There has been an increase in the implantation of subcutaneous reservoirs in recent years. The objective of this study is to compare puncture techniques against venous dissection.
MethodsRetrospective cohort study. It included patients who required a Port-a-Cath. Patients were divided into two groups: venous puncture (PV) and venous dissection (DV). Patients were over 18 years of age, requiring continued intravenous treatment, with no restriction of pathology. We excluded those who had been carrying a previous reservoir, and pediatric patients. The choice of the technique was based on the surgeon's preferences. We analyzed the clinical parameters of age, sex, ASA, BMI, reason for placement and laterality, and data related to the complications and withdrawal rate in each of the groups. The average follow-up was two years.
Results386 patients were included during 5 years: 228 DV group and 155 PV group. In three cases, the technique was not registered. There were no differences between the two groups in age, sex, ASA, BMI and reason for implantation (P > .05). DV presented a lower number of complications, and increased replacement and removal of catheter in PV was observed. Despite this, there were no statistically significant differences (P = .113).
ConclusionsBoth DV and PV are safe and effective techniques. In our experience, DV presented better intraoperative and long-term results. More studies are recommended to discern the technique to be used more safely.
Ha habido un aumento en la implantación de reservorios subcutáneos en los últimos años. El objetivo de este estudio es comparar las técnicas de punción frente a la disección venosa.
MétodosEstudio de cohortes retrospectivo. Incluyó a pacientes que requirieron un Port-A-Cath. Se dividió a los pacientes en dos grupos: punción venosa (PV) y disección venosa (DV). Los pacientes eran mayores de 18 años, requerían tratamiento intravenoso continuado, sin restricciones de patología. Se excluyeron quienes habían sido portadores de un reservorio previo, y pacientes pediátricos. La elección de la técnica se basó en preferencias del cirujano. Se analizaron los parámetros clínicos de edad, sexo, ASA, IMC, motivo de colocación y lateralidad, y los datos referidos a las complicaciones y la tasa de retirada en cada uno de los grupos. El seguimiento medio fue de dos años.
ResultadosFueron incluidos 386 pacientes durante 5 años: 228 grupo DV y 155 grupo PV. En 3 casos la técnica no quedó registrada. No hubo diferencias entre ambos grupos en edad, sexo, ASA, IMC y motivo de implantación p > 0,05. La DV presentó menor cifra de complicaciones y se observó un mayor recambio y retirada de catéter en PV. A pesar de ello no hubo diferencias estadísticamente significativas p = 0,113.
ConclusionesTanto la DV como la PV son técnicas seguras y eficaces. En nuestra experiencia la DV presentó mejores resultados intraoperatorios y a largo plazo. Se recomienda realizar más estudios para discernir la técnica a utilizar con mayor seguridad.
In recent years, an increase has been observed in the implementation of subcutaneous central venous catheters, largely due to the need to administer intravenous drugs continuously over long periods.1
The history of central venous catheters dates back to the early 20th century when Bleichroeder2 described the passage of a urethral catheter from the upper extremities to the armpit in a human being. Years later, Forssman3 managed to reach the cardiac cavities, corroborated with chest radiography.4 It was not until 1952, when Aubaniac5 achieved subclavian venous access through an infraclavicular puncture. In 1973, Broviac et al.6 conducted a study with 18 patients, with central venous access in 13 of them by puncture and 9 by subclavian dissection. To this end, they used an intravenous catheter, which was connected to a Dacron® cuff (DuPont de Nemours, Inc., Wilmington, Delaware, US), thereby isolating the intravascular access in what is considered the start of the venous devices as we know them today.
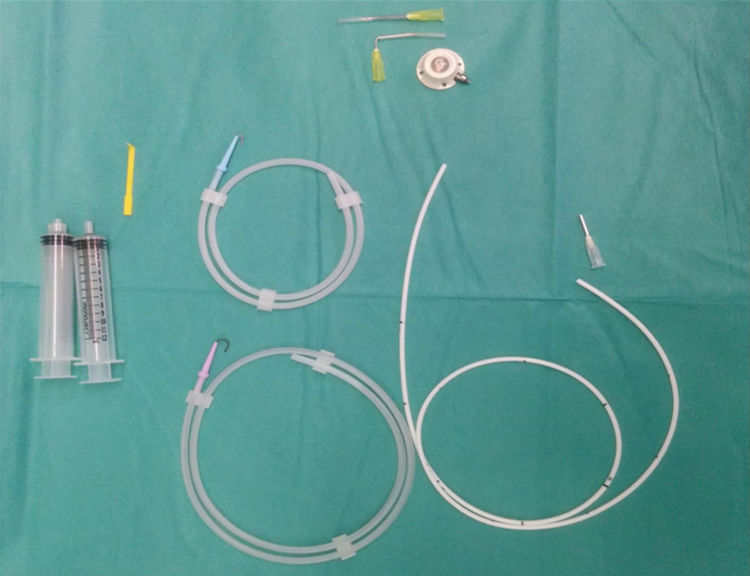
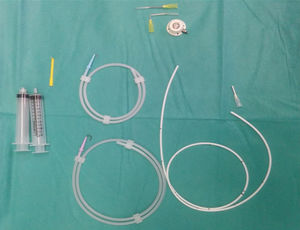
Currently, there is a wide variety of long-term venous access systems, called central venous catheters, that allow us to access the venous system and dispense with peripheral venous pathways.7 Currently, the most commonly used devices are fully implantable reservoirs, also called Port-A-Caths® PAC, which have been used in this present study Smiths Medical; Minneapolis, MN, United States. They are completely implanted under the skin and are especially useful in cases requiring prolonged intermittent access. PAC are made of surgical steel or a polyester material with a self-sealing silicone membrane, which can be accessed by percutaneous puncture with an angled needle, thereby preventing extravasation of the infused solution. PAC can usually withstand approximately 2000 punctures.7,8
The advantages of the placement of subcutaneous catheters are mainly that they are protected by their location under the skin, providing greater safety by reducing the probability of accidents, as opposed to peripheral pathways in which repeated venipunctures need to be performed, increasing the risk of infection.9 In this way, patients can live a normal life, leading to better acceptance of their disease.
Several studies about the use of venous catheters suggest that they are a safe and aesthetically acceptable alternative, with a low rate of complications in patients requiring prolonged venous access.10–12 In their comparative study, Tsai et al.13 suggested that the right access route is superior to the left, while there is no consensus on which of the techniques (Seldinger vs. venotomy) obtains lower complication rates.
The objective of this study is to compare the implantation techniques of a reservoir by venous puncture (VP) or vein dissection (VD) and to determine morbidity rates.
MethodsA retrospective comparative cohort study was conducted (without random selection) of patients who had PAC implanted at a second-level hospital. Two-venous access techniques were compared: direct VP and VD. The first, described by Seldinger14 in the 1950s, involved locating the vein, inserting a thin needle, subsequently inserting a flexible metal guide through it and checking for blood reflux, then allowing progression with the catheter, which is then connected to the port that is usually affixed on the pectoralis major.15 The second technique, called venotomy, involves performing open surgical dissection, usually on the cephalic vein, which causes less trauma injury to the vessel and reduces damage to neighboring structures.16 The selection of the technique in this study was based on the surgeon’s preferences.
The objective of this study was to compare both access techniques during the implantation of a PAC. Demographic data were analyzed, including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) scale, access laterality and reason for insertion. Other variables assessed included early complications during surgery, late complications and the need for withdrawal and a new PAC implantation.
The information in this study was obtained from medical records registered in the SAP software program (SAP AG, Walldorf, Germany). Inclusion criteria were: patients with indication for PAC placement for intravenous treatment who were over 18 years of age and had no pathology restrictions. Excluded from the study were patients with previous PAC and pediatric patients. All devices were implanted by the same 2 surgeons, each of them always performing the same technique.
Prior to each insertion, all patients underwent a preoperative anesthesiology study at our hospital, which systematically consisted of lab work, electrocardiogram and chest x-ray. The PAC used consisted of a titanium port with a self-sealing silicone membrane and a silicone catheter (Fig. 1). The devices were implanted in the operating room under aseptic conditions, local anesthesia and sedation. The access routes chosen were puncture (Seldinger technique) or by dissection. The port was affixed to the aponeurosis of the pectoral muscle. In all cases, the correct function and permeability of the catheter were verified, administering a solution with heparin at a concentration of 100 IU/mL to avoid thrombosis. Subsequently, radiological confirmation provided visualization of the location of the catheter tip. Patients were discharged after radiological follow-up. These patients were monitored for 2 years.
Statistical AnalysisFor the analysis of the data collected, the statistical system SPSS v.17.0 (IBM Corp; Armonk, New York, USA) was used. Pearson’s chi-squared test was used as well as Fisher’s exact test for qualitative variables. Likewise, the t-test and the Levene test were also used for equality of variances. A P value <.05 was considered statistically significant.
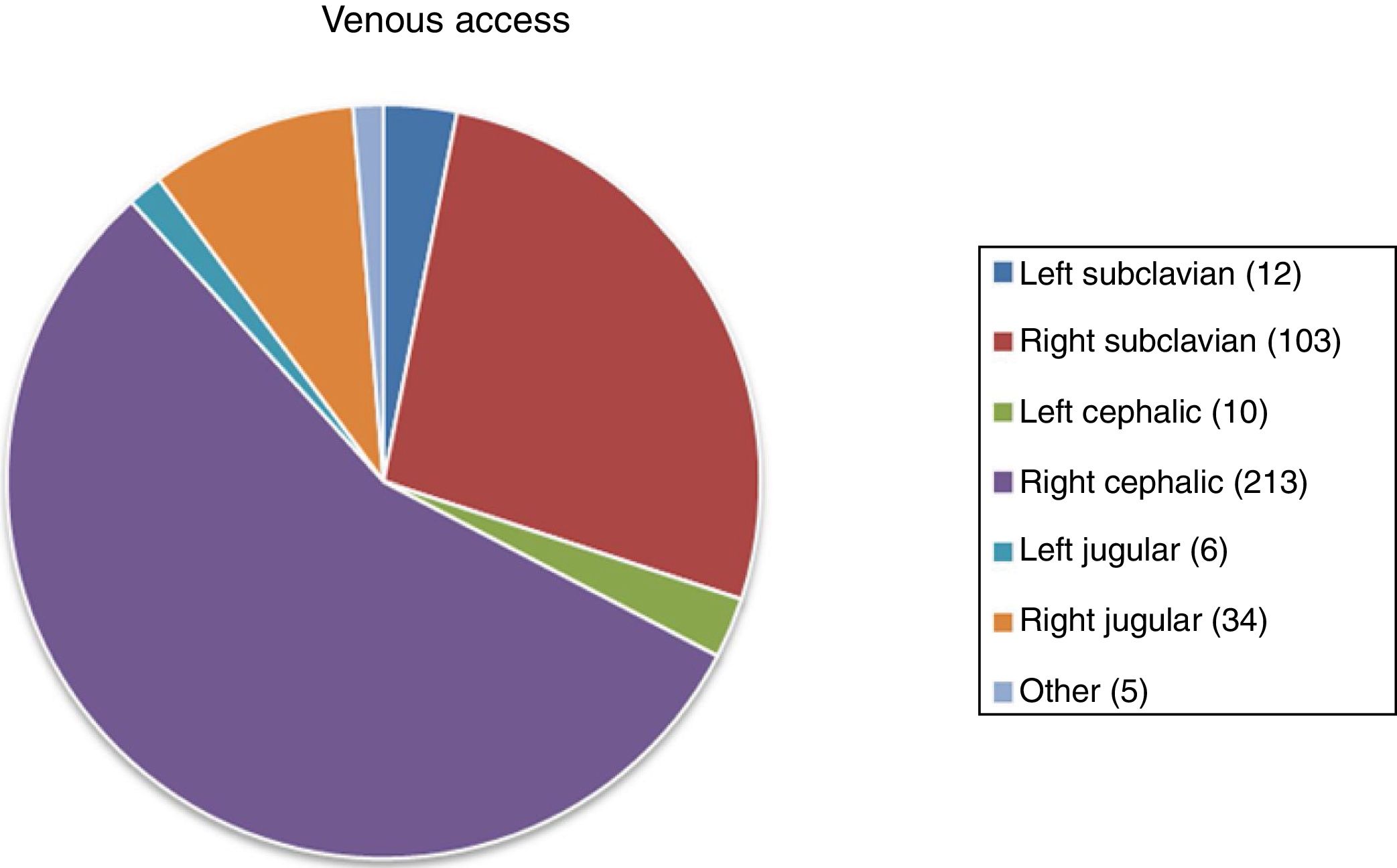
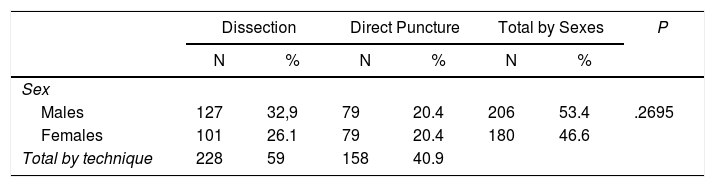
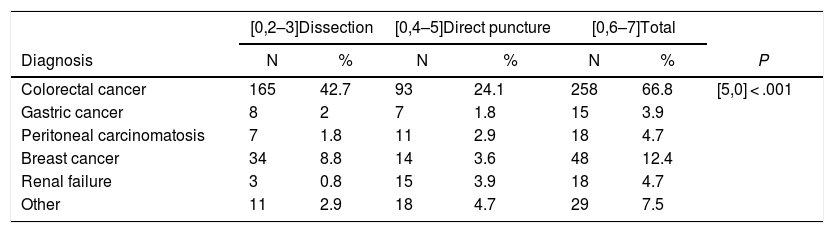
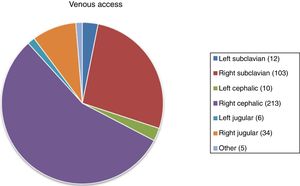
Results386 patients were recruited for PAC for a period of 5 years: 228 (59.5%) belonging to the VD group and 155 (40.5%) to the VP group. The distribution of the access route by sex is shown in Table 1. The age range was 28–92 years, with a mean of 64 and a median of 65 years. No statistically significant population differences were found. There were also no significant differences between the groups in age, sex, BMI and ASA (P > .05). The mean follow-up was 2 years. The most frequent indications for reservoir placement are shown in Table 2, while the distribution of the access types is shown in Fig. 2. The total number of left approaches was 28 (7.25%) and total number of right approaches was 350 (91%); in 5 (2%), the laterality was not defined, and in 3 no data are available about the technique used.
Access Pathway Chosen According to the Indication.
| [0,2–3]Dissection | [0,4–5]Direct puncture | [0,6–7]Total | |||||
|---|---|---|---|---|---|---|---|
| Diagnosis | N | % | N | % | N | % | P |
| Colorectal cancer | 165 | 42.7 | 93 | 24.1 | 258 | 66.8 | [5,0] < .001 |
| Gastric cancer | 8 | 2 | 7 | 1.8 | 15 | 3.9 | |
| Peritoneal carcinomatosis | 7 | 1.8 | 11 | 2.9 | 18 | 4.7 | |
| Breast cancer | 34 | 8.8 | 14 | 3.6 | 48 | 12.4 | |
| Renal failure | 3 | 0.8 | 15 | 3.9 | 18 | 4.7 | |
| Other | 11 | 2.9 | 18 | 4.7 | 29 | 7.5 | |
The vast majority of patients were treated in the major ambulatory surgery setting. In spite of this, the average hospital stay increased up to 1.9 days, with a standard deviation of 6.78 (range 0–40 days), but with a maintained median at 0 days, which is explained because some patients were already hospitalized previously and it was decided to place the device during hospitalization.
A total of 21 patients (5.5%), were re-operated: 12 (5.3%) from the VD group and 9 (5.8%) in the VP group (P = .85). No deaths were recorded that had been directly caused by PAC implantation. PAC removal was done in 20 cases during the period studied (5.2%), most of which were due to the completion of the chemotherapy cycles.
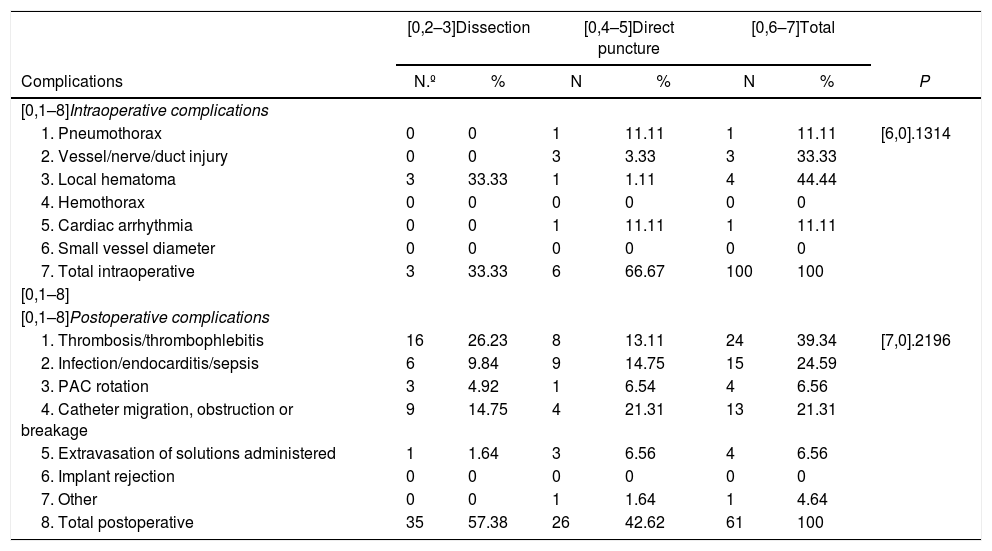
There were 9 (3%) intraoperative complications and 61 (15.8%) late complications throughout the study (Table 3). Regarding the overall complication rate according to the implantation technique used, the VD obtained better results: 15.4% of complications compared with 16.8% in VP (P = .113), with a risk estimation 1.09 times greater in VP.
Intraoperative and postoperative complications according to the access type.
| [0,2–3]Dissection | [0,4–5]Direct puncture | [0,6–7]Total | |||||
|---|---|---|---|---|---|---|---|
| Complications | N.º | % | N | % | N | % | P |
| [0,1–8]Intraoperative complications | |||||||
| 1. Pneumothorax | 0 | 0 | 1 | 11.11 | 1 | 11.11 | [6,0].1314 |
| 2. Vessel/nerve/duct injury | 0 | 0 | 3 | 3.33 | 3 | 33.33 | |
| 3. Local hematoma | 3 | 33.33 | 1 | 1.11 | 4 | 44.44 | |
| 4. Hemothorax | 0 | 0 | 0 | 0 | 0 | 0 | |
| 5. Cardiac arrhythmia | 0 | 0 | 1 | 11.11 | 1 | 11.11 | |
| 6. Small vessel diameter | 0 | 0 | 0 | 0 | 0 | 0 | |
| 7. Total intraoperative | 3 | 33.33 | 6 | 66.67 | 100 | 100 | |
| [0,1–8] | |||||||
| [0,1–8]Postoperative complications | |||||||
| 1. Thrombosis/thrombophlebitis | 16 | 26.23 | 8 | 13.11 | 24 | 39.34 | [7,0].2196 |
| 2. Infection/endocarditis/sepsis | 6 | 9.84 | 9 | 14.75 | 15 | 24.59 | |
| 3. PAC rotation | 3 | 4.92 | 1 | 6.54 | 4 | 6.56 | |
| 4. Catheter migration, obstruction or breakage | 9 | 14.75 | 4 | 21.31 | 13 | 21.31 | |
| 5. Extravasation of solutions administered | 1 | 1.64 | 3 | 6.56 | 4 | 6.56 | |
| 6. Implant rejection | 0 | 0 | 0 | 0 | 0 | 0 | |
| 7. Other | 0 | 0 | 1 | 1.64 | 1 | 4.64 | |
| 8. Total postoperative | 35 | 57.38 | 26 | 42.62 | 61 | 100 | |
When comparing the different subgroups, the right jugular presented a greater number of complications (41.5%) compared to the right subclavian (15.5%), while the route with the least complications was the right cephalic (15%). Based on our results, the best approach was the right cephalic vein with the dissection technique. Finally, the right-side access routes in general had fewer complications (33 in 350 patients; 9.4%) compared to the left-side approaches (9 in 28 patients; 21.4%). Overall, the VD presented a lower number of complications, both late and early, and there were more replacements and more removals with the technique by puncture.
DiscussionIn the present study, we have observed that the right cephalic access was mainly used, followed by the left subclavian, and implantation in cancer patients was most frequent.17 The indication was significantly higher in patients with colorectal cancer, with no observed differences in terms of sex. Overall, the technique that had fewer complications, both intraoperative and postoperative, was dissection. Alsfasser et al.,18 with a complication rate similar to the present study, agree that part of the complications of VP can be explained by the success rate during catheterization, which in VD is done under direct vision. This avoids repeated punctures, which are sometimes done during VP and are related with the surgeon’s experience.
The re-operation rate was higher with the Seldinger technique, with no observed statistically significant differences. Hospital stay, however, was longer with dissection, but the differences were due to the fact that part of the patients were already hospitalized when the PAC was implanted. The patients who were treated within the program showed no significant differences in terms of hospital stay.
The use of subcutaneous intravenous ports is on the rise because these devices are being indicated for more and more diseases. This is mostly due to the growing number of cancer patients undergoing chemotherapy, making this type of venous access essential for the regular administration of intravenous medication.19,20 In addition to the advantages for patients, some studies associate these devices with lower costs and fewer complications compared to peripheral venous pathways.21,22 Regarding the complication rate, Aspiazu et al.21 suggest that the complications could be related to the size and caliber of the port. Interventional radiology has been able to reduce the number of complications with the VP technique, so introducing this technique could change the comparative results in future studies.23
In recent years, the evolution of the technique and the surgical material has meant that the same procedure can be performed by different approaches safely and effectively.23 Both the dissection technique and the puncture technique are valid and offer good results in expert hands. Despite this, it is recommended that surgeons master both techniques in case one of the approaches is contraindicated or a definitive venous access was not achieved. Our experience leads us to believe that the open dissection technique has better intraoperative and long-term results. However, we also believe that new randomized, prospective studies with larger samples are needed to compare port types and sizes, as well as new variables like interventional radiology. Once these conclusions are corroborated, we will be able to offer the best techniques to patients with indications for central venous catheters.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Pérez Calvo J, Castellví Valls J, Crusellas O, Petrone P. Estudio comparativo entre vías de acceso de implantación de Port-A-Cath®. Cir Esp. 2020;98:79–84.