Cervical spondylotic myelopathy is caused by cervical stenosis. Several techniques have been described for the treatment of multilevel disease, such as the anterior corpectomy with titanium mesh cage and anterior cervical plate placement, which has the advantage of performing a wider decompression and using the same bone as graft. However, it has caused controversy since the collapse of the mesh cage continues being a major limitation of this procedure.
Material and methodA prospective 4-year follow-up study was conducted in 7 patients diagnosed with cervical stenosis, who were treated surgically by one level corpectomy with titanium mesh cage and anterior cervical plate placement, evaluating them by radiographs and clinical scales.
Results7 patients, 5 women and 2 males were studied. The most common level was C5 corpectomy (n=4). The Neck Disability Index (NDI) preoperative average was 30.01±24.32 and 4-year postoperative 16.90±32.05, with p=0.801. The preoperative and 4-year postoperative Nürick was 3.28±0.48 and 3.14±1.21 respectively, with p=0.766. Preoperative lordosis was 14.42±8.03 and 4-year postoperative 17±11.67 degrees, with p=0.660. The immediate postoperative and 4-year postoperative subsidence was 2.69±2.8 and 6.11±1.61mm respectively, with p=0.0001.
ConclusionsDespite the small sample, the subsidence of the mesh cage is common in this procedure. No statistically significant changes were observed in the lordosis or Nürick scale and NDI.
La mielopatía cervical espondilótica es ocasionada por un conducto cervical estrecho. Se han descrito varias técnicas para el tratamiento multinivel, como la corpectomía anterior más colocación de malla y placa anterior, que tiene la ventaja de realizar una descompresión más amplia y utilizar el mismo tejido óseo como injerto; sin embargo, es causa de controversia, ya que el hundimiento de la malla sigue siendo la mayor limitación que tiene este procedimiento.
Material y métodoSe realizó un estudio prospectivo con seguimiento a 4 años, en 7 pacientes con diagnóstico de conducto cervical estrecho que fueron tratados quirúrgicamente mediante corpectomía de un nivel, colocación de malla de titanio y placa cervical anterior, evaluándolos mediante radiografías y escalas clínicas.
ResultadosSe estudió a 5 pacientes femeninos y 2 masculinos. El nivel más común de corpectomía fue C5 (n=4). El índice de discapacidad cervical (IDC) prequirúrgico media de 30.01±124.32 y posquirúrgico a 4 años 32.05±16.90, p=0.801. El Nürick prequirúrgico y posquirúrgico a 4 años fue 3.28±0.48 y 3.14±1.21, respectivamente, p=0.766. La lordosis prequirúrgica fue de 14.42±8.03 y la posquirúrgica a 4 años 17±11.67 grados, p=0.660. El hundimiento posquirúrgico inmediato y posquirúrgico a 4 años fue de 2.69±2.8 y 6.11±1.61 mm, respectivamente, p=0.0001.
ConclusionesA pesar de lo pequeño de la muestra, el hundimiento de la malla es común en este procedimiento. No se observaron cambios estadísticamente significativos en la lordosis ni en la escala de Nürick ni en el IDC.
The term cervical spondylosis encompasses degenerative changes to the spine.
Cervical spondylosis is a sequence of changes to the intervertebral discs, the vertebrae and the joints, associated with degenerative changes caused by ageing or secondary to trauma. The main symptom is neck pain that is frequently associated with pain in the shoulder region.1–3
Cervical spondylotic myelopathy is a degenerative process caused by stenosis of the cervical canal and is the primary cause of functional disability in adults.4,5 For this reason, efforts have been made internationally to find appropriate treatment for this disorder. There are currently many surgical treatments for the condition that have been standardised over time.6–9
Although anterior cervical discectomy and fusion has been the gold standard in the treatment of cervical canal stenosis, techniques have been described to treat multilevel disease under the premise that the use of an implant reduces morbidity since it does not require taking a graft.10–12 Using a cervical mesh as an anterior support when performing a corpectomy, has the advantage over 2-level discectomy of creating a wider decompression window, and the same bone tissue from the corpectomy is used as the graft.13–15
The treatment is controversial, since subsidence of the cage is still the main limitation of this procedure.16–20
Anterior discectomy and arthrodesis with tricortical graft is currently the most commonly used technique to treat cervical radiculopathy and myelopathy. For placement of the tricortical graft, in biomechanical studies there is no statistical relevance of the height of the graft with application of distractive force.13 The use of cervical mesh cages started in 1986.21 Titanium mesh cages are rigid cylindrical implants which fill with spongy bone to provide anterior support and facilitate intervertebral arthrodesis.21,22 Their advantages are reduced morbidity at the donation site and their fusion rate; their disadvantages are their cost, determining radiographic union, revision surgery and migration.18,20,23–25 The indications for corpectomy are: multilevel disease, compression at the level of the posterior wall, anterior osteophytes, and deformity of the vertebral body.9
Nürick26 introduced a scale for assessing the gait of patients with spondylotic cervical myelopathy, consisting of 6 grades (grade 5 being the most serious): radicular symptoms with no myelopathic signs (0), normal gait with myelopathic signs (1), mild gait involvement (2), ataxic gait (3), assisted gait (4) and wheelchair-bound (5). The neck disability index27,28 is a self-administered questionnaire with 10 sections. Each of the sections (pain intensity, personal care, lifting, headache, concentration, work, driving, sleep and recreation) offer 6 possible responses that represent 6 progressive levels of functional capacity, and are scored from 0 to 5. The total score is expressed as a percentage of the maximum possible score.
There are international articles that cover the treatment of multilevel cervical canal stenosis by corpectomy and titanium mesh placement plus anterior fixation, the outcomes vary according to the authors. We found no literature at a national level when we performed a search in the Pub Med, Scielo, Scielo México, MD Consult, Science Directo and Ovid search engines using the keywords titanium mesh, cervical corpectomy and myelopathy and anterior fixation. We found 0 references containing reports on clinical and radiological evaluations of patients with this disorder in Mexican publications, using the abovementioned technique.
Therefore, the general aim was to establish an association between titanium mesh cage subsidence and clinical and functional outcomes at 4-year follow-up. The specific objectives were to assess subsidence of the mesh cage in millimetres by X-ray, classifying the grade of union by X-ray and clinical assessment using Nürick's classification for cervical myelopathy and the pre-and post-operative neck disability index (NDI).
Material and methodThis was a prospective, observational, longitudinal, open, non-randomised, deliberate intervention study with 4-year follow-up of 7 patients from our outpatients’ department with a diagnosis of cervical canal stenosis, aged over 40 years, who underwent corpectomy and placement of titanium mesh cage and one-level anterior cervical plate. The mesh cage was filled with autologous graft.
Demographic variables such as sex and age were assessed and intervening variables such as corpectomy levels, transoperative bleeding volume, surgical technique (mesh and anterior plate placement), grade of union, trans- and post-operative complications. Cervical lordosis was assessed and compared preoperatively and at 4-year follow-up. The dependent variable was the functional outcome assessed using the NDI and the Nürick functional scale, and mesh cage subsidence was the independent variable, assessed by digital X-rays and measured in millimetres in the DICOM® system.
The statistical analysis consisted of descriptive statistics estimating frequencies, percentages, measures of central tendency and dispersion. Paired t-tests and/or Wilcoxon signed Rank test, and Pearson and Spearman correlation tests were undertaken, as appropriate. A p value of <0.05 was accepted as statistically significant and the software packages Excel and SPSS v. 21 were used.
ResultsFrom January 2009 to December 2011, 13 patients were found with a diagnosis of cervical canal stenosis, who were treated surgically by corpectomy and placement of titanium mesh cage and one-level anterior cervical plate. Six of the patients were eliminated from the study: one died and the other 5 decided not to participate.
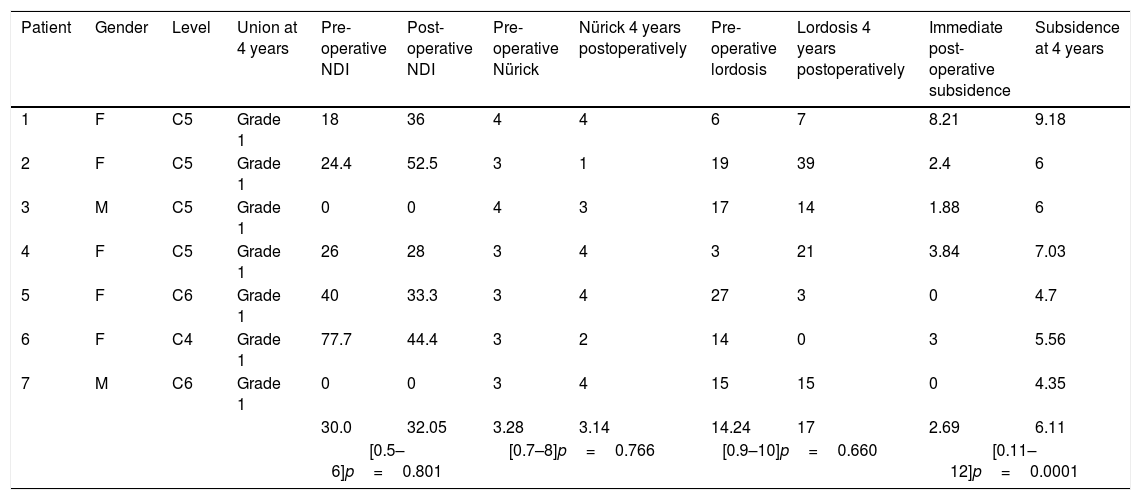
Of the 7 remaining patients in the study, 2 were male and 5 female, with a percentage of 28.6% and 71.4% respectively (Table 1).
Outcomes per patient.
| Patient | Gender | Level | Union at 4 years | Pre-operative NDI | Post-operative NDI | Pre-operative Nürick | Nürick 4 years postoperatively | Pre-operative lordosis | Lordosis 4 years postoperatively | Immediate post-operative subsidence | Subsidence at 4 years |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | C5 | Grade 1 | 18 | 36 | 4 | 4 | 6 | 7 | 8.21 | 9.18 |
| 2 | F | C5 | Grade 1 | 24.4 | 52.5 | 3 | 1 | 19 | 39 | 2.4 | 6 |
| 3 | M | C5 | Grade 1 | 0 | 0 | 4 | 3 | 17 | 14 | 1.88 | 6 |
| 4 | F | C5 | Grade 1 | 26 | 28 | 3 | 4 | 3 | 21 | 3.84 | 7.03 |
| 5 | F | C6 | Grade 1 | 40 | 33.3 | 3 | 4 | 27 | 3 | 0 | 4.7 |
| 6 | F | C4 | Grade 1 | 77.7 | 44.4 | 3 | 2 | 14 | 0 | 3 | 5.56 |
| 7 | M | C6 | Grade 1 | 0 | 0 | 3 | 4 | 15 | 15 | 0 | 4.35 |
| 30.0 | 32.05 | 3.28 | 3.14 | 14.24 | 17 | 2.69 | 6.11 | ||||
| [0.5–6]p=0.801 | [0.7–8]p=0.766 | [0.9–10]p=0.660 | [0.11–12]p=0.0001 | ||||||||
The levels resected were C5 in 4 cases (57.1%), C6 in 2 cases (6.9%) and C4 in 1 case (14.3%). Minimum surgery time was 100min and maximum 210min, with a mean of 153.57±40.28. Minimum transoperative bleeding was 150ml and maximum 300ml, with a mean of 200±57.73. The days of hospital stay were a minimum of 5 and maximum of 11, the mean was 7.57±2.43 (Table 1). Union of grade 1 was found in all patients at 4-year follow-up (remodelling and trabeculae) (Table 1).
The presurgical NDI was a minimum of 0 and a maximum of 77.7, with a mean of 30.01±24.32. The post-operative NDI at 4 years was a minimum of 0 and a maximum of 52, with a mean of 32.05±6.90. The correlation of the preoperative NDI and the postoperative NDI at 4 years was p=0.801, with 95% CI −21 at 16.91 (Table 1).
A minimum Nürick grade of 3 and a maximum of 4 were obtained, with a mean of 3.28±0.48. The postoperative Nürick at 4 years was a minimum of 1 and a maximum of 4, with a mean of 3.14±1.21. The correlation of the preoperative Nürick and the postoperative Nürick at 4 years was p=0.766, with 95%CI −.98 to 1.26 (Table 1).
A minimum of 3 degrees of preoperative lordosis was encountered and a maximum of 27 degrees, with a mean of 14.42±8.03. Postoperative–operative lordosis at 4 years was a minimum of 3 degrees and a maximum of 39, the mean was 17±11.67. The correlation between the preoperative and postoperative lordosis at 4 years was p=0.660, with 95% CI −16.18 to 11.04 (Table 1).
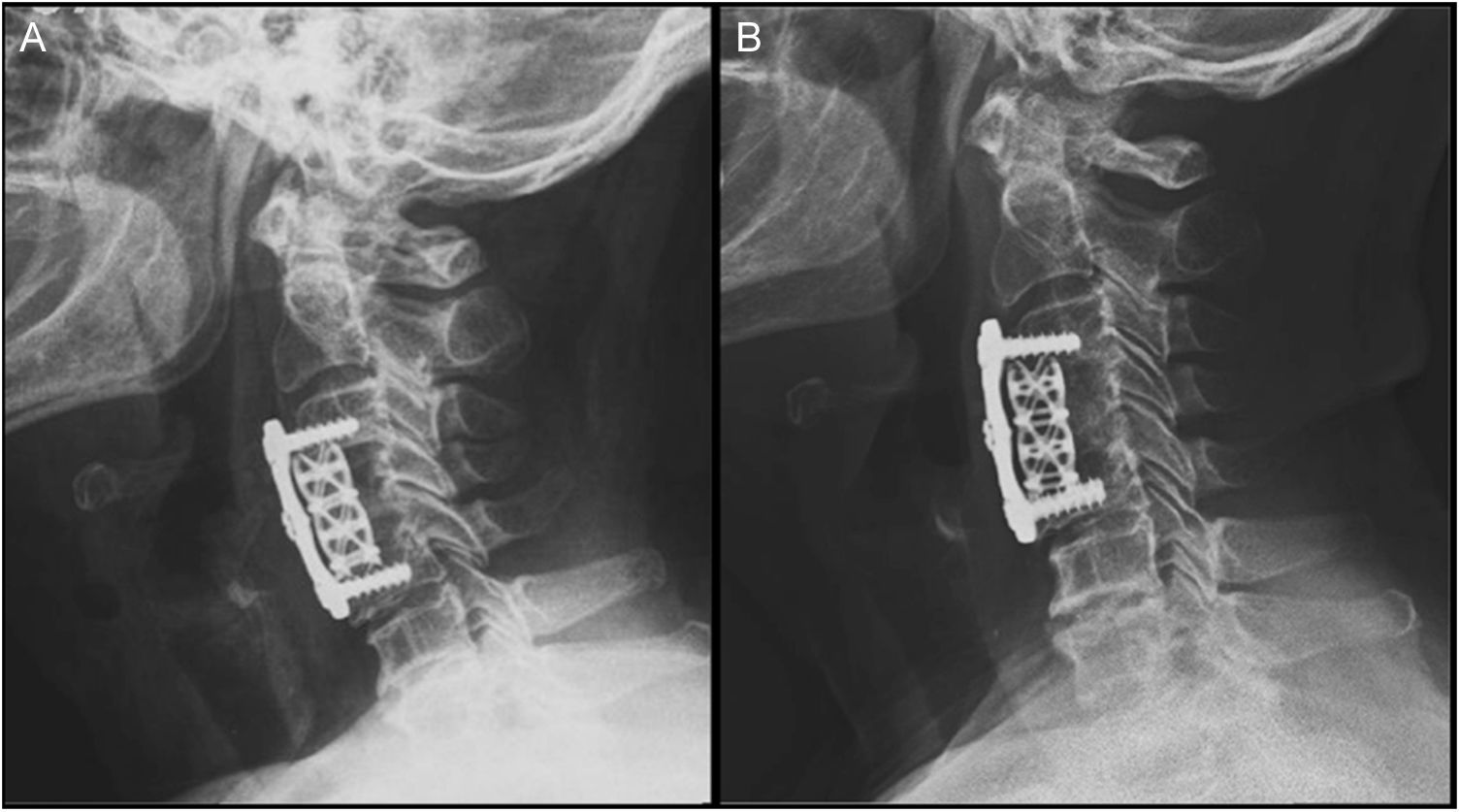
The minimum immediate postoperative subsidence was 0mm and the maximum was 8.21mm, the mean was 2.69±2.80. Postoperative subsidence at 4 years was a minimum of 4.35mm and a maximum of 9.18mm, the mean was 6.11±1.61. In this correlation there was a p=0.0001 with 96%CI −4.57 to −2.28 (Table 1, Fig. 1).
Five patients were found with immediate postoperative subsidence; the patient with the most subsidence at 8.21mm had a total subsidence at 4 years of 9.18mm, the difference was only 0.97mm and their Nürick grade was 4, with no changes during the preoperative period or at 4 years. Three of the patients had an initial subsidence of 2.4, 1.8 and 3mm, and a final subsidence of 6, 6 and 5.6mm, respectively, and had improved Nürick grades of 3 to 1, 4 to 3 and 3 to 2, respectively, and only one of them, with immediate postoperative subsidence went from 3.84 to 7.3mm in 4 years, with a poorer Nürick grade of 3. No immediate postoperative subsidence was found in 2 patients; however, their subsidence at 4 years was 4.7mm and 4.5mm, and both Nürick grades increased by one point, from 3 to 4. Using Spearman's test, a relationship was observed between postoperative subsidence at 4 years and Nürick grade at 4 years, but was not statistically significant.
DiscussionIt was found in this study that most of the patients studied were female (71.4%), in contrast to the study undertaken by Chen et al.19 who found that most of their patients were male (57.66%).
However, we coincide with these authors in that the most common level for corpectomy was C5: 57.1% of the patients in our study and 49.33% of those in the study by Chen et al.19
The only complication was the formation of a haematoma in the surgical approach in one patient, which was surgically drained, with a favourable outcome. This complication is reported by Paradells et al.29 as very rare in this type of approach.
Bone union outside the mesh cage was observed in all cases, especially in the portion posterior to it and its lateral areas. But we were not able to observe the same inside the mesh cages, due to the disadvantage of assessment by X-ray alone. We consider, therefore, that a weakness of our study is that the patients were not assessed by CAT scan at the end of the study, unlike Lee and Sung30 who used CAT and x-ray assessment for a comprehensive evaluation.
The mean surgery time was 153.57±40.28 and the mean transoperative bleeding was 200±57.73, equivalent to the meta-analysis by Wen et al.31 who compare anterior discectomy with corpectomy, with similar results to ours in these parameters.
On comparing the preoperative NDI, with a mean of 30.01±24.32, and the postoperative NDI at 4 years with a mean of 32.05±16.90, a p=0.801 was observed, which is not significant. This is explained because the NDI essentially assesses axial pain and not functional status, which is given on the Nürick myelopathy scale.
Correlation of the myelopathic assessment with preoperative Nürick had a mean of 3.28±0.48 and at 4-year follow-up presented a mean of 3.14±1.21, with a p=0.766, without being statistically significant, unlike that found by Bilbao et al.32 who found in a study of 71 patients an improvement of 62% on the Nürick scale, and observed that while the Nürick grade was lower, the patients achieved greater improvement. The patients in our study had severe myelopathic disorders, which would explain why they did not achieve significant improvement.
Preoperative cervical lordosis, with a mean of 14.42±8.03, correlated with the mean at 4 years of 17±11.67, with a p=0.666; although this is not statistically significant, we can assume that with a small sample size (7 patients) the difference would have to be very high to have any significance. In their study, Jang et al.33 observed an increase in lordosis at the end of their follow-up compared to the immediate postoperative period. This indicates that subsequent subsidence of the mesh cage causes an increase in lordosis.
The immediate postoperative subsidence, with a mean of 2.69±2.80, correlated with the subsidence at 48 months, with a mean of 6.11±1.61, a p=0.0001 was obtained, a similar result to that of Chen et al.19 who obtained an incidence of subsidence of 79.7%. Likewise, Jang et al.33 obtained a subsidence of 93.3% in the patients in their study.
Chen et al.19 also mention that the patients with moderate subsidence (60.7%) presented no significant clinical changes, but the group of patients with severe subsidence (19%) correlated with unfavourable neurological outcomes and complications associated with the subsidence.
We observed subsidences in the immediate postoperative period, which suggests to us that there was a fracture of the platforms that would encourage immediate subsidence in all the patients.
It was observed that the patients who had no immediate postoperative subsidence had depression of the platform of 4mm at the final 4-year follow-up, so we can assume that initial subsidence of the mesh cage does not affect its progress, and also has no probable relationship with the cause of symptoms or predisposition for the subsidence to increase.
There is an association between the Nürick grade at 4 years and postsurgical subsidence at 4 years. However it is not statistically significant, since the sample size is very small, and this is a problem in statistics. We observed a good outcome in 3 patients with an improved Nürick grade, with no relationship with immediate postoperative subsidence. The 2 patients with no initial subsidence had a worse grade by one point at the end of the follow-up period. One patient with initial subsidence also had negative changes by one point on the scale, and the patient who presented the most initial subsidence had no changes in their Nürick grade.
Furthermore, the satisfactory or unfavourable outcomes of the patients relate to the time of onset of the myelopathy, as Tetreault et al.34 mention in their study, the probabilities of a successful outcome reduce the longer the symptoms progress. It was a weakness of our study not to have covered this parameter, since it would be important to consider the duration of the myelopathy prior to surgery due to the presence of irreversible lesions. Other weaknesses of the study are that the sample was small and the variability in brand of material used. However some reports in the international literature have similar samples.
ConclusionSubsidence of the mesh cage is a common phenomenon in this type of procedure, despite the small sample size.
We observed no statistically significant changes between the preoperative and the 4-year postoperative comparisons in lordosis, or Nürick scale and NDI.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Reyes Sánchez AA, Gameros Castañeda LA, Obil Chavarría C, Alpizar Aguirre A, Zárate Kalfópulos B, Rosales-Olivares LM. Resultados a 4 años de seguimiento del tratamiento del conducto cervical estrecho mediante corpectomía, malla de titanio y fijación anterior con placa. Cir Cir. 2017;85:381–386.