The incidental finding of space-occupying lesions of the liver (either single or multiple) during laparoscopic or conventional surgery that had not been detected on preoperative imaging tests is frequent. Most are small hemangiomas or simple cysts whose macroscopic characteristics reveal their aetiology.1 Less frequently, the lesions are white, nodular, subcapsular and hard, which makes one suspect they are metastases of unknown origin.2–4 Detailed abdominal examination and biopsy of the mass should be carried out. Peribiliary gland hamartomas or bile duct adenomas are benign tumours derived from the epithelium covering the bile ducts; they represent only 1.3% of benign liver tumours and are generally autopsy or intraoperative findings.5,6
We present a case of bile duct adenoma in which the pathology study observed a proliferation of ducts surrounded by presumably atypical cells and encompassed by a stroma with marked dysplasia, which confused the diagnosis.
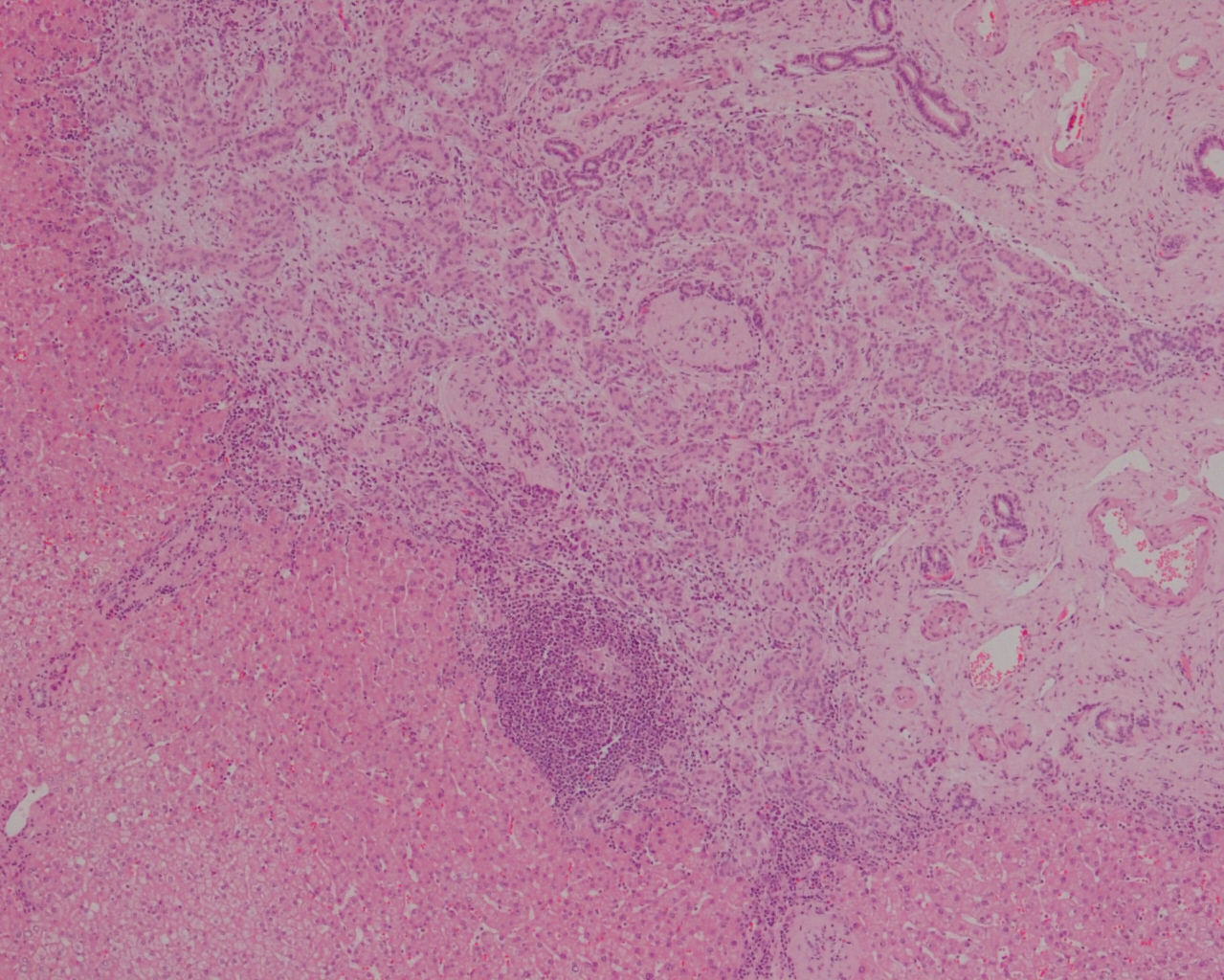
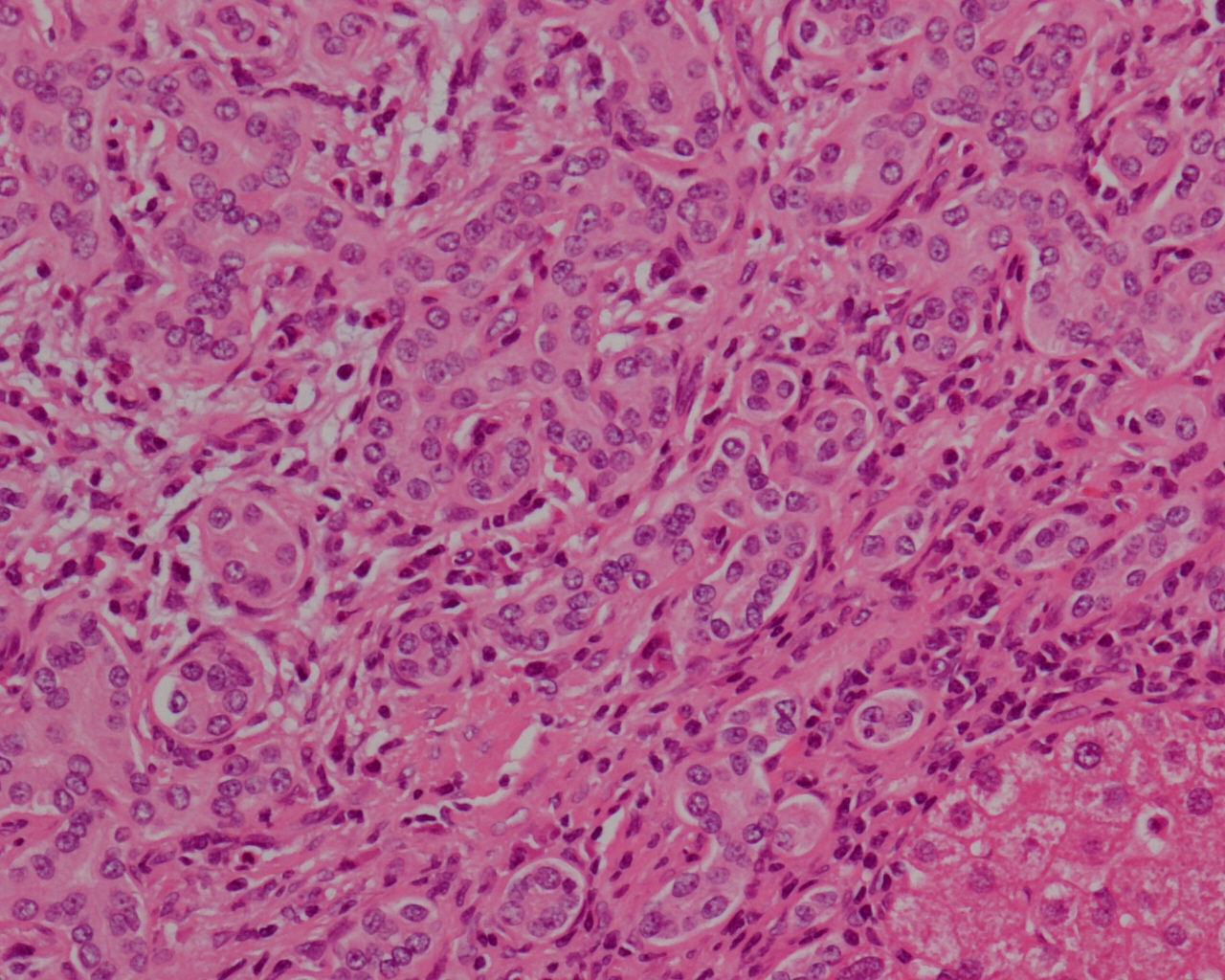
The patient is a 60-year-old woman with a history of arterial hypertension, pre-anaesthesia ASA II, BMI 28, who had undergone laparoscopic cholecystectomy due to multiple symptomatic gallstones (non-complicated) diagnosed by previous abdominal ultrasound. The imaging study also detected grade I hepatic steatosis and a solitary cyst measuring 3cm in segment II. Surgery involved conventional cholecystectomy and the biopsy of a white subcapsular nodule at the anterior edge of segment III, which measured less than 1cm in diameter. The postoperative period transpired without incident. The pathology study reported chronic cholecystitis and a moderately differentiated cholangiocarcinoma with infiltrated margins. Further studies included hepatic MRI, magnetic resonance cholangiopancreatography, and thoracoabdominal computed tomography, which only detected a simple cyst in liver segment II that was 3cm in diameter. With the incidental diagnosis of cholangiocarcinoma, the patient was re-operated on. Intraoperative findings included: (1) the remainder of a nodule on the anterior edge of segment III measuring 0.5cm; (2) on the lower edge of the liver, between segments II–III, other nodules with similar characteristics measuring 1cm; (3) in segment I, 4mm from the IVC, another 0.6cm nodule; (4) lymph node of the common hepatic artery that measured 2cm in diameter. With intraoperative ultrasound, the lesions were only observed with digital compression, and the previously detected simple cyst was also observed in the posterior region of segment II; the remainder of the examination was normal. Intraoperative biopsy study of the nodule between segments II–III reported this to be a carcinoma that was probably biliary in origin, while the lymphadenopathy was free of tumour infiltration. With the diagnosis of multicentric cholangiocarcinoma, we proceeded with hepatectomy of segments II–III–IV, segmentectomy of I and lymph node dissection of the hepatic pedicle. The patient was discharged without incident on the 7th day post-op. The study of the lymphadenectomy showed no evidence of tumour infiltration. The diagnosis of the liver nodules was uncertain, so samples were sent to 2 reference hospitals. The definitive pathology of the 3 nodules reported bile duct adenomas (peribiliary gland hamartoma) that were cytokeratin 7 positive, had a very low Ki-67 proliferation rate and were negative p53 (Figs. 1 and 2).
Adenomas of the bile ducts are rare focal lesions that are often multiple and have no accompanying symptoms. In general, they are not detectable with imaging studies, so they lead to diagnostic confusion with other primary or secondary tumours of the liver if they are not taken into consideration.2,6
There is no consensus about the origin and pathogenesis of these tumours. While some authors argue that they originate in small-calibre interlobular bile ducts,2 others attribute them to the intramural or extramural tubuloalveolar mucous glands (peribiliary glands).7
As for their formation, some classify them as true adenomas (benign neoplasms),8 others as hamartomas (developmental anomalies)7 and others still as a reactive process against a focal lesion of the ducts (inflammatory).2,5 They should be differentiated from von Meyenburg complexes,9 which are true hamartomas of the ducts, smaller in size (0.5cm), and part of the spectrum of cystic liver diseases; their presentation is multiple and they are characterized by dilated ducts filed with thick bile.
The immunohistochemistry profile studies detected the presence of acid mucin and antigens derived from the anterior intestine, such as D10, 1F6, MUC6, MUC5AC and TFF2, which would resemble a process of biliary healing originating in the peribiliary glands, similar to the metaplasia of the pyloric glands.5 In our case, the positivity for keratin 7 and epithelial membrane antigen indicated the bile ducts and portal spaces, respectively; likewise, the negativity for p53 and the limited Ki-67 activity ruled out intense proliferation.
There is consensus about the benign biological behaviour of bile duct adenomas, which only require observation (always with histologic confirmation). What is more important, due to the frequent confusion of this lesion with metastatic adenocarcinomas and cholangiocarcinomas (one-third of cases according to Allaire et al.), both surgeons and pathologists should be familiarized with its existence and correct diagnosis to indicate conservative treatment.1–4,10
Please cite this article as: Fernández Fernández JM, Muriel Cueto P, Sánchez Sánchez AM, Dulanto Vargas M, Bados Nieto P. Adenoma de conductos biliares (hamartoma de glándulas peribiliares): la importancia de su adecuado reconocimiento. Cir Esp. 2015;93:e95–e96.