Craniovertebral junction lesions in the paediatric population are associated with a low survival rate, which has declined in recent years. Neurological disability is a major concern due to the high economical cost it represents. Paediatric patients are more susceptible to this lesion because of hyperextension capacity, flat articulation, and increased ligamentous laxity. Survival after these kinds of injuries has been more often reported in adults, but are limited in the paediatric population.
Clinical caseA case of an 8-year-old male is reported with occipitocervical and atlantoaxial dislocation associated with clivus fracture, brain oedema, and post-traumatic subarachnoid haemorrhage. A halo vest system was placed with no traction. One month after the trauma the patient was surgically treated with C1 and C2 trans-articular screws, occipitocervical fixation with plate and screws, and C1–C2 fixation with tricortical bone graft and wires without complication. He has now returned to school and is self-sufficient.
ConclusionsWith better pre-hospital medical care and with improved surgical techniques the mortality rate has declined in this kind of lesion.
Las lesiones traumáticas del complejo occipitoatloaxoideo en población pediátrica están asociadas con menor sobrevida, lo que en años recientes ha disminuido. La secuela neurológica que resulta de estas lesiones es un factor importante por el gran costo económico y emocional que representan. Los pacientes pediátricos son más susceptibles a este tipo de lesiones por la capacidad de hiperextensión, articulaciones planas y laxitud ligamentaria. La sobrevida con este tipo de lesiones se ha reportado mayormente en adultos y muy limitada en la población pediátrica.
Caso clínicoPresentamos el caso de un niño de 8 años de edad con luxación occipitocervical y atlantoaxial asociada con fractura del clivus, edema cerebral y hemorragia subaracnoidea; se aplicó un halo con chaleco sin tracción. Un mes posterior al traumatismo el paciente fue intervenido quirúrgicamente con tornillos transarticulares de C1–C2, fijación occipitocervical con una placa y tornillos, y fijación de C1–C2 con injerto tricortical óseo y alambres, sin ninguna complicación. Actualmente, el paciente acude a la escuela y es autosuficiente.
ConclusionesDebido a la optimización de la atención prehospitalaria y la fusión de técnicas quirúrgicas, se ha logrado disminuir la mortalidad en este tipo de lesiones.
Traumatic dislocation of the occipitoatlantoaxial complex is the consequence of a high-speed mechanism exposure, in general associated with car accidents.1,2 The mortality rate and the neurological sequel have diminished in recent years due to improvement in prehospital care, which includes: cervical spine collar for stabilization, improved ambulance response time and the establishment of standard trauma protocols by the American College of Surgeons.2–4 Overall survival information with these lesions is limited in pediatric population.3,5,6
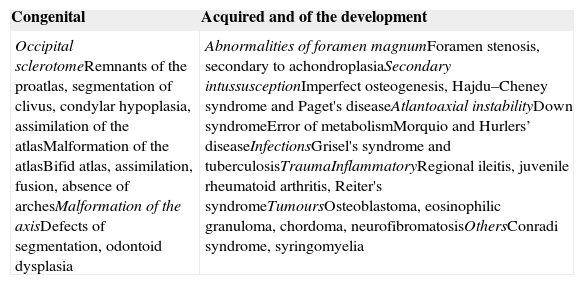
The hyperextension mechanism of the occipito-cervical complex involving the posterior ligaments is the hallmark of this lesion. Paediatric patients are more susceptible to this type of injuries due to their hyperextension, plane articulations and the increased ligamentous laxity.7 In 1960's, survival was reported to be 35%. The abnormalities of the cranio-cervical junction may be classified in congenital and acquired (Table 1).8 The instability of the ligaments, secondary to upper cervical spine trauma can be mainly classified in four groups: occipitocervical dislocation, translation effect, axial and atlantoaxial rotation.9
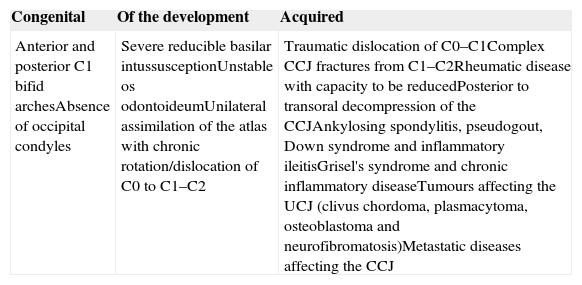
Classification of craniocervical abnormalities.
| Congenital | Acquired and of the development |
|---|---|
| Occipital sclerotomeRemnants of the proatlas, segmentation of clivus, condylar hypoplasia, assimilation of the atlasMalformation of the atlasBifid atlas, assimilation, fusion, absence of archesMalformation of the axisDefects of segmentation, odontoid dysplasia | Abnormalities of foramen magnumForamen stenosis, secondary to achondroplasiaSecondary intussusceptionImperfect osteogenesis, Hajdu–Cheney syndrome and Paget's diseaseAtlantoaxial instabilityDown syndromeError of metabolismMorquio and Hurlers’ diseaseInfectionsGrisel's syndrome and tuberculosisTraumaInflammatoryRegional ileitis, juvenile rheumatoid arthritis, Reiter's syndromeTumoursOsteoblastoma, eosinophilic granuloma, chordoma, neurofibromatosisOthersConradi syndrome, syringomyelia |
The objective of this article is to describe the treatment in a pediatric patient with severe craniocerebral trauma, traumatic occipitocervical and atlantoaxial dislocation with concomitant clivus fracture and with a good neurological outcome.
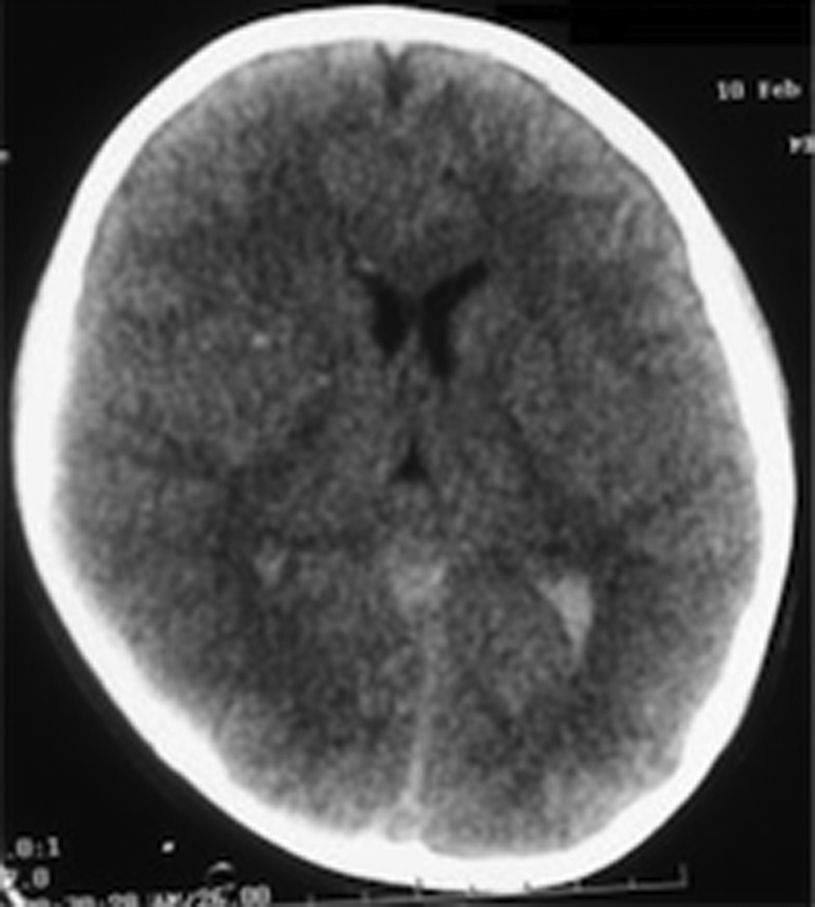
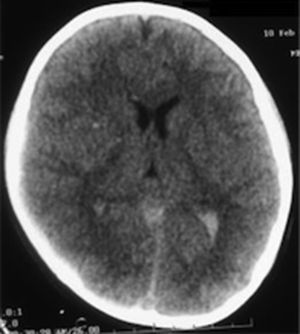
Clinical caseHealthy 8-eight-year-old boy, admitted to the emergency department on 10 February 2008 after a car accident with lateral impact. He was initially transferred to another hospital, where he was stabilised and the airway was secured. Afterwards, he was transferred to the Centro Médico ABC. Campus Observatorio (Mexico City), where he was received by our team. The patient arrived with a score of 6 points in the Glasgow scale and under sedative medication. Diagnosis upon arrival was: severe traumatic brain injury, diffuse axonal injury (grade III), subarachnoid haemorrhage (Fisher IV), right temporal brain contusion, pulmonary contusion, fracture in the first left rib and spleen laceration (grades I–II) (Fig. 1).
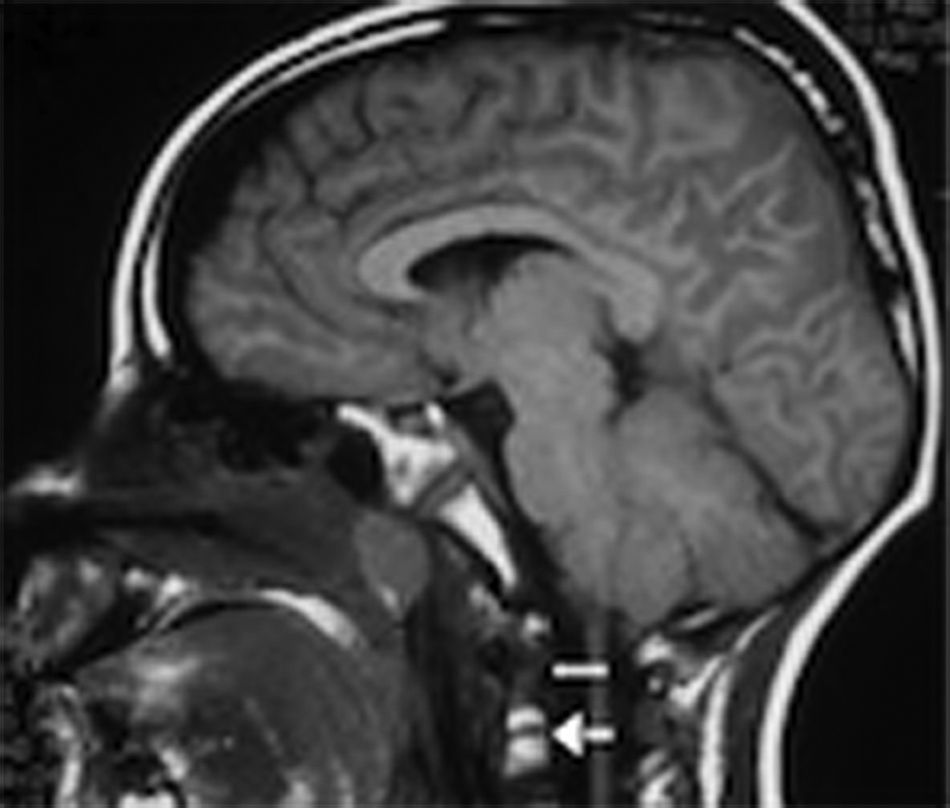
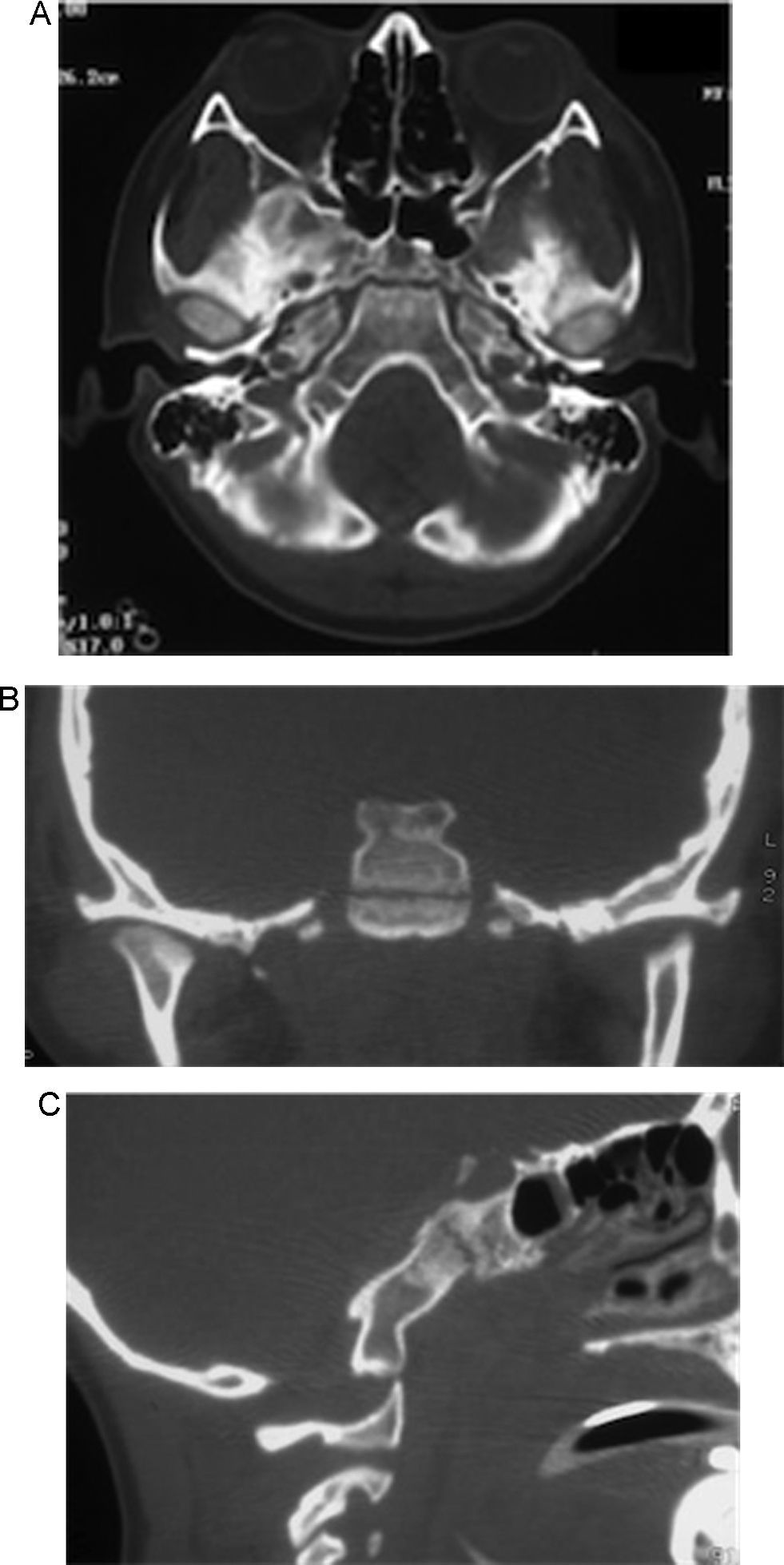
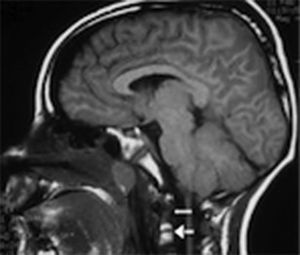
During the first 24h an external ventricular drainage with intracranial pressure monitor was placed. Pharmacological antiedema measures were started; and, regardless of the medical treatment, the intracranial pressure continued increase by three-times higher than normal limits, reaching up to 38cmH2O. Magnetic resonance imaging showed clivus fracture and occipitocervical and atlantoaxial dislocation (Figs. 2 and 3). A bilateral craniectomy was performed 48h after arrival because the patient did not respond to the medical therapy, and even under barbiturate coma (thiopental) he still maintained a high intracranial pressure. Two days after surgery, the intracranial pressure was stabilised in normal values. After 6 days of hospital stay, a halo vest without traction was applied and sedative medication was withdrawn. Subsequently, he developed a sepsis of unknown origin, with negative cultures and good response to antimicrobial therapy. Once without sedation, the patient could initially move the lower limbs, and days later, he moved the four limbs.
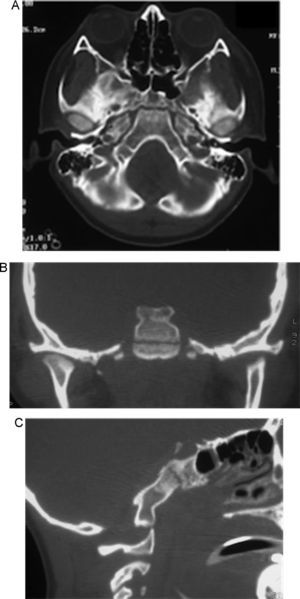
A tracheotomy was performed due to prolonged intubation. The patient obeyed simple orders. One month after the trauma, the occipitocervical fixation was performed with implantation of C1–C2 transarticular screws, plate, tricortical bone grafting and wiring, with no complications (Fig. 4). In the radiologic control studies, no ischaemic or haemorrhagic areas were demonstrated. The progress of the patient continued to be favourable and rehabilitation started with good response. Speech therapy was also started, as the patient was unable to adequately speak and only stammered incomprehensible words. Five weeks after the bilateral craniectomy, bilateral methyl methacrylate cranioplasty was performed.
Two months after the accident, he was discharged and transferred to a neurological rehabilitation facility. His progress has been very favourable. He has returned to normal life, goes to school and is self-sufficient. His speech has significantly improved, and only certain limitations to walk remain.
DiscussionAtlantoaxial instabilityTreatment for this kind of injuries is very limited in the paediatric population, and most experiences come from adult patients. Limited neck muscle development is additional challenging in the surgical technique, because of, the disproportion between head and body and the smaller articulations of the occipitocervical complex.10,11 The most recommended treatment for odontoid fractures is the anterior cervical approach with biplanar fluoroscopy as it manages to greatly preserve the ligaments, the axial rotation and the immediate atlantoaxial fixation with a fusion rate of 92–100%. The complication rate is 9.5% and most of the complications are due to instrumentation material failure. The use of double internal screws in odontoids has not demonstrated a significant biomechanic advantage over the use of one sole screw. There are three essential movements involved in the atlantoaxial joint: flexion, extension and axial rotation. The fixation techniques can be divided into rigid and semi-rigid techniques. In the rigid fixation technique, transarticular screws or screws and rod in C1–C2 are used. In the semi-rigid fixation wires or cables are used.
The indications to perform atlantoaxial arthrodesis depend on the aetiology, which could be congenital, due to development or acquired. The interlaminar wiring and grafting fixation technique described by Brooks and provides a very effective stabilisation of the rotation in the sagittal plane. The bone grafting mechanically prevents extension. This technique preserve axial movement and with a low arthrodesis rate external immobilization is mostly recommended. This treatment is recommended for patients with C1–C2 fixation, due to immature spine. The C1–C2 transarticular screw fixation technique has a high rate of immediate stability in all the movements of the joint.
This procedure is recommended in children older than 9 years. Technically it is very demanding and the surgeon's experience plays a key role in the success of the surgery. The limitations of the surgical technique are mainly caused by the size of C2; and, likewise, there is great risk of injuring the vertebral artery (4.1%). This is why it is necessary to have access to vascular imaging, since a vertebral artery injury is an absolute contraindication. Spine fusion by the lateral masses is indicated when the transarticular fixation cannot be performed due to anatomical variations in the vertebral artery and to a severe thoracic kyphosis.
Occipitocervical fusionThe most common indication to perform an occipitocervical fixation is the occipitocervical instability, which could be congenital or acquired aetiology as shown in Table 2, proposed by Ahmed et al.12 Werne has studied the technique in cadaver specimens to determine the forces necessary to produce a rupture in the tectorial membrane and in the alar ligament and that at the same time may produce an atlantooccipital dislocation.13
Indications for occipitocervical fusion.
| Congenital | Of the development | Acquired |
|---|---|---|
| Anterior and posterior C1 bifid archesAbsence of occipital condyles | Severe reducible basilar intussusceptionUnstable os odontoideumUnilateral assimilation of the atlas with chronic rotation/dislocation of C0 to C1–C2 | Traumatic dislocation of C0–C1Complex CCJ fractures from C1–C2Rheumatic disease with capacity to be reducedPosterior to transoral decompression of the CCJAnkylosing spondylitis, pseudogout, Down syndrome and inflammatory ileitisGrisel's syndrome and chronic inflammatory diseaseTumours affecting the UCJ (clivus chordoma, plasmacytoma, osteoblastoma and neurofibromatosis)Metastatic diseases affecting the CCJ |
C, cervical; CCJ, craniocervical junction.
From Ahmed et al.12
Surgical treatment must be individually selected, being able to extend one or two levels below the axial instability according to the radiographic findings. Bone graft is used to obtain a definitive fusion. The autologous bone grafts have several advantages: they are osteogenic, osteoconductive and osteoinductive; therefore, the immunological incompatibility and the risk of infectious diseases disappear. In the majority of cases iliac crest is used 91%.12,14,15
Donor-site morbidities include: persistent pain in the donor site, myalgia, paraesthesia and local infection of the wound.16 In the paediatric population a quick regeneration of the ribs is observed, for this reason morbidities decrease (3.7%) and the fusion rate is increased (98.8%).17
At present, a limited number of articles on survival in patients with atlantoaxial and atlantoccipital injuries has been published.2,18–21 In the case described, the transarticular fixations and the bone grafting obtained a favourable fusion and survival with minimal neurological sequel.
Intraoperative complications include: venous haemorrhage, vertebral artery lesion and dural lacerations. The bleeding happens mainly during the exhibition of the lateral mass of C1 or C2, and can be prevented by maintaining the subperiosteal plane of dissection. Late complications include infection of the surgical wound and failure of reduction and fusion.12
ConclusionSurvival from atlantoccipital and atlantoaxial injuries have improved with a reduction in the mortality rate and an increase in survival, secondary to an improvement in the prehospital care and the use of protocols for trauma attention. The emergency teams must be familiarised with this type of injuries to avoid delays in the treatment and complications.
Posterior intraarticular fusion offers optimal long-term results in paediatric patients. The spine fusion surgery in the paediatric population is potentially complicated, as it may lead to spinal growth limitations, long-term fusion and spinal deformities. The neuro-rehabilitation programmes are essential for the outcome of the patients.
Conflict of interestThe authors declare that there are no conflicts of interest.
The authors thank Harbey B. Sarnat, MS, MD, FRCPC, Professor of Paediatrics, Pathology, (Neuropathology) and Clinical Neurosciences University of Calgary, School of Medicine, Alberta Children's Hospital for publishing assistance.
Please cite this article as: Herrada-Pineda T, Loyo-Varela M, Revilla-Pacheco F, Uribe-Leitz M, Manrique-Guzmán S. Luxación traumática occipitocervical y atlantoaxial con fractura del clivus en un paciente pediátrico. Reporte de un caso. Cir Cir. 2015; 83: 135–140.