Evidence of the benefit on propioceptive neuromuscular facilitation for reducing falls in older people does not exist.
ObjectiveThe aim of this study is to evaluate the effects of propioceptive facilitation over falls and biomechanical variables, in comparison to standard treatment and control groups.
Materials and methodsSeries cases comparative for the 24 participants were recruited and randomnly assigned to 3 groups. Group 1, propioceptive neuromuscular facilitation, group 2, standard treatment, and 3 control. Falls and biomechanic variables were measured before and after. χ2 was used for falls and multiple regression for biomechanical variables.
ResultsParticipants had similar falls in previous year. Women had higher falls in a relation 7:1 women–men. After intervention, there was no difference between 3 groups. A correlation exist between muscular strength and gait speed with one foot position time r2=0.67, p=0.02.
ConclusionsImproving 1kg-force of muscular strength of pelvic limb and 0.1m/s in gait speed, balance (unipodal position time) increases balance by 11.3%. After 3 months of intervention group 2 got 7.9kg-force and 0.26m/s of profit, while group 1 had 4.1kg-force and 0.15m/s and control group 2.4kg-force and 0.1m/s.
Los estudios sobre caídas en ancianos no definen claramente el efecto de la facilitación neuromuscular propioceptiva para reducir sus caídas y sus variables asociadas.
ObjetivoEvaluar los efectos de la facilitación propioceptiva sobre caídas y las variables biomecánicas relacionadas con la marcha en ancianos.
Material y métodosSeries de casos comparativas en las que participaron 24 pacientes, quienes se asignaron aleatorizadamente a 3 grupos de 8 participantes: grupo 1, tratamiento de facilitación neuromuscular propioceptiva; grupo 2, tratamiento estándar, y grupo 3, testigo. Se midieron las caídas y variables biomecánicas relacionadas con: fuerza muscular, velocidad de marcha, cinestesia, tiempo de posición unipodal y tiempo de reacción muscular. Se aplicó chi2 y regresión múltiple en las variables en estudio.
ResultadosLos grupos fueron equivalentes en la edad y en caídas durante el año previo (p=0.20). Las caídas fueron más frecuentes en las mujeres en una relación 7:1. Posterior a la intervención, existió una disminución significativa en la caída de los participantes de los 3 grupos. Existió correlación entre la fuerza muscular y velocidad de marcha con el tiempo de posición unipodal (r2=0.67; p=0.02).
ConclusionesAumentando 1kg-fuerza del miembro pélvico y 0.1m/s en la velocidad de marcha mejora el equilibrio (tiempo de posición unipodal) un 11.3%. Posterior a 3 meses de la intervención el grupo 2 obtuvo un aumento de 7.9kg-fuerza y 0.26m/s, mientras que el grupo 1 obtuvo 4.1kg-fuerza y 0.15m/s, y el grupo control tuvo 2.4kg-fuerza y 0.1m/s.
Falls are “involuntary events whereby one loses one's balance and falls to the ground or another firm surface which breaks that fall”. There are many reasons for falls and they should be considered as a public health problem.1 37 million falls requiring medical attention are reported annually. Their incidence in the elderly ranges from 25% to 35%; Prevalence ranges from 30% to 50%. The female-male ratio in adults is 2.7–1 and the probability of recurrent falls in people with a history of falls is 52%.2 It is a frequent event amongst the elderly.
In Mexico there are 8.8 million people over the age of 60, and it is expected that this will rise to 15 million in 2020.3,4 Falls represent 30% of the causes of death. However, 10–35% of falls lead to fractures and of these, a hip fracture is the most common (10%),5,6 with a 5 year survival rate of almost 80%.7–17
Several publications list risk factors involved in suffering from falls such as: a history of falls, mobility difficulties, insufficient visual abilities and balance, cognitive deterioration, living in an old peoples’ home, reduced functional independence, fear of falling, depression, anti-arrhythmic medication and psychotropic drugs.7–15
There is a close association between the balance of the musculoskeletal system and the risk of presenting with a fall.10,18–20 It has also been shown that balance has no lineal correlation with age.10,20–22
Despite the importance of falls on the quality of life and in association with increased morbidity and mortality in the elderly, no alternative methods, such as proprioceptive neuromuscular facilitation,13,23–25 have been explored against standard procedures based on the use of flexibility and muscular strength.5,10–12,17,19,22,26–29
The aim of our study is therefore to evaluate the affectivity of proprioceptive neuromuscular facilitation, comparing it with standard treatment used for the prevention of falls in the elderly.
Material and methodsA comparative case series with 24 participants in the study who were randomly assigned to 3 groups, with 4 men and 5 women in each one. Group 1, proprioceptive neuromuscular facilitation, group 2, standard treatment, and group 3 control group.
At the start of the assessment clinical and epidemiological variables were measured which included: age, characteristics of the home, educational level, mental state tests, depression and fear of falling. Data was also collected regarding: weight, height, and body mass index.
The following were measured before and after treatment: falls, muscular strength biomechanical variables with dynamometry, gait speed (standard test), synaesthesia (digital goniometry), one foot position time and time of muscular reaction (reaction to computerised visual and auditory stimulae).
The procedures, risks and benefits were explained in detail to each patient and their written consent to participate was obtained, in accordance with the Code of Helsinki and legislation governing health in Mexico.
The study was submitted to the Comité de Bioética del Hospital General de Zona del Instituto de Seguridad Social para Trabajadores del Estado, León, Guanajuato, Mexico.
The χ2 test was used for statistical analysis to assess differences between groups and a correlation model for associating the muscular and skeletal variables with the number of falls. The statistical programme Epi Dat 7.0 Stat was used. The statistically significant level was fixed at an alfa of 95%.
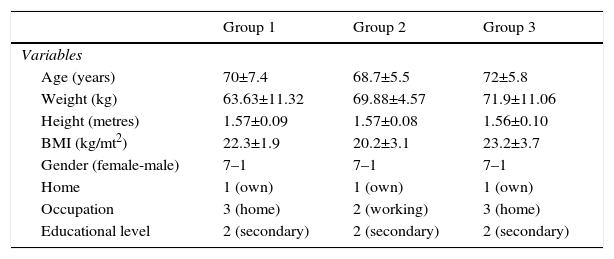
ResultsThe 3 groups were the same at the start of the study in age variables (p=0.35), falls in the previous year (p=0.15) and gender (ratio 7:1 female-male) (Table 1). This table also shows values which were not statistically significant in the type of home, educational level, mental state, depression, fear of falling.
Descriptive statistics of the 3 groups. Descriptive characteristics of the participants.
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Variables | |||
| Age (years) | 70±7.4 | 68.7±5.5 | 72±5.8 |
| Weight (kg) | 63.63±11.32 | 69.88±4.57 | 71.9±11.06 |
| Height (metres) | 1.57±0.09 | 1.57±0.08 | 1.56±0.10 |
| BMI (kg/mt2) | 22.3±1.9 | 20.2±3.1 | 23.2±3.7 |
| Gender (female-male) | 7–1 | 7–1 | 7–1 |
| Home | 1 (own) | 1 (own) | 1 (own) |
| Occupation | 3 (home) | 2 (working) | 3 (home) |
| Educational level | 2 (secondary) | 2 (secondary) | 2 (secondary) |
| Baseline | Final | Delta | Baseline | Final | Delta | Baseline | Final | Delta | |
|---|---|---|---|---|---|---|---|---|---|
| Falls | 2.6±1.0 | 0.5±0.8 | −2.3 | 3±1.3 | 2.3±3.1 | −1.9 | 3.3±1.3 | 1.6±1.0 | −0.5 |
(X+DE). The qualitative variables are reported in absolute values.
BMI, body mass index.
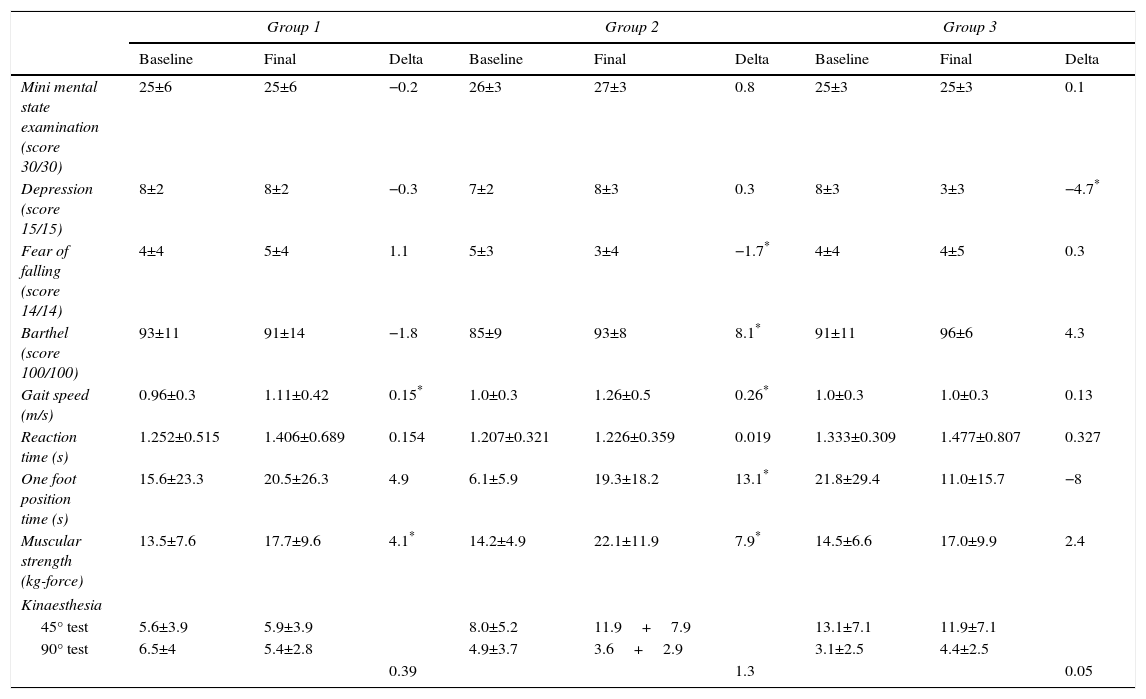
Gait speed was discreetly higher in group 2, compared with groups 1 and 3, with statistical significance for groups 1 and 2. The initial muscular reaction time increased similarly in the 3 groups, which implies clinical deterioration.
Muscular strength increased in the 3 groups, clinically significantly in group 2, with statistical significance for groups 1 and 2. One foot position time in the 3 groups improved and the group with the highest statistical significance was group 2.
Regarding synaesthesia, the 3 groups had values of synaesthesic discrepancy above 3.5°, primarily in the 45° test, which implies clinical deterioration (Table 2).
Descriptive statistics of outcome variables.
| Group 1 | Group 2 | Group 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Final | Delta | Baseline | Final | Delta | Baseline | Final | Delta | |
| Mini mental state examination (score 30/30) | 25±6 | 25±6 | −0.2 | 26±3 | 27±3 | 0.8 | 25±3 | 25±3 | 0.1 |
| Depression (score 15/15) | 8±2 | 8±2 | −0.3 | 7±2 | 8±3 | 0.3 | 8±3 | 3±3 | −4.7* |
| Fear of falling (score 14/14) | 4±4 | 5±4 | 1.1 | 5±3 | 3±4 | −1.7* | 4±4 | 4±5 | 0.3 |
| Barthel (score 100/100) | 93±11 | 91±14 | −1.8 | 85±9 | 93±8 | 8.1* | 91±11 | 96±6 | 4.3 |
| Gait speed (m/s) | 0.96±0.3 | 1.11±0.42 | 0.15* | 1.0±0.3 | 1.26±0.5 | 0.26* | 1.0±0.3 | 1.0±0.3 | 0.13 |
| Reaction time (s) | 1.252±0.515 | 1.406±0.689 | 0.154 | 1.207±0.321 | 1.226±0.359 | 0.019 | 1.333±0.309 | 1.477±0.807 | 0.327 |
| One foot position time (s) | 15.6±23.3 | 20.5±26.3 | 4.9 | 6.1±5.9 | 19.3±18.2 | 13.1* | 21.8±29.4 | 11.0±15.7 | −8 |
| Muscular strength (kg-force) | 13.5±7.6 | 17.7±9.6 | 4.1* | 14.2±4.9 | 22.1±11.9 | 7.9* | 14.5±6.6 | 17.0±9.9 | 2.4 |
| Kinaesthesia | |||||||||
| 45° test | 5.6±3.9 | 5.9±3.9 | 8.0±5.2 | 11.9+7.9 | 13.1±7.1 | 11.9±7.1 | |||
| 90° test | 6.5±4 | 5.4±2.8 | 4.9±3.7 | 3.6+2.9 | 3.1±2.5 | 4.4±2.5 | |||
| 0.39 | 1.3 | 0.05 | |||||||
Variables reported with mean and standard deviation.
In kinaesthesia, delta is the average of the 45° and 90° tests.
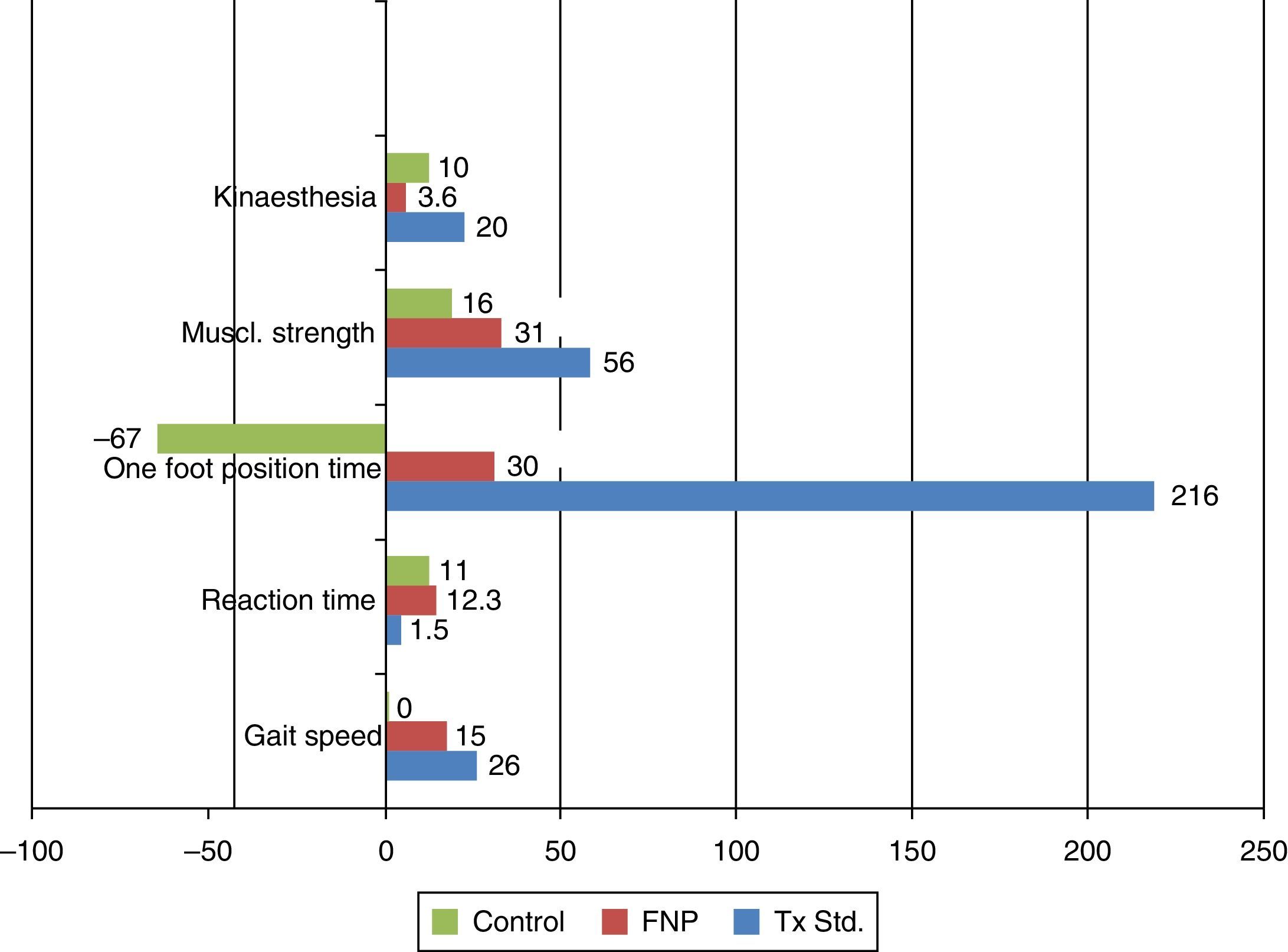
For the variable gait speed, group 1 increased by 15%, starting at a mean of 0.96m/s and finishing at 1.11m/s with a coefficient of variation (CV) of 0.93. Group 2 improved by 26%, starting at 1m/s and finishing at 1.26m/s and with a CV of 1.1. Group 3 started at 1.1m/s and finished at 1.23m/s, improving by 1.1%, with a CV of 1.25. Regarding the difference of before–after means, group 2 had the greatest difference with 0.26m/s (CI 95: 0.05–0.47), whilst group 1 had a difference of 0.15m/s (CI 95: 0.05–0.25); the difference in group 3 was 0.16m/s (CI 95: 0.02–0.3).
Regarding the muscular reaction time variable, in group 1 this increased by 12.3%, starting at 1.252ms and finishing at 1.406s with a CV of 3.44; in group 2 this increased by 1.5%, starting at 1.207 and finishing at 1.226s, with a CV of 23.68; the control group started at 1.333s and finished at 1.477s, increasing by 11%, with a CV of 1.54. The group with the least difference of means was group 2 with 0.019s (CI 95: 0.293–0.769), whilst the difference in group 1 was 0.154s (CI 95: 0.214–0.522) and group 3 had 0.144s (CI 95: 0.046–1.339).
In the one foot position time variable, group 1 increased its time by 30%, starting at 15.6s and finishing at 20.4s, with a CV of 7.26; group 2 improved by 21.6%, starting at 6.08 and ending at 19.26s, with a CV of 1.44, and the control group reduced its time by 67%, starting at 16.3 and finishing at 10.9s, with a CV of 4.38. The highest differences of means was for group 2 with 13.1s (CI 95: 0.02–26.18); for group 1 the difference was 4.7s (CI 95%: −18.9 to 29.3) and for the control group it was −5.3s (CI 95: −21.4 to 10.8).
For the muscular strength variable group 1 increased by 31%, starting at 13.4kg-force and finishing at 17.6kg-force, with a CV of 1.28; group 2 increased by 56%, starting at 14.7kg-force and finishing at 22.1kg-force with a CV of 1.48, and group 3 increased by 16%, starting at 14.5kg-force and finishing at 16.9kg-force, with a CV of 1.73. The greatest difference of means was for group 2 with 7.9kg-force (CI 95%: −0.2 to 16.0), whilst group 1 had 4.1kg-force (CI 95: 0.47–7.73), and group 3 had 2.4kg-force (CI 95: −0.48 to 5.28).
In the synaesthesia variable, group 1 increased its levels of discrepancy by 3.6%, starting at 6.05° of error and finishing at 6.25°, the average between the tests at 45° and 90°, with a CV of 19.32; group 2 had an increase of 20.2%, starting at 6.48° of error and finishing at 7.8° as an average of the 2 tests, with a CV of 2.28; and group 3 increased by 10%, starting with 7.35° and finishing at 8.15° of error, with a CV of 2.46. The least difference in means was for group 1 with 0.20° (CI 95: −2.35° to 2.73°), group 2 had 1.31° (CI 95: −0.76° to 3.38°), and group 3 had 0.80° (CI 95: 0.57–2.17°) all intervals and means were transferred.
In the multiple regression model the one foot position time (balance) was associated with muscular strength and gait speed where an r2 of 0.67 and p=0.02 was obtained.
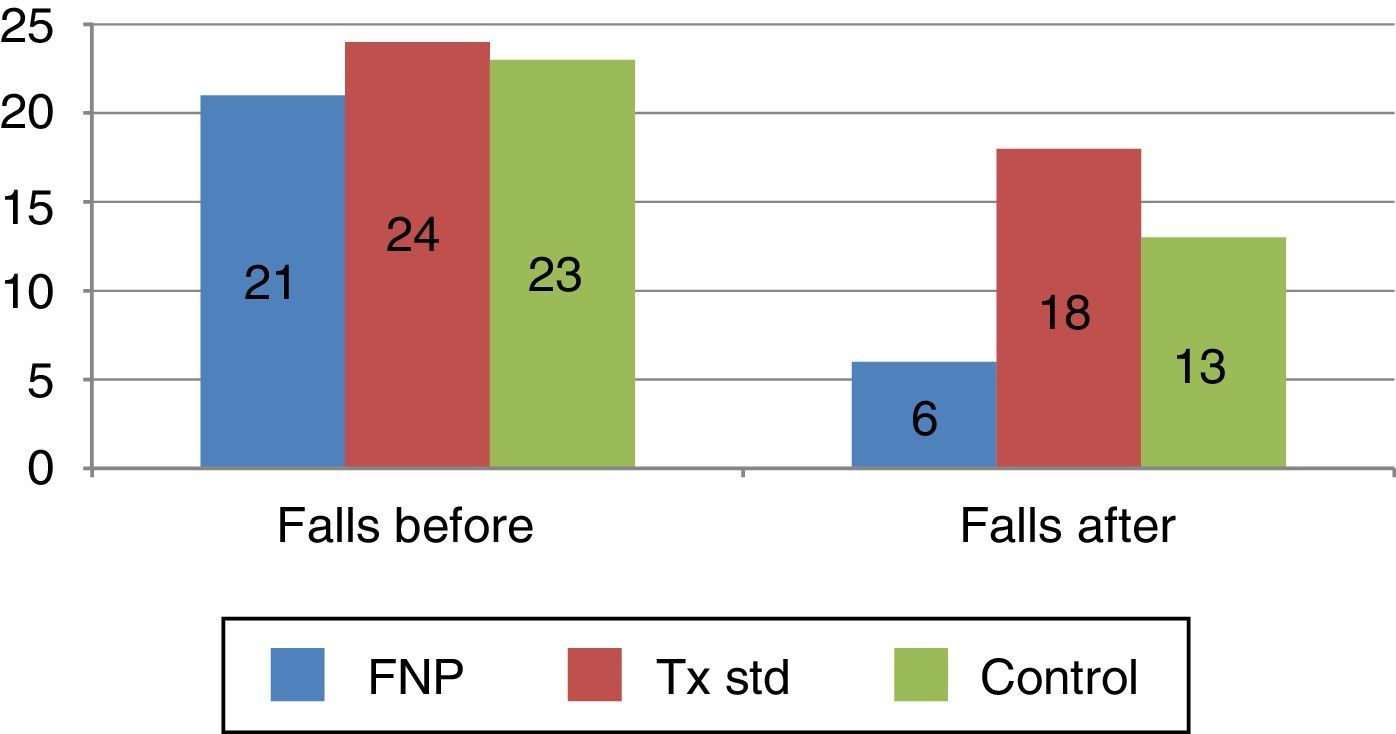
50% of the participants had 2 or more falls in groups 1 and 2, group 3 had 75% in a year prior to the study (Figs. 1 and 2).
There was a lower number of falls among the participants of group 1 (37%) compared with the other groups, who had a 62%, difference which was of statistical significance.
DiscussionAlthough the prevalence of falls in the 3 groups stayed within the range of that reported in published literature, i.e. from 30% to 50%, there was a clinical difference between the 2 groups who received intervention and the control group. Only 12% of participants in groups 1 and 2 had 2 or more falls in 6 months, whilst in group 3 62% did.
The participants of group 1 started with 21 falls in the previous year and finished with 6 falls, with an expected frequency for 6 months of 10.5 falls. Falls fell by 57% in this group. Group 2 started with 24 falls in the year prior to the study and finished with 18 falls in the 6 months, 50% more than expected. Group 3 started with 23 falls in the previous year and finished with 13 falls in 6 months. 16.5 falls had been expected for 6 months and fell by 28%.
In accordance with the study, with an increase of 1kg-force of the pelvic limb and 0.126m/s in gait speed, balance increased (time standing on one leg) by 11.3%; in the standard treatment (group 2) an increase of 7.9kg-force was obtained and in group 1 with the proprioceptive neuromuscular facilitation 0.26m/s, 4kg-force and 0.15m/s was obtained during the 3 months of treatment.
Domínguez-Carrillo et al.12 indicate that time standing on one leg lower than 30s is a predisposing factor for falls. In this study, group 2 was the most effecting in altering this variable on increasing it by 216% compared with 30% in group 1.
It is interesting to highlight that in the 3 groups assessed, the highest kinaesthesia error was presented in the 45° test, almost doubling the error value compared with the 90° test; several probable causes are that the 45° position requires greater muscular strength to maintain it, combined with the pain of arthritis of the knee of the participants assessed. Coronado-Zarco et al.13 mention that the discrepancy over 3.7° in execution of the kinaesthetic knee tests is a factor for suffering 2 or more falls per year. Group 2 was the only one where the mean was lower for this parameter after 3 months intervention with 3.6° of discrepancy in the 90° test. However, comparing baseline and final measurement of this group, there was an increase of 20%. The group which best controlled this outcome over time was group 1, with just 3.6% baseline to the end and with a mean of 5.4° in the 90° test.
In accordance with the outcome of each treatment, it is possible to deduce several observations regarding their efficacy in certain variables:
In group 1, the discrepancy of the kinaesthesia (3.6%) was controlled during the time of research, whilst in groups 2 and 3 there were increases in levels of discrepancy (20% and 10%, respectively). Thus, also in group 1 muscular strength of the pelvic limb was increased in the pattern of complete extension by 31% (p=0.040), and la gait speed by 15% (p=0.04).
Group 2 obtained the best outcome in the time for standing on one leg, with 216% (p=0.02). Thus there was also an improvement in muscular strength with 56% (p=0.002) and gait speed 26% (p=0.003).
One factor which may play a part in the outcome of the variables studied is receiving group therapy, since there may be a certain amount of coerciveness amongst the participants. According to Burke et al.30 this may result in a total effect of 0.28 (CI 95%: 0.20–0.35) in variables involved.
In group 3, one probable explanation of the gain in 16% of muscular strength is due to the variable “occupation” with a home mean=3 and cognitive state=25, final depression under the 3 groups with a mean=3 points and higher score of final functional autonomy in the 3 groups with a mean=96 (Barthel); however, in the variables gait speed, one foot position time, reaction time and kinaesthesia this group deteriorated during the 3 month period.
ConclusionsGroup 1 had the best outcome in falls at 6 months, but clinical improvement in the other variables was mainly to be found in group 2.
In this study, the most important components associated with balance are muscular strength and gait speed. A significant correlation was found and standard treatment was what most effectively modified these parameters.
The observed outcomes have enabled us to distinguish that proprioceptive neuromuscular facilitation treatment controls kinaesthesia, whilst standard treatment changes muscular strength and gait speed and, finally, that each patient's balance plays a part in falls or risk factors for falls.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to think the elderly participants from the city of León (Guanajuato); the managers of the Hospital Regional, Instituto de Seguridad y Servicio Social de los Trabajadores del Estado (ISSSTE-León) for their facilities and the ISSSTE for financing this study, and to all personnel who have assisted us in this clinical research.
Please cite this article as: García-Flores FI, Rivera-Cisneros AE, Sánchez-González JM, Guardado-Mendoza R, Torres-Gutiérrez JL. Correlación entre velocidad de marcha y fuerza muscular con equilibrio para reducir caídas en ancianos. Cir Cir. 2016;84:392–397.