Cervical lymphangiomas are uncommon benign congenital malformations usually present in children, and are rare in adults. Currently, complete resection is still the standard care.
Two cases are presented of a cervical lymphangioma in an adult. The diagnosis and surgical approach is also discussed.
Clinical casesCase 1. The first case is a 23 year old male with chief complaint of a tumour in the posterior triangle of the neck, which showed a substantial increase in size in the last 9 months. No associated signs or symptoms, or any trauma history was reported. CT scan of the neck showed images suggestive of a posterior cervical lymphangioma. Exploratory cervical surgery was performed, with complete resection of a cystic tumour located in the posterior triangle of the neck. Surgery was performed without complications and postoperative care was unremarkable. Case 2. The second case is a 28 woman with a cystic tumour in submandibular space. She had history of a previous incomplete operation in another institution 2 years ago, with recurrence of the tumour. A second surgery was performed with complete resection without complications, and with a good outcome.
ConclusionsCervical lymphangioma is a very rare benign disease, surgical treatment is preferred, but sclerotherapy can be used as alternative treatment.
Los linfangiomas de cuello son malformaciones congénitas benignas, poco frecuentes, que se presentan generalmente durante la infancia y son muy raros en los adultos. Su resección completa continúa siendo el tratamiento de elección.
ObjetivoReportar 2 casos de linfangioma cervical en el adulto, presentar el protocolo de estudio y el abordaje quirúrgico realizado.
Casos clínicosCaso 1. Paciente masculino de 23 años de edad, que acude por tumor en triángulo posterior izquierdo de cuello, con aumento progresivo de tamaño en los últimos 9 meses, sin sintomatología asociada ni traumas previos en dicha región. Se realizó tomografía computada de región cervical, que reportó imágenes sugestivas de linfangioma. Se realizó exploración cervical con resección completa del tumor sin incidentes transoperatorios, con evolución satisfactoria. Caso 2. Mujer de 28 años de edad, con tumor quístico submandibular a quien 2 años antes se le practicó una resección incompleta en otra institución. Se le realizó una resección quirúrgica completa del tumor, sin incidentes, y su evolución postoperatoria fue satisfactoria.
ConclusionesEl linfangioma en cuello en el adulto es una enfermedad poco frecuente, benigna. La resección quirúrgica es el tratamiento de elección; se puede utilizar la escleroterapia como tratamiento alternativo.
Cervical lymphangioma is a congenital malformation of the lymphatic system, which triggers the development of a benign cystic tumour and that most often presents in the posterior triangle of the neck.1,2
There are several theories as to their embryological origin. The most accepted of these describes a deficient union of the primary lymphatic spaces with the central lymphatic system as the cause. Another theory suggests deficient development of the venous system and, finally, it is associated with respiratory infections or trivial trauma events.3
These tumours are lymphatic compounds covered by endothelial cells, which develop cysts of various sizes that can haemorrhage or present infections which are confined to the lesion.
They are most common in children between the ages of 3 and 51–4 and rarely present in adults.5 They are generally asymptomatic, can become large in size and patients might not seek attention until adulthood,6 as in our cases. When there are clinical symptoms, these will depend on the location of the tumour; for example, tumours of the neck can be associated with dysphagia or respiratory difficulty, which might even be an indication for emergency surgery.3
The treatment of choice is complete surgical resection, although other treatment alternatives are reported, one of which is sclerotherapy.7
We report the cases of 2 adult patients with large neck lymphangiomas; one in the left posterior triangle and the other in the right submandibular space, which were successfully surgically resected.
Clinical casesCase 1A 23-year-old male patient presenting with a tumour in the left posterior triangle of his neck that had been gradually increasing in size over 9 months. The patient did not report dysphonia, dyspnoea, dysphagia or any other associated symptoms. On examination, a tumour was found in the left posterior triangle of the neck of approximately 15cm×10cm, with smooth surface, defined edges, mobile, painless, with no colour changes and non-pulsatile (Fig. 1).
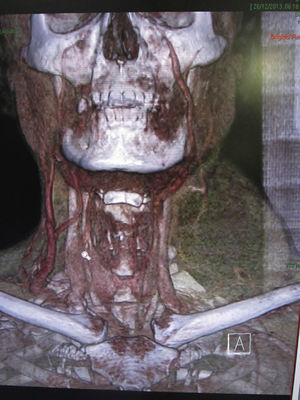
A computed axial tomography scan was performed on the cervical region which reported a tumour with no enhancement of its walls, with some vascular routes on its periphery, totally obliterating the left posterior cervical space and displacing the paraspinal muscles medially, anterior to the submandibular gland and antero-lateral to the sternocleidomastoid, which was slightly compressing the carotid space medially, with homogenous lymph glands, the smallest were 15mm, in both jugulodigastric regions. Tomography concluded images suggestive of lymphangioma of the posterior cervical space (Fig. 2).
Case 1. Axial computed tomography of the left neck, showing a tumour of multilocular cystic appearance, showing no enhancement of its walls, with some vascular routes on its periphery, totally obliterating the left posterior cervical space and medially displacing the paraspinal muscles, anterior to the submandibular gland and antero-lateral to the sternocleidomastoid, slightly compressing the carotid space medially, with homogenous lymph nodes, the smallest being 15mm, in both jugulodigastric regions.
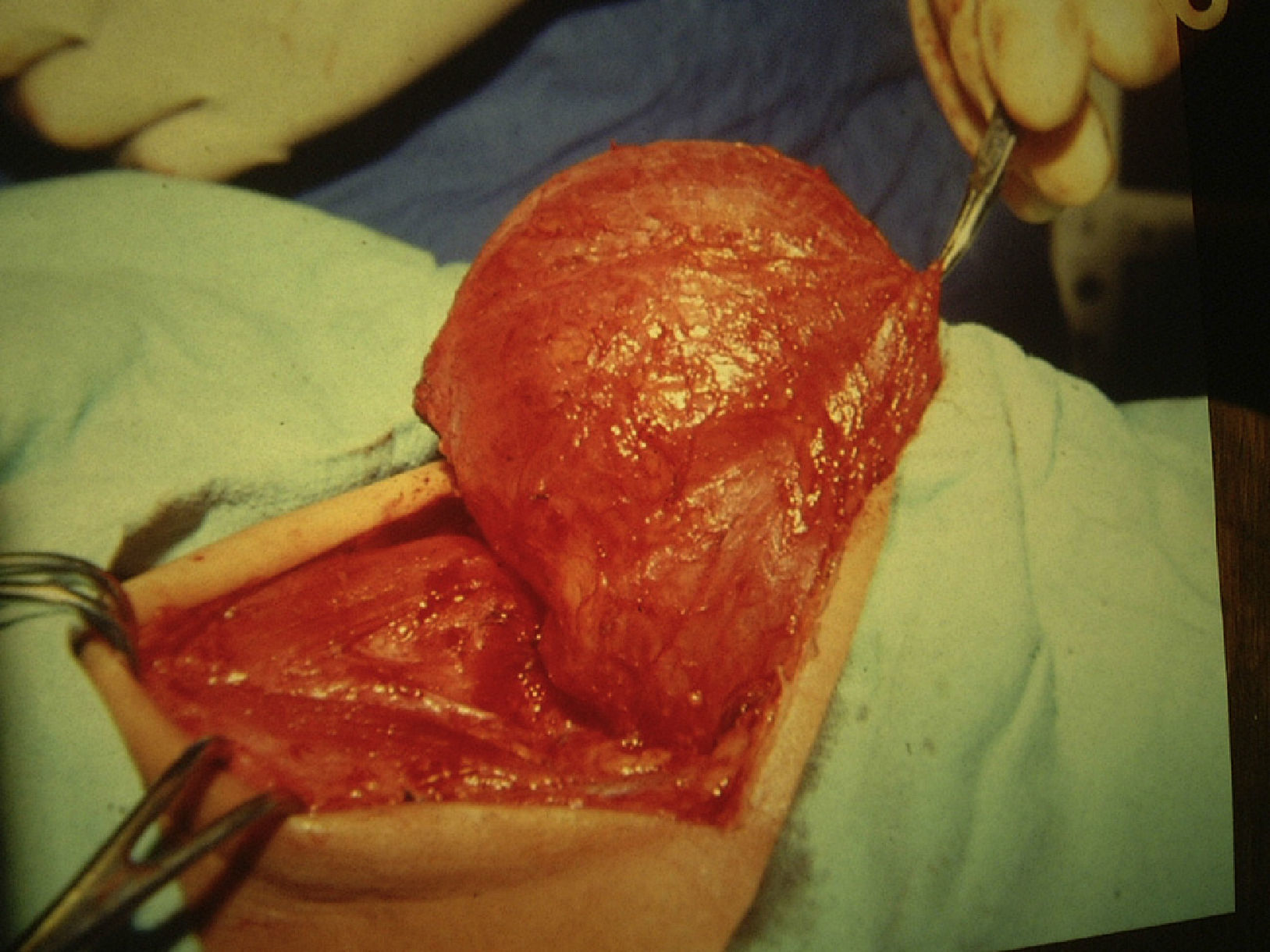
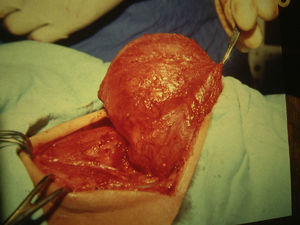
Surgical examination of the neck revealed a cystic tumour in the left posterior triangle of the neck, of approximately 20cm in diameter, in contact with the external, internal jugular vein and spinal nerve, which were preserved. A complete dissection was performed with harmonic scalpel (Focus™ forceps), the lymph nodes closest to the thoracic duct were clipped; the tumour was completely resected. A closed drenovac™ drain was placed and the wound was closed on 2 planes. Histopathological study confirmed the diagnosis of cystic lymphangioma.
The patient made satisfactory progress postoperatively (Fig. 3). One year later, the post-operative outcome was satisfactory; the patient only reported paresthesia at the area of the trapezius muscle on the operated side, due to dissection of the spinal nerve that did not affect the mobility of the shoulder, which was appropriate. There have been no further complications or recurrence to date.
Case 2A 28-year-old female patient presenting a tumour in the right submandibular region. The patient was asymptomatic, with a history of surgery 2 years previously in a different institution. Three months after surgery the patient presented recurrence with gradual and painless growth of the tumour until it had reached the size at which the patient was admitted to our hospital; she did not report signs of pain, fever, skin changes. The type of surgery she had undergone was unknown (she was operated in a different institution and had no clinical summary). On physical examination we found a cystic tumour in the right submandibular region of 12cm×10cm; it was painless and she had a surgical scar (Fig. 4). An ultrasound was performed and the submandibular cystic tumour corroborated. The patient was operated, the previous scar was resected and the tumour completely removed without incident (Fig. 5), a closed drain was placed and the wound was closed. The postoperative outcome was satisfactory (Fig. 6). The histopathological report confirmed the diagnosis of cystic lymphangioma.
The drain was removed on the fourth postoperative day, with no complications.
The patient made satisfactory progress after 5 years’ follow-up and only reported mild submandibular paresthesia, which did not affect salivation or taste. Mobility of the neck was appropriate and the marginal branch of the facial nerve was not affected.
The patient did not present recurrence of the tumour.
DiscussionLymphangiomas of the neck are rare, benign, congenital malformations which are most common in childhood.1,2,4 Ninety percent of lymphangiomas present in children under 2, with an incidence of 1.2–2.8 per 100,000 newborns.2,3 They rarely present in adults.5,6
The most common location is the posterior triangle of the neck (75% of cases), such as the first case presented; 20% in the submandibular triangle, as in the second case, and 5% can present in the abdomen, retroperitoneum, mediastinum and even in multiple locations.8–11
They are classified according to the size of the vessels involved into: capillary, generally located in the subcutaneous tissue; cavernous, located on the tongue and mouth; cystic, also called cystic hygromas, which present most commonly in the neck.12
The clinical presentation depends on their location. Lymphangiomas of the neck are generally renitent, with no other signs or symptoms. They can occasionally cause symptoms due to compression of organs, which can manifest as dysphagia when the oesophagus is compressed and dyspnoea when the trachea is compressed.
The diagnostic study of choice is computed tomography, to assess the lymphangioma and it also enables the surgical approach to be chosen.
The usual surgical findings are: a hypodense tumour, which might be multilocular, with a thin capsule with no reinforcement of its walls with the contrast medium, which might displace adjacent structures,12 as can be seen in Fig. 2.
Ultrasound can show: a hypoechoic tumour, with trabeculae which might indicate its relationship with the adjacent structures.
Complete resection of the tumour remains the treatment of choice, principally in loculated tumours.2,13,14 In the cases presented, despite the fact that one case presented a large, multiloculated tumour, which it was possible to completely resect without prior puncture, the structures near the tumour were preserved and there was no neurovascular injury, due to the valuable information provided by computed axial tomography of the neck that was performed preoperatively, enabling us to plan the correct approach with regard to the dissection plane and to identify the structures in contact with the tumour.
The approach incision should always be made on folds to ensure an appropriate final cosmetic result. It is also important to dissect and preserve the nerves and blood vessels during the procedure. The approach incisions used in the patients we present preserved the spinal nerve, the external and internal jugular vein and the brachial plexus along with other elements that were in intimate contact with the tumour. Preoperative planning enabled us to use the harmonic scalpel (Focus™ forceps) for less blood loss and to save surgical time. It is very important that the lymphatic vessel or vessels near the thoracic duct are always identified; these should be clipped and sectioned, to prevent seromas and, in particular, recurrences.
Case 2 was a submandibular lymphangioma, operated in a different hospital, which recurred early in the postoperative period. This implies that it was not completely resected because a second operation was required, made difficult because of the previous surgical management, although it was possible to resect it completely, and also clip the main lymph vessels which were feeding the tumour.
In both cases the postoperative outcome was appropriate, the drain was removed when the drainage was less than 25ml in 24h and there had been no recurrence; this is the case to date.
Another treatment alternative is video-assisted surgical resection, using a minimally invasive approach, appropriate exposure for dissection is reported, which is safe and feasible with a good cosmetic effect.15
Another treatment method is sclerotherapy. Various substances have been proposed for this, for example: intralesional bleomycin injection has been used to treat tumours which are also largely invading neighbouring organs, the aim being to reduce both the size of the tumour and damage to neighbouring organs. In a study which used intralesional bleomycin injection, complete reduction was reported in 47% of cases, with partial reduction in more than 50%, with 42.9% morbidity.7,16
The most frequently reported complications are: infection, haemorrhage, haematoma, seroma and injury to the nerves in the region.1 The cases we report did not present any of these complications. We prefer to leave closed drains routinely in large tumours in the neck, to prevent the collection of lymph and the development of seromas.
Antibiotics were not used in either of our cases in the postoperative period, because we consider the operations clean. If indicated, the prophylactic administration of a dose of antibiotic could be used 30min prior to the start of the operation.
ConclusionsLymphangioma in the cervical region in adults is a rare, benign malformation which can be easily diagnosed.2,3 Axial computed tomography or magnetic resonance imaging of the neck are the studies of first choice, as they enable the surgical approach to be planned appropriately. At present, surgical resection of the lymphangioma is the treatment of choice, due to its low mortality and recurrence rate.2,14,15,17
An incision which enables adequate exposure of the lymphangioma and adjacent structures should always be attempted, and one which also offers an appropriate aesthetic result. Sclerotherapy can be tried as an alternative treatment.7,16
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Basurto-Kuba EOP, Hurtado-Lopez LM, Campos-Castillo C, Garcia-Figueroa RB, Figueroa-Tentori D, Pulido-Cejudo A. Linfangioma de cuello en el adulto. Reporte de 2 casos. Cirugía y Cirujanos. 2016;84:313–317.