Puncture biopsy and fine needle aspiration guided by endoscopic ultrasound has been used as an effective technique and is quickly becoming the procedure of choice for diagnosis and staging in patients suspected of having pancreatic cancer. This procedure has replaced retrograde cholangiopancreatography and brush cytology due to its higher sensitivity for diagnosis, and lower risk of complications.
ObjectiveTo assess the levels of pancreatic enzymes amylase and lipase, after the puncture biopsy and fine needle aspiration guided by endoscopic ultrasound in pancreatic lesions and the frequency of post-puncture acute pancreatitis.
Material and methodsA longitudinal and descriptive study of consecutive cases was performed on outpatients submitted to puncture biopsy and fine needle aspiration guided by endoscopic ultrasound in pancreatic lesions. Levels of pancreatic enzymes such as amylase and lipase were measured before and after the pancreatic puncture. Finally we documented post-puncture pancreatitis cases.
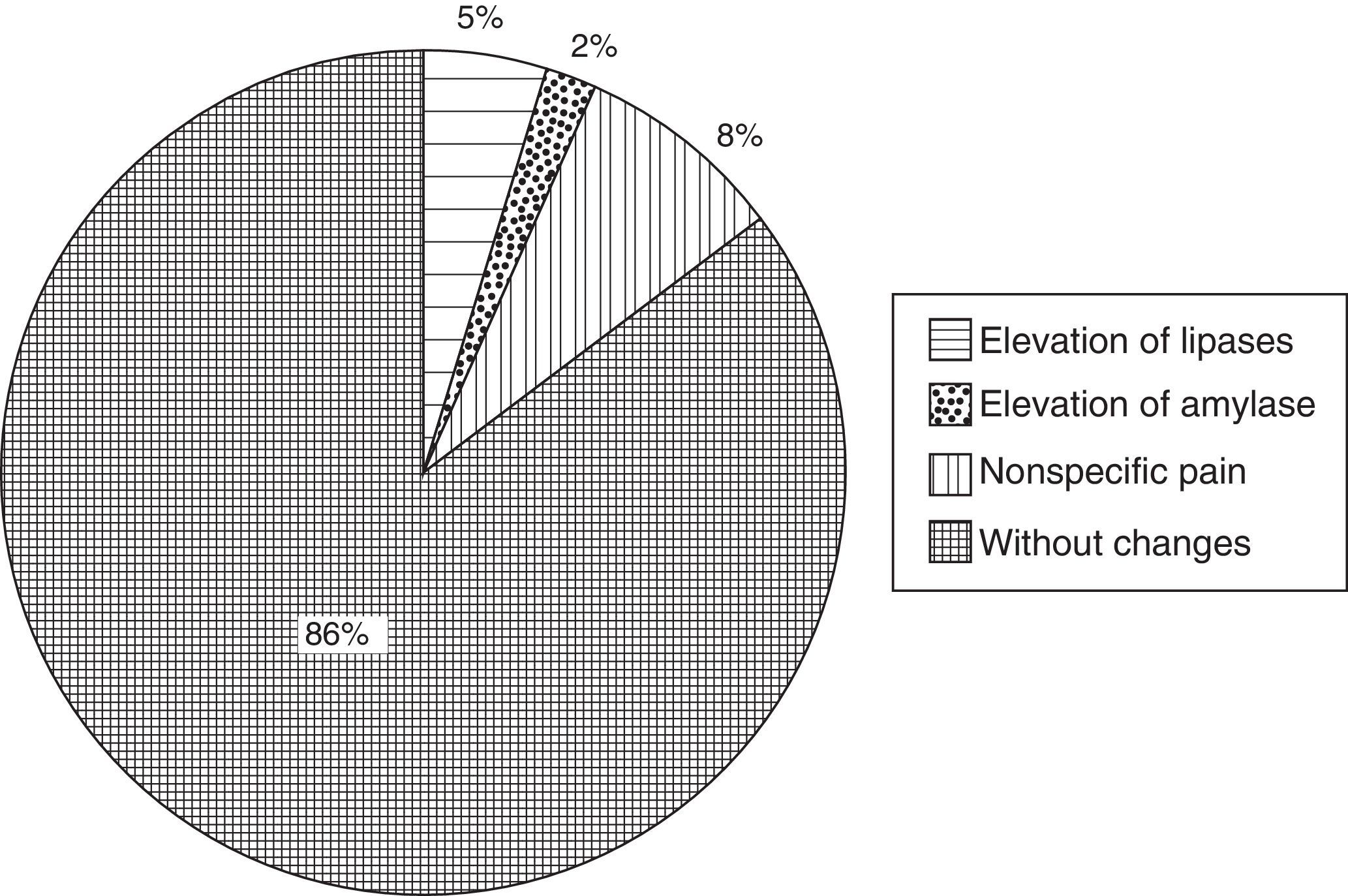
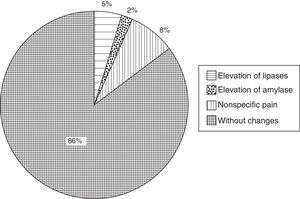
ResultsA total of 100 patients who had been diagnosed with solid and cystic lesions were included in the study. Significant elevation was found at twice the reference value for lipase in 5 cases (5%) and for amylase in 2 cases (2%), none had clinical symptoms of acute pancreatitis. Eight (8%) of patients presented with mild nonspecific pain with no enzyme elevation compatible with pancreatitis.
ConclusionPancreatic biopsy needle aspiration guided by endoscopic ultrasound was associated with a low rate of elevated pancreatic enzymes and there were no cases of post-puncture pancreatitis.
La biopsia por punción y aspiración con aguja fina guiada por ultrasonido endoscópico ha sido utilizada como una técnica eficaz que se está convirtiendo rápidamente en el procedimiento de elección para el diagnóstico y la estadificación de los pacientes en los que se sospecha cáncer de páncreas. Este procedimiento ha desplazado a la colangiopancreatografía retrógrada y a la citología por cepillado debido a su mayor sensibilidad y menor riesgo.
ObjetivoDeterminar el nivel sérico de enzimas pancreáticas tales como amilasa y lipasa posterior a la realización de una biopsia por punción y aspiración con aguja fina guiada por ultrasonido endoscópico en lesiones de páncreas, además de la frecuencia de pancreatitis aguda pospunción.
Material y métodosSe realizó un estudio longitudinal y descriptivo de casos consecutivos en pacientes que fueron sometidos a una biopsia por punción y aspiración con aguja fina. Se realizó la medición de los niveles séricos de enzimas pancreáticas amilasa y lipasa antes y después de la punción, además de documentar los casos de pancreatitis.
ResultadosUn total de 100 pacientes con lesiones pancreáticas de tipo sólido y quístico fueron incluidos. Encontramos una elevación clínicamente significativa, el doble del valor de referencia de lipasa en 5 casos (5%) y de amilasa en 2 (2%); en ningún caso se presentó cuadro clínico de pancreatitis aguda. El 8% de los pacientes refirió dolor no compatible con un diagnóstico de pancreatitis.
ConclusiónLa biopsia por punción y aspiración con aguja fina guiada por ultrasonido endoscópico se asoció a una baja tasa de elevación de enzimas pancreáticas y en ningún caso se desarrolló pancreatitis pospunción.
Endoscopic ultrasound-guided (EUG) fine needle aspiration biopsy (FNAB) has been used for diagnosis in patients with a suspected tumour of the pancreas,1–6 because ultrasound has been demonstrated to be more sensitive for diagnosis, and there is a low risk of complications. Reports of complications associated with the procedure vary from 0% to 5%, these include: acute pancreatitis,7 bleeding, infection and perforation. The risk factors for biopsy-related pancreatitis are unknown, but the result of one study show that patients with a history of recent acute pancreatitis or puncture of a healthy pancreas are more likely to develop acute pancreatitis after fine needle aspiration biopsy,8 therefore some researchers consider such a history a risk factor.9
Acute pancreatitis or acute inflammation of the pancreas is secondary to the intraglandular activation of the pancreatic enzymes and is a disease of varied clinical presentation from very mild, self-limiting cases to multiorgan failure and death. This is a local inflammatory process which results in a systemic inflammatory response in most cases.10
The disease's pathophysiology includes the activation and release of pancreatic enzymes into the interstitium with pancreatic self-digestion and in severe cases, multiple organ dysfunction due to spread of the inflammatory mediators of the pancreas11,12 and other pancreatic enzymes such as amylase, lipase and nucleases, which are also actively secreted.
The production of cytokines and chemokines by the acinar cells of the pancreas has recently been recognised to be the first signal required for recruitment of inflammatory cells to the pancreas during the onset of pancreatitis.13 Damage to the acinar cell is followed by a proinflammatory cascade which results in pancreatic necrosis, systemic inflammatory response syndrome and distant organ dysfuntion.14 Chemokines are related to highly conserved cytokines with chemotaxis properties and orchestrate the migration of leukocytes to areas of inflammation.15 In pancreatitis cases, amylase tends to elevate in the first 24h and remains elevated from 1 to 3 days; levels usually return to normal after days 3–5. This test has a sensitivity of 82%, specificity of 91%, and a positive predictive value of 65%. Other processes that cause amylase elevations should always be discounted, however, in practice and under normal conditions, only the pancreas and the salivary glands significantly contribute to the maintenance of the serum levels of this enzyme. Serum amylase levels are only useful for diagnosis and bear no correlation with the severity of the picture, and therefore have no prognostic value.
Lipase is the second most frequently used test in the diagnosis of acute pancreatitis. Lipasaemia has the advantage that it does not elevate in some situations that cause false positives of amylase. However, it accompanies amylase in false positives secondary to biliary disease, perforated ulcer, intestinal obstruction, mesenteric thrombosis and acute appendicitis. The activity of serum lipase increases in parallel to that of amylase and testing for both enzymes increases diagnostic performance.
Lipase levels can remain elevated for 7 to 14 days. Lipase may now be the most indicated enzyme to establish a diagnosis. It has a sensitivity of 94%, specificity of 96% and a positive predictive value of 86%. Elevated lipase and serum trypsin levels can be diagnostic of acute pancreatitis, and therefore these tests are particularly useful in patients with hyperamylasaemia of non-pancreatic origin.
It has been published in the international literature that the presence of abdominal pain and enzyme elevation of at least 3 times the benchmark levels should be present for a diagnosis of pancreatitis to be considered.
Since there are no publications yet in this regard from our country, it is essential for us to generate information in our environment and contrast it with the results of the international literature, because increasingly more centres are performing these procedures. Therefore, our main objective as authors is to assess the levels of pancreatic enzymes, particularly amylase and lipase, before and after performing an endoscopic ultrasound-guided (EUG) fine needle aspiration biopsy (FNAB) in pancreatic lesions and compare these before and after levels. In addition, our second objective is to report the frequency of acute pancreatitis in our patients after performing the puncture.
Material and methodA longitudinal, prospective and descriptive study was performed of the serum amylase and lipase levels of patients who underwent EUG FNAB referred to our department between 1 March 2012 and 1 March 2013. The levels were measured before and after the biopsy was performed. The study was undertaken in the Endoscopy Department of the Hospital de Especialidades del Centro Médico Nacional Siglo XXI of the Mexican Social Security Institute.
PatientsThe patients were diagnosed with pancreatic lesions, including solid and cystic lesions. All the patients were included that required EUG FNAB to establish the aetiology of their lesions and who agreed to take part in the study after signing their informed consent.
Patients with a documented diagnosis of pancreatic abscess and those with elevated pancreatic enzymes prior to the puncture procedure were excluded. Patients who had signed their informed consent and who later refused to participate were removed from the study and none of their data was used.
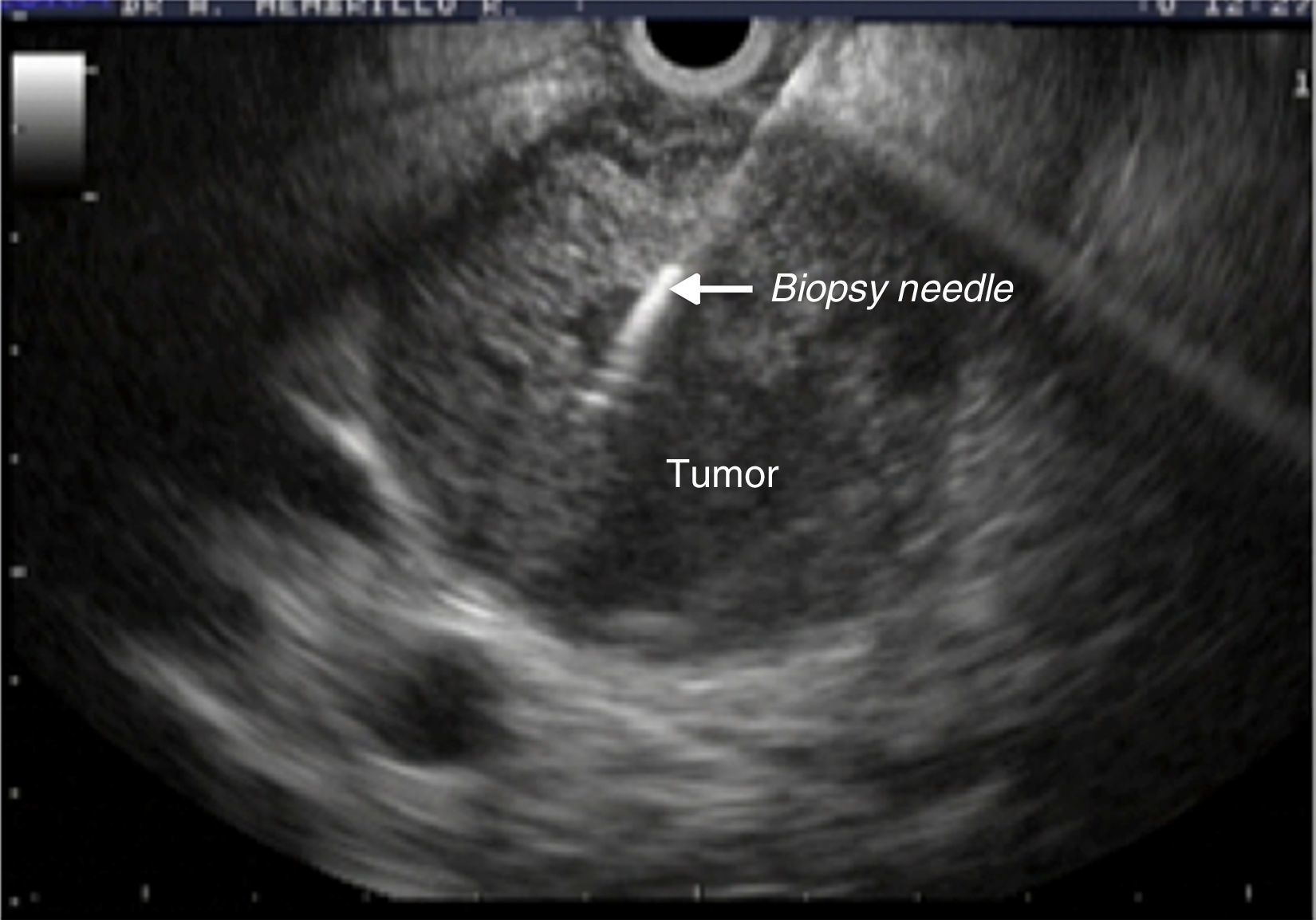
Equipment and proceduresThe EUG FNAB was performed with a 22-G Wilson Cook® needle (Cook Medical Incorporated) and Olympus® (Olympus Corporation) GF-UCT140 linear ultrasound array (Fig. 1). All the equipment is part of the biomedical services provided by the Mexican Social Security Institute. The procedures were undertaken with anaesthetic support and after preoperative assessment. A transgastric approach was used for lesions of the neck, body and tail of pancreas; lesions of the head and uncinate process of the pancreas required a transduodenal approach.
A blood sample was taken in all cases before the procedure to assess the serum levels of amylase and lipase. The second sample was taken 2h after the puncture was performed. Once the procedure was completed, the patients were monitored in the recovery room, where they stayed for an average of 6–8h, until they were discharged. Since most were outpatients, follow-up was by telephone at 24, 48 and 72h. For the hospitalised patients, follow-up was performed by visits until they were discharged. Patients who had suspected or were showing signs of acute pancreatitis, such as abdominal pain, nausea and vomiting were also hospitalised.
The pancreatic enzyme testing was performed in the hospital's own laboratory. For amylase, the photometric technique was used with 4,6-ethylidene-(G7)-p-nitrophenyl-(G1)-alpha-D-maltoheptaoside reagent, which is an oligosaccharide that breaks down the catalytic action of the alpha-amylases; the resulting fragments completely hydrolyse to p-nitrophenol and glucose through alpha-glucosidase action. The intensity of the p-nitrophenol formed is directly proportional to the activity of the alpha-amylase. Lipase is a glycoprotein with a molecular weight of 47,000Da and is termed triglyceride hydrolase, its transformation catalyses to diglycerides, monoglycerides and free acids. When lipase is added glutaric acid forms, which is an alkaline solution that is transformed into methylresorufin. This reaction is proportional to the amount of lipase, and gives a reddish colour which is also measured by photometry. All the tests were performed in automated form with a Hitachi autoanalyzer.
Statistical analysisBecause there are few very clear data in the literature on how much pancreatic enzymes increase after EUG FNAB, we decided to describe the changes in these levels, particularly amylase and lipase, as a variable of interest, and then to report the frequency of acute pancreatitis post puncture. The sample was obtained by non-probabilistic sampling of consecutive cases by convenience, where we used descriptive statistics for the sample's demographic and clinical variables, represented by frequencies and percentages for nominal variables and means with standard deviation for continuous variables. The final data were analysed using SPSS version 20 for MAC.
ResultsA total of 100 patients were included in the study over one year.
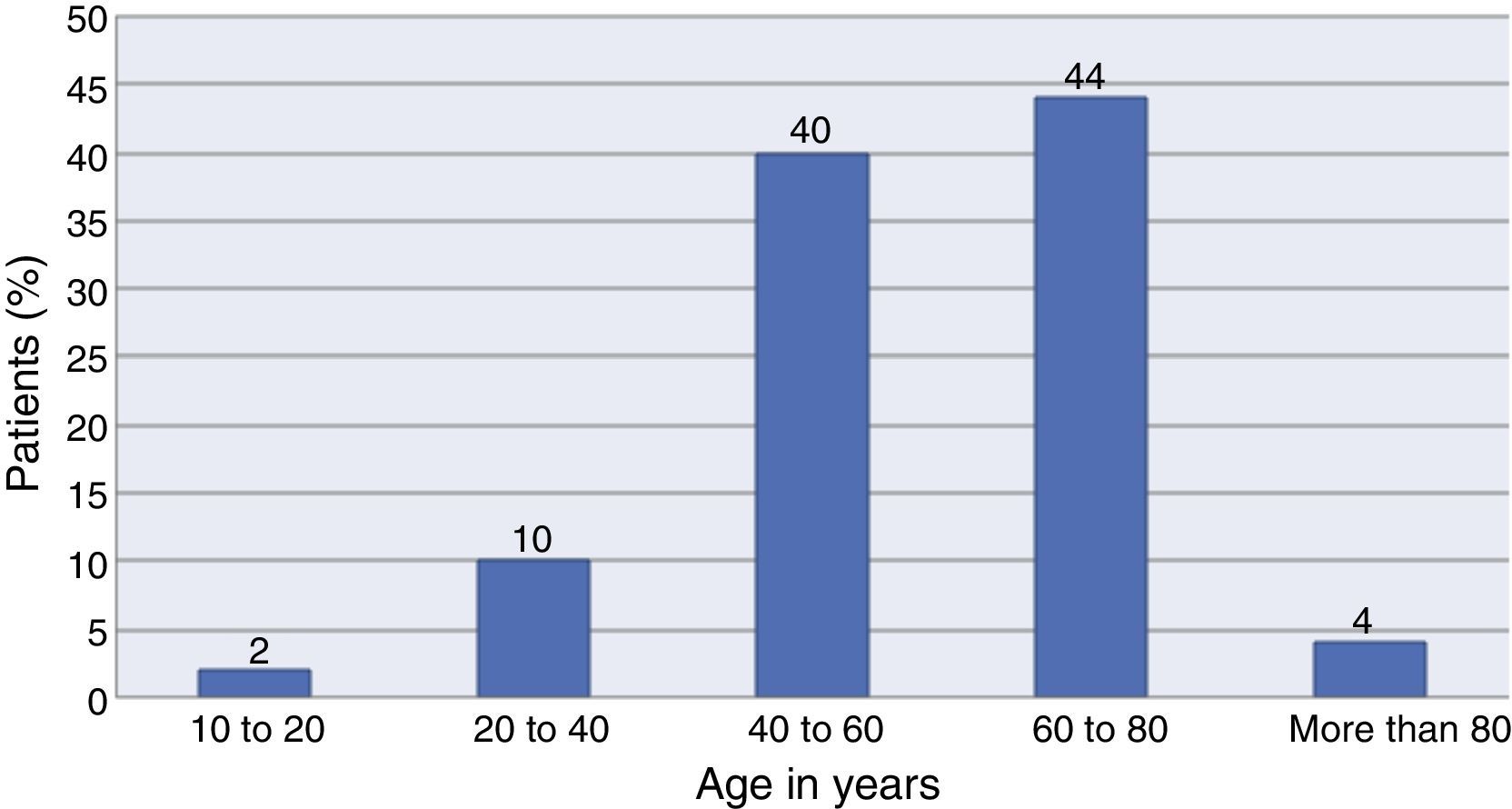
Forty percent (n=40) of the total sample were male and 60% female. The age range was between 17 and 86 years, with a mean age of 56.4±13.3. The distribution by age is shown in detail in Fig. 2.
The most common pancreatic lesions were in the pancreatic head (73%, n=73), followed by the body (24%, n=24) and, finally, the tail and uncinate process of the pancreas (3%, n=3). The cytological diagnoses were classified as: malignant 67% (n=67), suspicious 7% (n=7), benign 15% (n=15) and inadequate sample in 11% (n=11). The most frequent histopathological diagnosis was adenocarcinoma and there was an average of 3 needle passes in all cases.
In terms of pancreatic enzymes, elevated lipase was recorded in 5% (n=5) of the cases and amylase in 2% (n=2) of the cases. None of the patients presented a significant amylase or lipase elevation above 3 times the benchmark level (13–60U/L for lipase and 28–100U/L for amylase). Eight percent (n=8) of the patients presented abdominal pain reported as mild and non-specific (Fig. 3). The pain disappeared before they were discharged, and their pancreatic enzyme levels showed no changes with respect to the baseline level. Therefore, none of the cases were compatible with a diagnosis of acute pancreatitis post puncture. Abdominal pain was not reported during clinical monitoring after recovery discharge or at home.
DiscussionAlthough there are no standardised criteria for diagnosing post-puncture pancreatitis, we took the universal criteria for acute pancreatitis as our basis: abdominal pain and elevated pancreatic enzymes at least three times the baseline level. This hospital is considered a tertiary referral centre and an average of 800–1000 procedures are carried out here each year. Given this amount, it general it can be claimed that there are few risks associated with the ultrasound-guided aspiration puncture biopsy procedure, like other centres where the procedure is performed.16 Some studies show that pancreatitis after puncture occurs more frequently in patients with a history of pancreatitis17 or when a healthy pancreas is punctured; other risk factors have also been mentioned such as lesions smaller than 3cm and more than 4 needle passes. The mechanism that causes pancreatitis after a needle puncture is still unclear and it is thought that puncturing the pancreatic parenchyma causes direct trauma to the gland, to the main duct or even one of its branches. This causes oedema and an acute inflammatory response which could be associated with the diameter of the lesions, the diameter of the needle, the number of punctures made, the technique used or the susceptibility of the patient. We know that the pancreas reacts to factors that cause it trauma with an elevation in the pancreatic enzymes, basically amylase and lipase, and therefore if a patient has clinical symptoms of abdominal pain, nausea and vomiting after a EUG FNAB, blood levels of lipase and amylase should be tested. If the levels have increased more than 3 times the baseline levels, the patients should start a management protocol like that for acute pancreatitis, since there is not yet a protocol for the management of post-puncture pancreatitis. Although the levels of amylase and lipase in our study were elevated, they were not elevated enough to show signs of post-puncture pancreatitis, and this elevation did not coincide with the patients who had abdominal pain. In these cases the pain did not require analgesia, since it was transitory and associated more with the abdominal distension created by the air inserted to carry out the procedure, and puncture of the abdominal wall.18 In sum, the risk of pancreatitis after EUG FNAB is low, in line with the international literature (<4%),19 and no symptoms compatible with post-puncture pancreatitis are reported in this paper. Similarly, we did not observe any cases of digestive perforation, haemorrhage secondary to the procedure or any infectious process, which have been reported as complications in other publications.20
The benefit of this report is that EUG FNAB is an increasingly used method, and in Mexico we still have no official reports of its risks and complications, therefore the information obtained in this group of patients is very useful in further developing the procedure. The complications reported worldwide indicate that it is a safe diagnostic procedure, which we also reflect in our results, and is ultimately an efficient, sensitive technique with a generous safety margin when performed by experienced endosopic ultrasonographers.
ConclusionEUG FNAB was associated with a low rate of elevated pancreatic enzymes and no patient developed post-puncture pancreatitis. The frequency of acute pancreatitis after puncture varies in each centre where EUG FNAB is performed and might relate to the experience of the doctor undertaking the procedure.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Membrillo-Romero A, Gonzalez-Lanzagorta R, Rascón-Martínez DM. Evaluación de los niveles de amilasa y lipasa posterior a la realización de biopsia por aspiración con aguja fina guiada por ultrasonido endoscópico en lesiones del páncreas. Cirugía y Cirujanos. 2017;85:387–392.