 1 (2) |
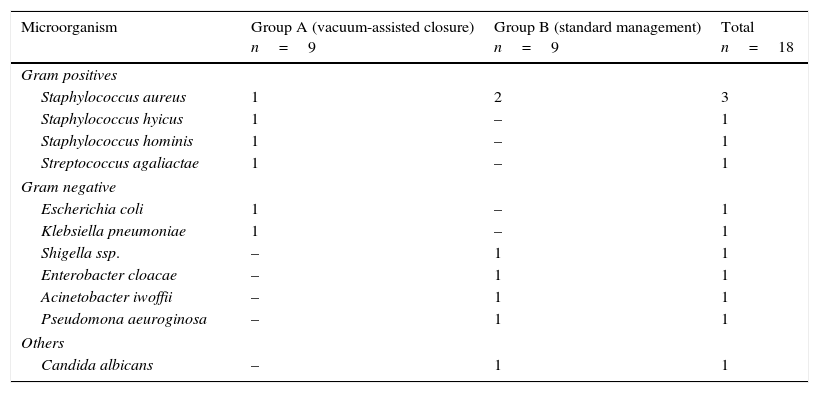
Transsurgical cultures showed a negative culture at 72h in 11 (61%) patients, whilst 5 (27%) were from a single microorganism and 2 (12%) polybacterial. The cultures at the end of the study in patients in group A showed an absence of microorganisms in 7 (78%); however, 2 (22%) patients presented with a positive single bacterial culture. In the patients in group B, 7 showed a negative culture and 2 a positive culture, one was unibacterial and the other polybacterial. The isolated microorganisms are presented in Table 2.
Microorganisms isolated from the cultures in both groups after 72h of surgical draining.
| Microorganism | Group A (vacuum-assisted closure) n=9 | Group B (standard management) n=9 | Total n=18 |
|---|---|---|---|
| Gram positives | |||
| Staphylococcus aureus | 1 | 2 | 3 |
| Staphylococcus hyicus | 1 | – | 1 |
| Staphylococcus hominis | 1 | – | 1 |
| Streptococcus agaliactae | 1 | – | 1 |
| Gram negative | |||
| Escherichia coli | 1 | – | 1 |
| Klebsiella pneumoniae | 1 | – | 1 |
| Shigella ssp. | – | 1 | 1 |
| Enterobacter cloacae | – | 1 | 1 |
| Acinetobacter iwoffii | – | 1 | 1 |
| Pseudomona aeuroginosa | – | 1 | 1 |
| Others | |||
| Candida albicans | – | 1 | 1 |
Of the patients in the study group, 3 (33%) presented with a persistent purulent secretion 4 days after the removal of the V.A.C. and one patient presented with dehiscence of the sutured wound, after the system had been removed. In the control group, one patient required a second surgical intervention due to residual abscess. Other complications were pleural effusion in 3 (33%) corresponding to the control group, followed by 2 cases of pulmonary thromboembolia, one in the study group and one in the control group, and 2 cases of mediastinitis in the control group. 50% of the patients with mediastinitis required tracheotomy. The average of surgical interventions in group A was one, in contrast to 4 in group B.
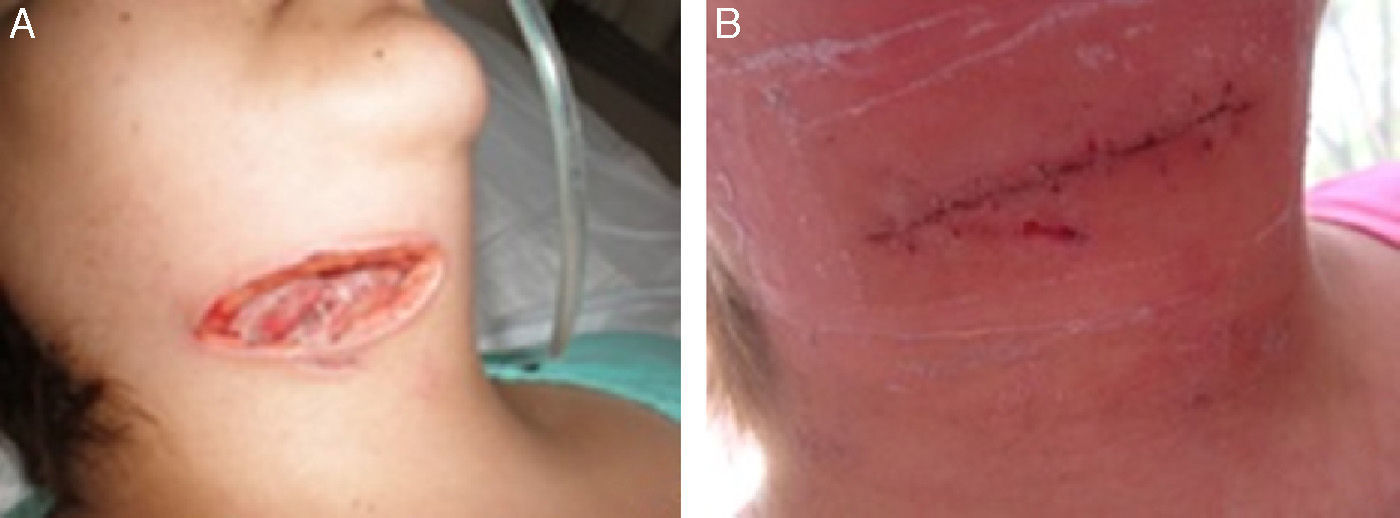
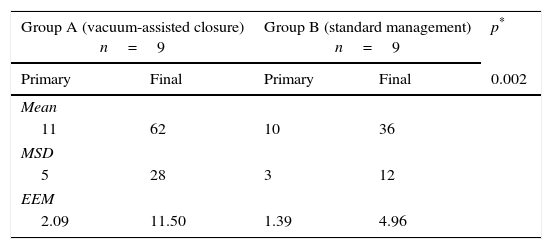
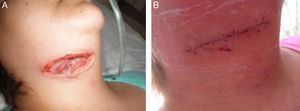
The percentage of viable tissues for group A was initially 11% and finally 62%; In group B it was initially 10% and finally 36% (p=0.025) (Figs. 1 and 2) (Table 3). With regards to the number of days required for wound healing in group A, the mean was 22, with a mean standard deviation of 6, and a standard error mean of 2.4 compared with group B with a mean of 38, mean standard deviation of 15.5 and standard error mean of 6.3 (p=0.01).
Percentage of viable tissue.
| Group A (vacuum-assisted closure) n=9 | Group B (standard management) n=9 | p* | ||
|---|---|---|---|---|
| Primary | Final | Primary | Final | 0.002 |
| Mean | ||||
| 11 | 62 | 10 | 36 | |
| MSD | ||||
| 5 | 28 | 3 | 12 | |
| EEM | ||||
| 2.09 | 11.50 | 1.39 | 4.96 | |
MSD, mean standard deviation; MSE, mean standard error.
Mean hospital stay in days for group A was 12.33±5 and for group B was 12.83±8 days (p=0.43). There were no deaths.
DiscussionDespite the impact of antibiotic treatment nowadays, deep neck abscesses are still a frequent disease to be found in the emergency otolaryngology services in clinical practice.
This study was carried out to analyse the clinical characteristics of patients with deep neck abscesses and to assess the efficacy of V.A.C. therapy for the treatment of this condition.
The most common aetiology of deep neck abscesses was odontogenic in 50% of cases and secondary to this were infection of airways in 21%. In the study by Cárdenas et al., dental infection was observed in 80% of cases and worldwide literature reports this as a principal cause.8–11 Kim et al.12 reported that the most frequently affected spaces secondary to original dental infection are the submandibular, parapharyneal and masticator spaces. In our study the deep neck spaces affected most frequently were: submandibular, parapharyngeal and submental.
The prevalence of pathogenic microorganisms causing deep cervical space infections varies in accordance with the population studied and the origin of infection: in our case we observed that Staphylococcus aureus was the most frequent bacteria. Lee and Kanagalingam13 recognised this microorganism together with other gram positive microorganisms as one of the most prevalence causes due to the fact that several of its species usually inhabit the oral cavity. However, it is of note that there is both an absence of anaerobic microorganisms inside the pathogen agents and that the majority of cultures were unibacterial. This contrasts with already well reported literature regarding the polymicrobial cause of deep neck abscesses.14,15 It has been observed that this fact may be owing to the antibiotic treatment administered prior to hospital admittance of the patient or to the use of intravenous therapy prior to surgical drainage of the abscess.16
Surgical drainage with debridement associated with the systemic administration of antibiotics, after controlling the airway, is considered to be the treatment of choice in deep neck abscesses. However, particularly in complicated cases, multiple reviews of the surgical site may be required.17
In standard practice, surgical drainage of an abscess requires extensive incision to clean the deep cervical spaces affected, with exposure of the tissues, increase in the risk of over infection and unsatisfactory aesthetic results of healing. The patients treated with this conventional method, in our study, required one or more cervical incisions depending on the affected spaces and mechanical curing 2 or 3 times a day, depending on the wound conditions. In general, all the patients mentioned discomfort during healing which varied depending on each patient's pain threshold.
The V.A.C. therapy system has been used to reduce the risk of haematomas and for drainage after abdominal orthopaedic, orals or neurosurgical surgery.18,19 It has been satisfactorily used to reduce swelling, promote granulation tissues, improve skin grafts, improve blood flow and reduce bacterial load.20–26
The use of V.A.C. in the craneocervical area is an important part of postoperative management of deep neck abscesses since it promote the integrity of the flap, wound healing and revascularisation in addition to reducing postoperative infection of the wound.18 However, there is very little experience with the V.A.C. system in the management of infected wounds in the cervicofacial area. Gallo et al.17 showed how effective this system was, in their study on a patient with a deep neck abscess compromised by mediastinitis. The need for thoracotomy for mediastinal drainage was avoided and clinical and tomographic improvement was enhanced after 3 days of therapy with negative pressure.
In their study involving 30 patients with deep neck abscesses treated with a negative pressure system, Hyun et al.18 supported the major clinical use of this system compared with others using other drainage systems, as they observed that minimal incisions were required and that postoperative management was simple and presented fewer complications.
The mean hospital stay in our study was 12 days for both groups, with a range of 6–18 days. In the study by Dhir et al.27 all patients of the study received V.A.C. therapy in the hospital with a mean of 11.4 days, and within a range of 5 to 28 days; 83% of patients did not need another treatment for healing the wound and 84% were cured without the need to administer other therapies or undergo surgical interventions. They concluded that this modality could be applied to dehiscent wounds with or without blood vessel exposure, to tissues treated with chemotherapy and radiotherapy, salivary fistulas or necrotising fasciitis. However, they also reported the following disadvantages: the need for correct application around the airway, failure for complete closure of salivary fistulas, the need for creativity in application of the sponges in patients with multiple wounds, and contraindication in its use on patients with suspected or confirmed biopsy results of malignancy.
In our study we observed a significant difference in time for wound healing in both groups: there was a higher percentage of tissue granulation and a faster development of it in the group treated with V.A.C. therapy compared with the control group. Furthermore, wound closure and wound healing had aesthetically more favourable outcomes, compared with the standard cure for drained cervical abscesses.
ConclusionsV.A.C. therapy is effective in the treatment of deep neck abscesses, since it reduces healing time and increases viable tissue growth compared with standard treatment. Suture closure of the wound occurs in a shorter period, and thus also reduces the trauma of curing.
The therapeutic proposal derived from this study, based on outcome, is that this is the best treatment option for patients under these conditions who have been treated for neck abscesses with conventional wound closure therapy at secondary or tertiary intention. Our proposal promotes wound closure using sutures which benefit healing, as shown via the infection-free viable epithelisation, the obtainment of negative cultures and the clinical photographic evidence.
Conflict of interestsThe authors have no conflict of interests to declare.
To the MPSS Aida Rebeca Márquez Valdez for her support in image editing.
Please cite this article as: Govea-Camacho LH, Astudillo-Carrera A, Hermosillo-Sandoval JM, Rodríguez-Reynoso S, González-Ojeda A, Fuentes-Orozco C. Impacto del manejo con cierre asistido al vacío en abscesos profundos de cuello. Cir Cir. 2016;84:275–281.