Melanoma is found mainly in the skin and eyes, followed by the anorectal region. In the rectum, melanocytes are located in the anal transition zone and in the squamous zone.1 Primary anorectal melanoma is highly malignant, with increased metastatic capacity; the symptoms are silent and sometimes not visible, as they can be amelanocytic.2 It represents 0.3%-3% of melanomas1 and 1%–3% of anorectal tumors.1,2
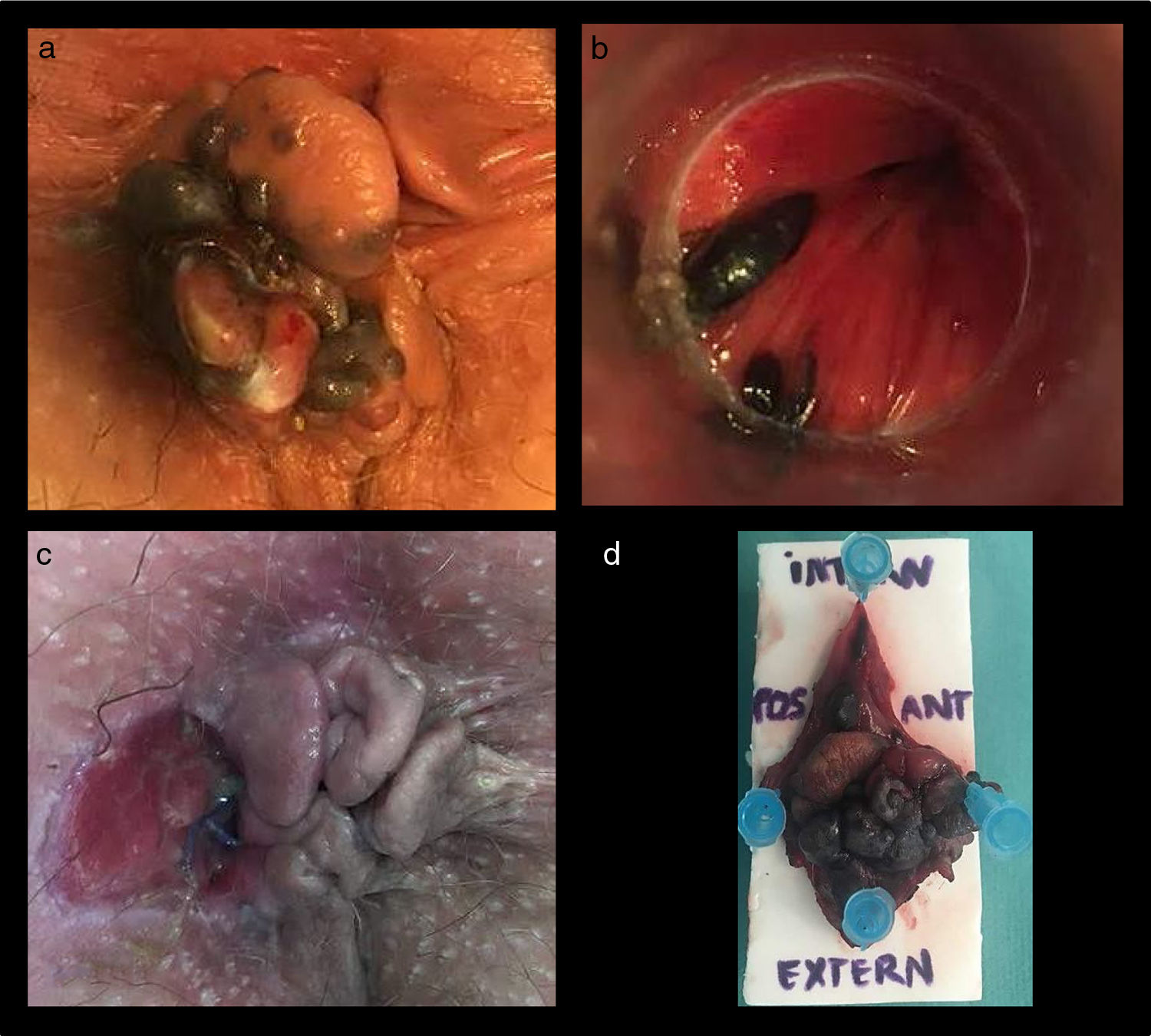
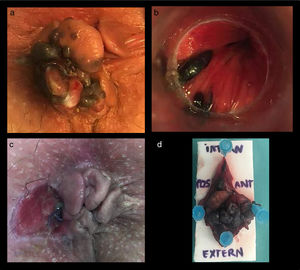
We present the case of a 69-year-old patient with a history of vaginal intraepithelial neoplasia (VIN-III) treated by local resection in 2015, who was disease-free two years later. In the most recent follow-up office visit, perianal skin tags were observed with an inner blackish area that were suspected anal melanoma (Fig. 1a). Anoscopy revealed two pigmented mucosal lesions in the anal canal, predominantly in the left anterior quadrant (Fig. 1b). The pathology study of a biopsy sample reported malignant melanoma. The extension study with rectal magnetic resonance imaging (MRI), thoraco-abdomino-pelvic computed tomography (CT) scan and complete colonoscopy revealed a left perianal pseudonodule measuring 30 × 16 × 13 mm, with no evidence of distant dissemination or sphincter involvement.
En bloc resection (Fig. 1c, d) of the affected area was performed.
The pathology study reported malignant melanoma of the anal canal invading perirectal tissue with free margins, pT3NxMx, and adequate surgical resection margins greater than 1 cm.
After the procedure, the patient began a high-risk clinical follow-up protocol with office visits every 3 months. The first PET/CT revealed a left inguinal lymphadenopathy that was biopsied and identified as metastatic anal melanoma. The patient entered an immunotherapy clinical trial, including nivolumab combined with BMS-986016 (anti-LAG-3).
The initial evolution was favorable, with almost complete regression of the lymphadenopathy in the first two follow-up CT scans. After 17 months of follow-up, the patient presented paraplegia of the lower limbs, and MRI of the medulla revealed leptomeningeal carcinomatosis, a rare form of distant recurrence of this disease. Palliative care was initiated, and the patient died 18 months after the intervention.
1.2% of melanomas are found in the mucosa, and less than 25% of these are anorectal.3 Anal melanoma is a very aggressive disease due to its poor prognosis, and it is considered a systemic disease.
The symptoms are nonspecific, most in the form of rectorrhagia, tenesmus and changes in bowel movements.1 It equally affects men and women, occurring most frequently around the fifth-sixth decades of life and mainly affecting Caucasians.1,4 Up to 60% of patients present metastasis at diagnosis, which is usually limited to regional lymph nodes. They can metastasize to the liver, lungs2 and the central nervous system, representing the third most frequent cause of meningeal carcinomatosis after breast and lung cancer.
Anal melanoma is considered a different pathology from cutaneous melanoma,4 with a specific classification and controversial treatment. While cutaneous melanoma is the result of a malignant transformation of melanocytes exposed to ultraviolet radiation acting as a carcinogenic stimulus, the etiopathogenesis of anal melanoma is not well established.1 It is suggested that patients with HPV and HIV have a higher risk of developing this disease due to the role of immunology in the development of anal melanoma.1,4
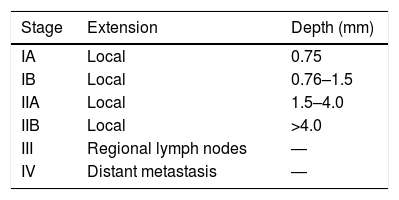
There are two specific staging methods for anorectal melanoma:3,5 that of the American Joint Commission on Cancer Staging for Anorectal Melanoma,1,6 which takes into account both the extent and depth of the lesion (Table 1); and the method based solely on extension (stage 1: localized; stage 2: involvement of regional lymph nodes; stage 3: metastatic disease).1,3
Staging by the American Joint Commission on Cancer Staging System for Anorectal Melanoma1,8
| Stage | Extension | Depth (mm) |
|---|---|---|
| IA | Local | 0.75 |
| IB | Local | 0.76–1.5 |
| IIA | Local | 1.5–4.0 |
| IIB | Local | >4.0 |
| III | Regional lymph nodes | ― |
| IV | Distant metastasis | ― |
Treatment is based on surgery, and the ideal form of treatment is still up for debate: abdominoperineal resection (APR) vs local excision with safety margins (1 cm is considered sufficient when the thickness of the lesion does not exceed 1 mm; otherwise, extension of the margins up to 2 cm has been proposed).4
Unfortunately, there are no randomized controlled studies to evaluate the differences between APR and local excision. However, many studies affirm that, despite its radical nature and better local control of the disease, APR has not been shown to increase patient survival7 and, on the contrary, it increases the comorbidity associated with surgery, worsening quality life.2 Nonetheless, APR is the treatment of choice in cases with sphincter involvement.
Adjuvant radiation therapy (including both iliac and inguinal lymph node chains), chemotherapy, and immunotherapy remain controversial, as they may increase disease-free time, but not overall survival.7,8 However, a recent study has published that the most effective treatment is the combination of surgery and radiotherapy in the case of non-disseminated disease.9,10
Unfortunately, when the disease spreads, the prognosis is very poor, with 5-year survival rates of 0%5 and 18-month median survival rates of 5-7 months with no metastasis at diagnosis.2 The field of immunotherapy looks promising, but is still in the research phase. The drugs in current trials are mostly c-kit inhibitors.
Please cite this article as: Mericahl Resina M, Cerdan Santacruz C, Sierra Grañón E, Tarragona Foradada JA, Olsina Kissler JJ. Melanoma anal, una patología radicalmente distinta al melanoma cutáneo, con un pronóstico infausto. Cir Esp. 2020;98:491–493.