Supralevator fistula-in-ano are difficult to manage. If these fistulas have an additional supralevator internal-opening in rectum apart from the primary internal-opening at the dentate line, then the management becomes even more difficult. There is no literature/guidelines available on the management of supralevator rectal opening (SRO).
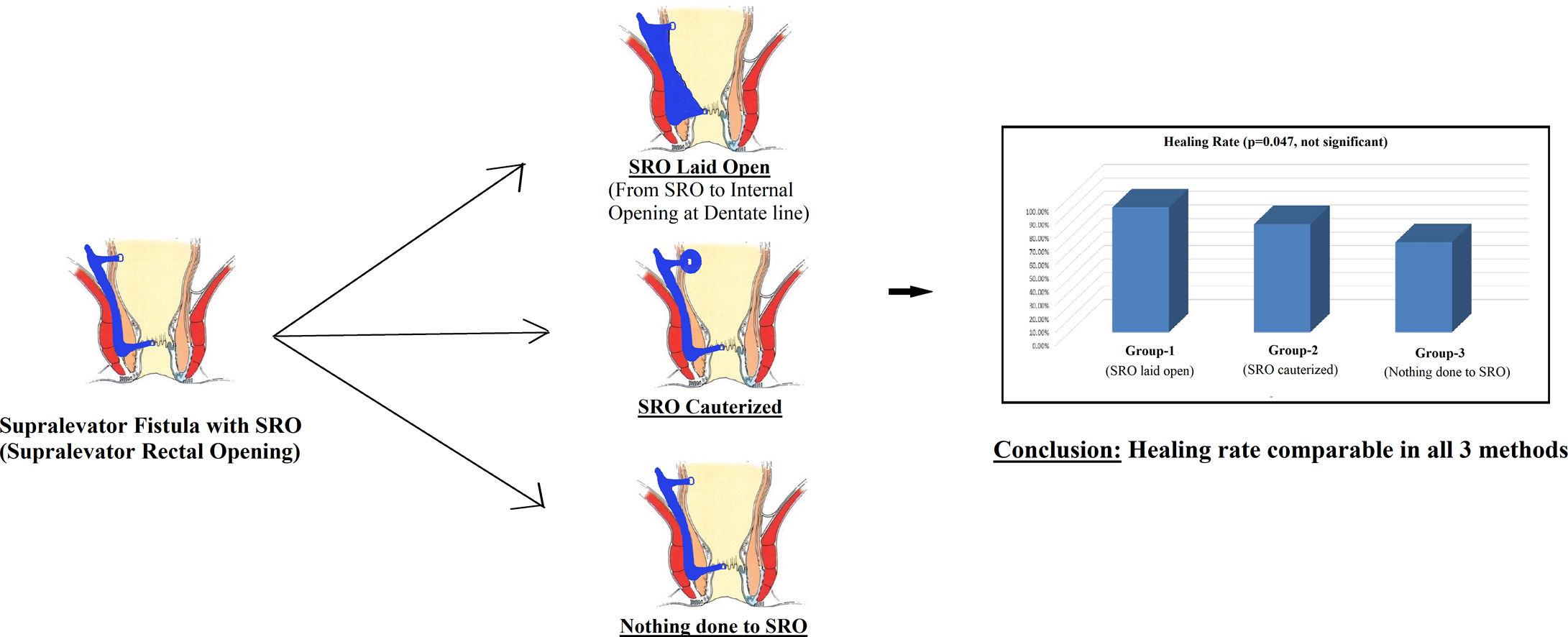
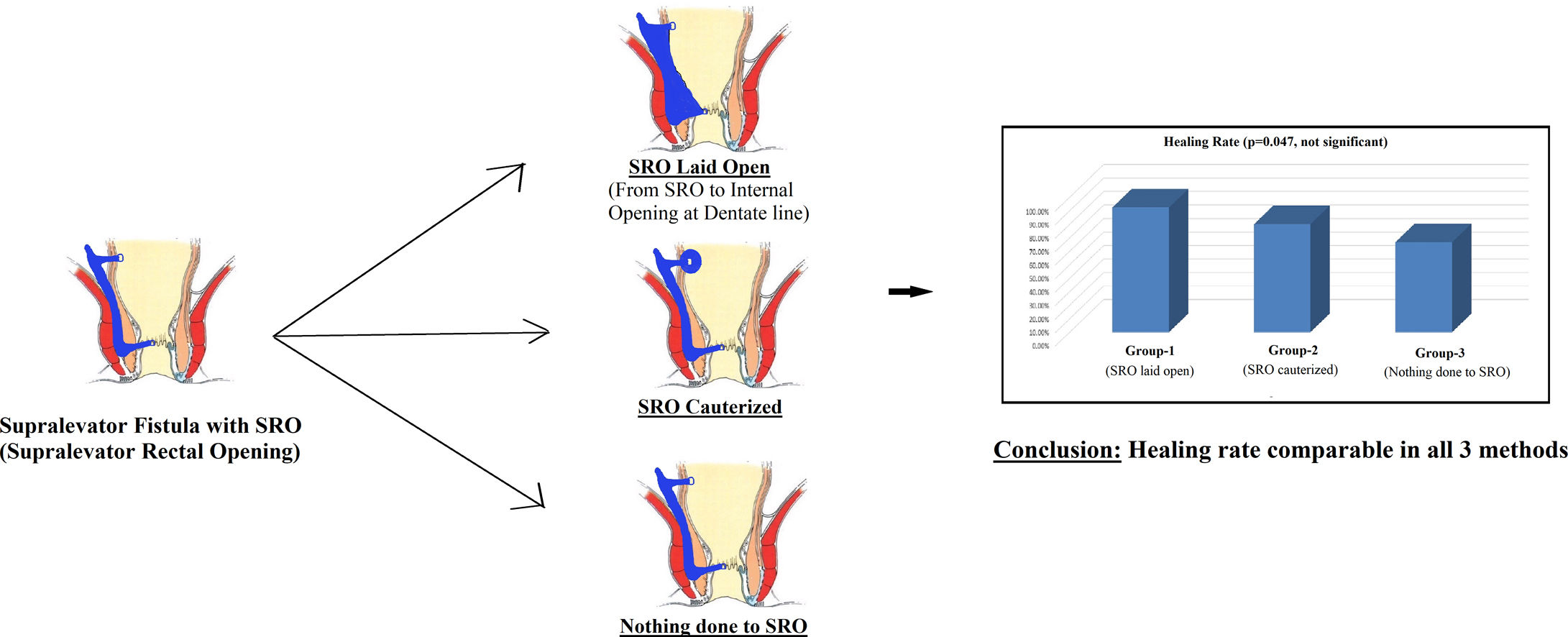
MethodsAll consecutive supralevator fistula-in-ano patients having a SRO were retrospectively analyzed. The operative management of SRO in these fistulas was reviewed. All the fistulas were managed by the same procedure, transanal opening of intersphincteric space (TROPIS). The latter was a modification of LIFT (ligation of intersphincteric tract) procedure in which the intersphincteric tract was opened-up in the rectum rather than ligated (as is done in LIFT). The SRO was managed in three ways, group-1:SRO was laid-open into the rectum in continuity with the primary opening at dentate line, group-2:the mucosa around SRO was cauterized, group-3:nothing could be done to SRO.
ResultsOut of 836 patients operated between 2015 and 2020, 138 patients (16.5%) had supralevator extension. Amongst these, 23/138 (16.6%) patients had a SRO. 2 patients were excluded (short follow-up) and 21 patients were included in the analysis. 12/13(92%) patients in group-1, 4/5 (80%) patients in group-2 and 2/3(67%) patients in group-3 got healed (p=0.47, Chi-square test). The overall healing rate was 18/21(86%).
ConclusionsThe supralevator rectal opening (SRO) heals well irrespective of the method utilized. Thus, proper management of the primary opening at the dentate line holds the key to fistula healing and SRO is perhaps not much responsible for persistence of the fistula. However, more studies are needed to corroborate these findings.
Las fístulas anales del supraelevador son difíciles de manejar. Si estas fístulas tienen una apertura interna supraelevador adicional en el recto además de la apertura interna primaria en la línea dentada, el manejo se vuelve aún más difícil. No hay literatura o pautas disponibles sobre el manejo del orificio rectal supaelevador (ORS).
MétodosSe analizó retrospectivamente a todos los pacientes consecutivos con fístula en el ano supraelevador que tenían un ORS. Se revisó el manejo operatorio del ORS en estas fístulas. Todas las fístulas fueron manejadas por el mismo procedimiento, apertura transanal del espacio interesfinteriano (TROPIS). El último fue una modificación del procedimiento ligadura del tracto interesfinteriano (LIFT) en el que el tracto interesfinteriano se abrió en el recto en lugar de ligarse (como se hace en LIFT). El ORS se manejó de 3 maneras: grupo 1: el ORS se abrió en el recto en continuidad con la apertura primaria en la línea dentada; grupo 2: se cauterizó la mucosa alrededor del ORS, y grupo 3: no se pudo hacer ORS.
ResultadosDe 836 pacientes operados entre 2015 y 2020, 138 pacientes (16,5%) tenían extensión del supraelevador. Entre estos, 23/138 (16,6%) pacientes tenían un SRO. Se excluyó a 2 pacientes (seguimiento corto) y se incluyó a 21 pacientes en el análisis; 12/13 (92%) pacientes en el grupo 1, 4/5 (80%) pacientes en el grupo 2 y 2/3 (67%) pacientes en el grupo 3 se curaron (p=0,47, prueba de la chi al cuadrado). La tasa de curación general fue 18/21 (86%).
ConclusionesEl ORS cicatriza bien, independientemente del método utilizado. Por lo tanto, el manejo adecuado de la abertura primaria en la línea dentada es la clave para la curación de la fístula y el ORS quizás no sea muy responsable de la persistencia de la fístula. Sin embargo, se necesitan más estudios para corroborar estos hallazgos.
Complex anal fistulas are not easy to treat and amongst these, the supralevator fistulas are considered the most difficult ones.2–4 Anal fistulas usually initiate at the dentate line and the supralevator extension generally occur at a later stage.2,5,6 Some of the tracts extending to the supralevator space open into the rectal lumen as well, thus forming an additional supralevator rectal opening (SRO).5 An additional SRO has been reported in up to 20% of supralevator fistulas.5 The management of these fistulas with a primary internal opening at the dentate line (PIOD) and a SRO can be quite challenging.5 There is no literature available on management of anal fistulas with a SRO.
MethodsAll consecutive patients of fistula-in-ano operated at a single Centre between August 2015 and August 2020 were retrospectively analyzed. Preoperative MRI was done in all the patients. The fistulas with supralevator extension were segregated from the cohort. In this sub-group of supralevator fistulas, the cryptoglandular fistulas which had a supralevator rectal opening (SRO) were included in the study. The patients of Crohn's disease were excluded from the study. The diagnosis of supralevator tract and SRO was made on MRI. (T2 weighted images on coronal and axial section). The approval was taken from the Ethics Committee of the hospital.
The patients were admitted on the day of surgery and were given three doses (before surgery, 12 and 24h after surgery) of antibiotics (Ciprofloxacin-500mg, Ornidazole-500mg). The patients having an acute abscess with systemic symptoms (fever, leucocytosis, etc.) were admitted a day before surgery and were administered antibiotics (Ciprofloxacin, Ornidazole and Amikacin) a day before and on the day of surgery and continued with Ciprofloxacin and Ornidazole for five days after surgery.1
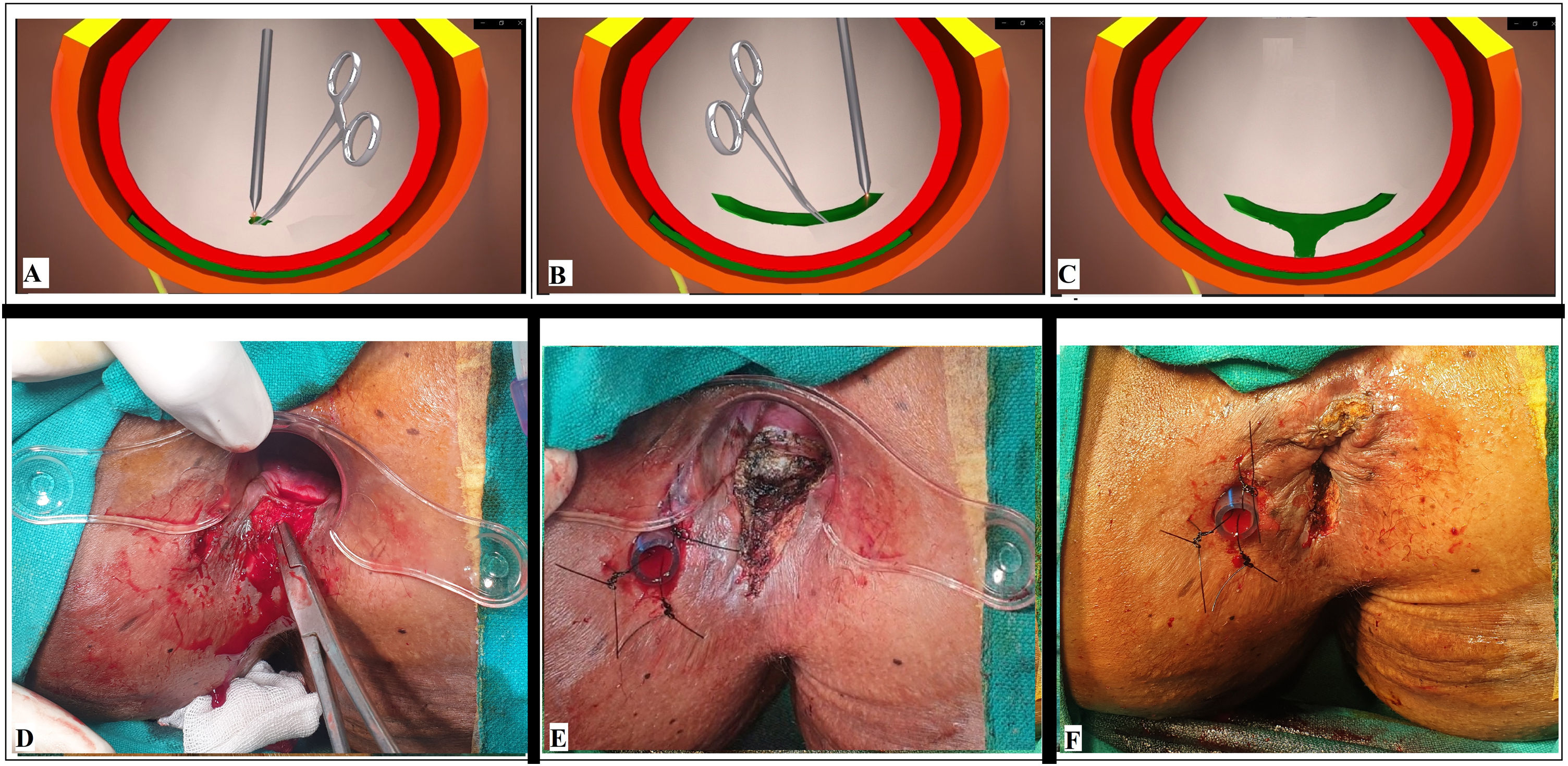
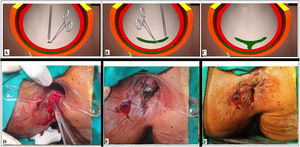
All the fistulas were managed by the transanal opening of intersphincteric space (TROPIS) procedure.1,7,8 The TROPIS procedure is a modification of the LIFT (ligation of intersphincteric tract) procedure. Unlike the LIFT procedure in which the intersphincteric tract is ligated, in TROPIS procedure, the internal opening and the intersphincteric portion of fistula tract is opened-up (deroofed) into the rectum through the transanal route1,7,8 (Fig. 1). The resulting wound (laid open intersphincteric space) in the anus was left open to heal by secondary intention1 (Fig. 1, panel: E). Thus, both the internal opening and the intersphincteric portion of the fistula tract healed well by secondary intention despite infection.1 On the other hand, the portion of fistula outside (lateral) to the external sphincter can be managed by any method convenient to the operating surgeon (excision of the tracts, curettage and insertion of a tube, laser excision, etc.). In the present study, the external tracts were curetted and cleaned. A tube (abdominal drain kit) was placed in these cleaned tracts from the external opening up to the lateral border of the external sphincter1 (Fig. 1, panel: E, F). This tube was sutured with the perianal skin1 (Fig. 1, panel: E, F). Once the wound inside the anus healed completely implying healing of the internal opening and the intersphincteric portion of the fistula tract, then the tube in the external tract was removed.1 Thus, the tracts on both sides of the external sphincter were managed without cutting or damaging the external sphincter in any way (the tracts inside the external sphincter was managed by TROPIS procedure and the tracts external to the external sphincter were managed by curettage and insertion of the tube). The opened up intersphincteric portion of fistula tract was not closed by sutures but was encouraged to heal by secondary intention.1 The latter was achieved by performing a gentle per-rectal examination in the post-operative period.1
Intraoperative wound after TROPIS (transanal opening of intersphincteric space). Schematic diagram: Panel-A: Intersphincteric tract (green colour) and an artery forceps inside the internal opening about to be laid open with electrocautery. Panel-B: Intersphincteric tract laid open with electrocautery. Panel-C: Intersphincteric space distal (inferior) to the internal opening laid open by a vertical incision. Intraoperative photograph: Panel-D: A curved artery-forceps inside the intersphincteric tract before laying it open. Panel-E: TROPIS wound in the anal canal. Panel-F: The tube inserted in the high abscess cavity and sutured to the skin with monofilament non-absorbable suture (2–0 nylon).
Group 1 – Lay-open: The SRO was laid-open into the rectum in continuity with the primary opening at dentate line (extension of the TROPIS wound up to the SRO).
Group 2 – Cauterization of surrounding mucosa: In cases, where SRO was high up and it was technically not possible to lay-open the intersphincteric tract up to the high opening, the mucosa around the SRO was cauterized with electrocautery.9 The intention was to create a raw wound around the internal opening so that the wound healed by secondary intention. This has shown to result in closure of the internal opening.9 These were the fistulas in which it was not possible to lay open the SRO (as was done in group 1).
Group 3 – Nothing was done: In cases, where SRO was so high up in the rectum that it was not possible to even cauterize the mucosa around the SRO, then nothing was done to SRO. Only the primary fistula and the opening at the dentate line was managed (TROPIS procedure).
Follow-upThe patients were discharged on the next day of surgery. They attended the clinic daily for a gentle per-rectal examination. This daily examination was done for approximately 4 weeks in the study, though in our opinion, even once a week per-rectal examination should also suffice. and then the patients were followed-up with visit to the clinic on a monthly basis.
The continence was evaluated by Vaizey's continence scoring10 preoperatively as well as postoperatively (on long-term follow-up). Vaizey's scores were used as they are more comprehensive than other scoring systems.10 This scoring assessed six parameters – incontinence to gas, liquid or solid, any need to take constipation medicines, any alteration in lifestyle, inability to hold defecation for 15min and need to wear a pad. A score of 24 would mean that the patient was totally incontinent while a score of zero would imply perfect continence.10
The healing was determined both clinically and radiologically (postoperative MRI) in all the cases. The fistula was defined as clinically healed when there was complete healing of all fistula tracts including the supralevator tracts as assessed by the operating surgeon on clinical examination (complete healing of intra-anal wound and closure of the external opening) and total cessation of pus discharge from all fistula tracts. The cut-off time period to define ‘non-healing’ was taken as six months. The fistulas of patients with persistent pus discharge after six months of surgery were labelled as ‘not healed’ and before six months were labelled as ‘short follow-up’. Once the clinical healing was complete, a postoperative MRI was done to corroborate the clinical healing in all the cases. Only when the fistula was healed clinically and radiologically, it was considered as fully healed.
After the fistula had completely healed, the subsequent long-term follow-up was done by telephonically questioning the patients and the latest status was updated. For the purpose of the study (long-term follow-up), all the patients were individually telephoned, and their latest fistula healing and continence status was updated. The patients who could not be contacted and whose long-term status could not be ascertained were listed as lost to follow-up.
Statistical analysisThe categorical variables were compared by performing Fisher's exact test or chi-squared analysis. When the data was normally distributed, the continuous variables were analyzed by t-test when there were two samples or ANOVA test when there were more than two samples. If the data was not distributed normally, Wilcoxon signed rank test was applied for paired samples and Mann–Whitney U test was performed for unpaired samples. The significant cut off point was set at p<0.05.
Results836 anal fistula patients were operated between 2015 and August 2020. The patients were followed-up for 29 months (median) (range: 2–62 months). Out of these, 138 patients (16.5%) had supralevator extension. Amongst these patients with supralevator extension, 23/138 (16.6%) patients had an additional SRO (supralevator rectal opening) along with a primary opening at the dentate line (PIOD). The PIOD was in midline posteriorly in all the cases. The external opening was present in 16 patients and there was no external opening in 7 patients as the fistula was high intersphincteric in these patients. In 12/16 patients, there was a single external opening and in 4/16 patients, there were two external openings. The location of external opening was posterior in 7/16, anterior in 4/16 and lateral in 5/16 patients. In all these 16 patients, the external tracts in the ischiorectal fossa were thoroughly curetted and a tube was put in. The tube was sutured to the perianal skin with a suture (Fig. 1, panel: E and F). Once the TROPIS wound inside the anal canal was healed and radiological healing confirmed with post-operative MRI, the tube in the external tracts was taken out.
As per Parks classification,11 there were 7 patients of grade-1 (high intersphincteric fistula with supralevator extension), 15 patients of grade-2 (transsphincteric fistula with supralevator extension), 1 patients of grade-3 (suprasphincteric fistula with supralevator extension) and no patient of grade-4 (extrasphincteric fistula).
There were 14 patients in group-1, six patients in group-2 and three patients in group-3. Two patients (one patient in group 1 and group 2 each) had a short follow-up and were excluded from the analysis. Thus, 21 patients were finally included in the analysis.
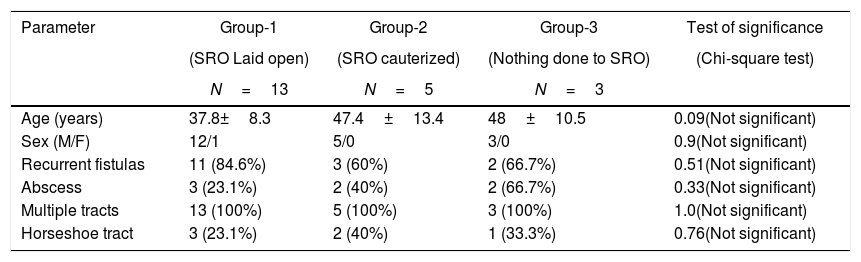
All the three groups were similar in age, sex, recurrent fistulas, multiple tracts, associated abscess, and horseshoe tracts (Table 1). In group-1, 9/13 (69.2%) fistulas were healed and 4/13 (30.8%) fistulas did not heal. 3/4 of these unhealed fistulas were operated again by the same procedure and all three got healed. None of fistulas in group-2 and group-3 were reoperated. Thus, the overall fistula healing was 12/13 (92%) patients in group-1, 4/5 (80%) patients in group-2 and 2/3 (67%) patients in group-3 (Table 2) (Fig. 2). The healing rate was comparable in all the groups (p=0.47, Chi-square test) (Table 2). The overall healing rate was 18/21(86%). The change in continence scores (Vaizey's scores) after the surgery was also similar in the three groups (p=0.88, Wilcoxon signed rank test) (Table 2).
Patient parameters and fistula characteristics in the three groups with a supralevator rectal opening (SRO).
| Parameter | Group-1 | Group-2 | Group-3 | Test of significance |
|---|---|---|---|---|
| (SRO Laid open) | (SRO cauterized) | (Nothing done to SRO) | (Chi-square test) | |
| N=13 | N=5 | N=3 | ||
| Age (years) | 37.8±8.3 | 47.4±13.4 | 48±10.5 | 0.09(Not significant) |
| Sex (M/F) | 12/1 | 5/0 | 3/0 | 0.9(Not significant) |
| Recurrent fistulas | 11 (84.6%) | 3 (60%) | 2 (66.7%) | 0.51(Not significant) |
| Abscess | 3 (23.1%) | 2 (40%) | 2 (66.7%) | 0.33(Not significant) |
| Multiple tracts | 13 (100%) | 5 (100%) | 3 (100%) | 1.0(Not significant) |
| Horseshoe tract | 3 (23.1%) | 2 (40%) | 1 (33.3%) | 0.76(Not significant) |
Fistula healing and incontinence scores in the three groups with a supralevator rectal opening (SRO).
| Parameter | Group-1 | Group-2 | Group-3 | Test of significance |
|---|---|---|---|---|
| (SRO Laid open) | (SRO cauterized) | (Nothing done to SRO) | ||
| N=13 | N=5 | N=3 | ||
| Fistula healed | 12 (92.3%) | 4 (80%) | 2 (66.7%) | 0.47(Not significant, Chi-square test) |
| Vaizey's incontinence scores (mean) | 0.88(Not significant, Wilcoxon signed rank test) | |||
| Pre-operative | 0.25±0.6 | 0.2±0.4 | 0 | |
| Post-operative | 0.33±0.6 | 0.2±0.4 | 0 | |
| Change in scores | 0.07±0.2 | 0 | 0 |
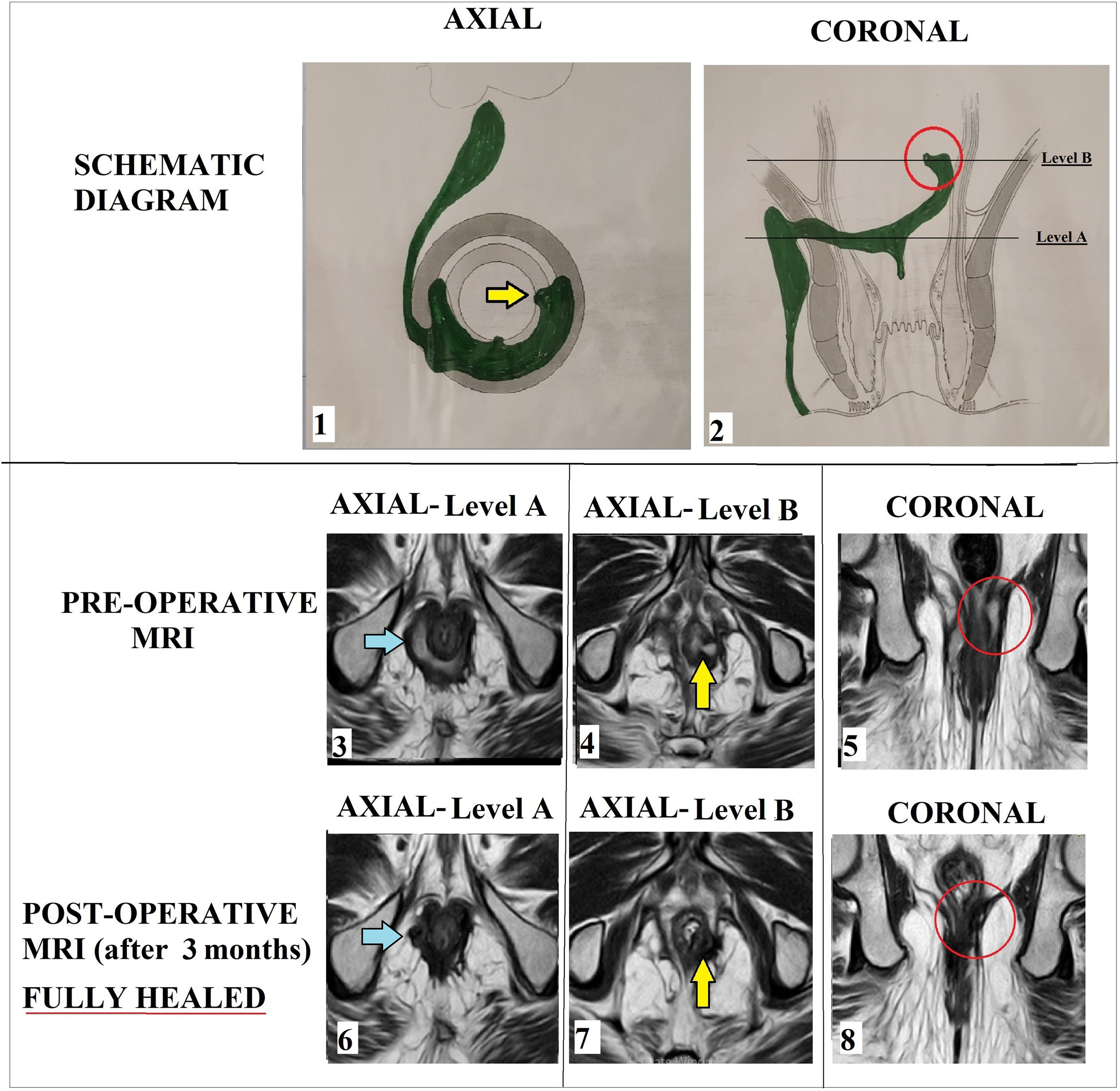
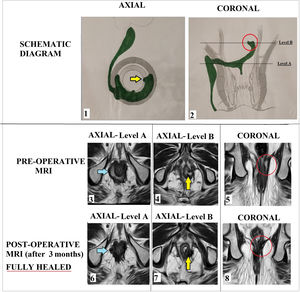
A 61-year old male patient with horseshoe fistula with additional supralevator rectal opening (SRO) at 3 o’clock position managed by cauterization of mucosa around the SRO (group-2). Panel-1: Schematic diagram-Axial section Panel-2: Schematic diagram-Coronal section. Level-A: level of intersphincteric horseshoe tract, Level-B- level of opening of SRO. Pre-operative MRI-T2 weighted images: Panel-3: Axial images at level-A showing intersphincteric horseshoe tract (blue arrow). Panel-4: Axial images at level-B showing SRO (yellow arrow). Panel-5: Coronal images showing SRO (red circle). Post-operative healed MRI-T2 weighted images (3 months after surgery). Panel-6: Axial images at level-A showing healed intersphincteric horseshoe tract (blue arrow). Panel-7: Axial images at level-B showing healed SRO (yellow arrow). Panel-8: Coronal images showing healed SRO (red circle).
Supralevator cryptoglandular anal fistulas are diagnostically as well as therapeutically challenging.12,13 The subset of supralevator fistulas with high additional supralevator rectal opening (SRO) looks even more trickier.2,6 However, the study highlighted that the SRO can be managed successfully in different ways and also demonstrated that perhaps, the proper management of the primary internal opening at the dentate line (PIOD), holds the key to the successful management of the SRO and the complete fistula. This is the first study in which different methods of managing SRO have been compared.
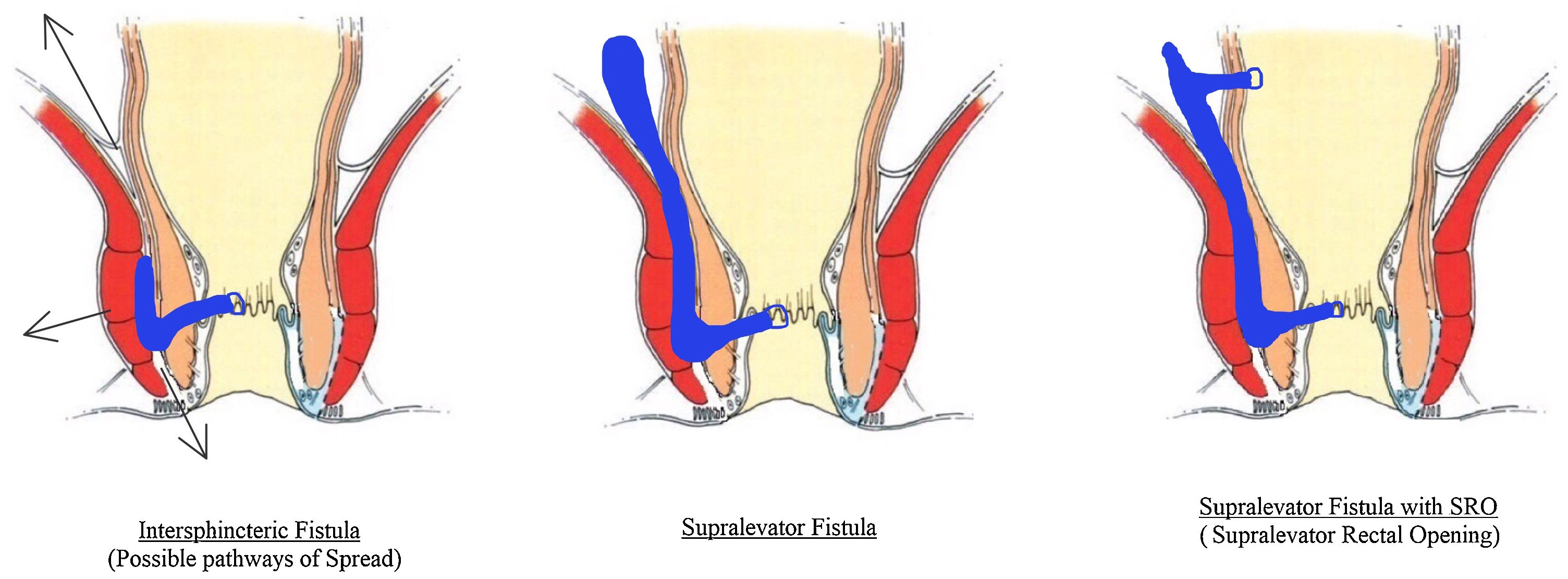
The importance of management of the PIOD is not difficult to understand. First, PIOD is the place where the opening of the ‘infected’ crypt gland lies, and the process of fistula formation starts.14 Therefore, PIOD is present in almost every cryptoglandular fistula. Once the fistula forms with the internal opening at the dentate line, then it can spread in any direction- towards the perianal skin, through the external sphincter into the ischiorectal fossa or through the intersphincteric space (Fig. 3).5
At times, enough pressure is generated in some fistulas that the pus/sepsis reaches up to high intersphincteric plane and in some of these cases, the tract even reaches the supralevator space5 (Fig. 3). Therefore, the supralevator extension is not common and only occur when the infection is quite virulent or the pus is not able to drain outside in the skin or ischiorectal fossa and spreads superiorly into the supralevator space. In the present study, the supralevator extension occurred in 16% of cases. However, this percentage could be slightly higher than the actual incidence because the study centre is a referral institute and gets more complicated cases due to which the supralevator cases could be proportionately higher.
Once the fistula/pus reaches the supralevator space, then it would perhaps require much higher amount of pressure for the pus to ‘burst or make way’ into the rectum5 (Fig. 3). Moreover, the intersphincteric space in infralevator region is tightly bound by the sphincter muscles (internal and external anal sphincter) and a little pus would generate quite high pressure whereas the supralevator space is a loose space and generating sufficient pressure by the pus would require much higher amount of pus. Therefore, the additional supralevator rectal opening occurred in much smaller proportion of supralevator fistulas (only 16% of supralevator fistulas had SRO). Apart from the possibility of pus spontaneously ‘bursting’ under high pressure into the supralevator space to form an additional SRO, there could be other reasons as well. The additional SRO could also form iatrogenically while draining a supralevator abscess during the previous surgery. This is relevant as 18/23 (78.2%) patients in the present study had undergone previous operations. The other possible reason could be inflammatory bowel disease (especially Crohn's disease). This reason looks less possible in the present study as none of the patients in the study was suffering from Crohn's disease.
The different methods of managing SRO (including the one in which nothing could be done to SRO as it was so high up in the rectum) yielded comparable success rates (92% in group-1, 80% in group-2 and 67% in group-3, p=0.88, not significant)) (Table 1). These findings especially the healing of the fistulas in group-3 in which nothing could be done to SRO looks surprising. Even though the healing occurred in only two patients in this group, but it still gives some insight into the pathophysiology of the complex fistulas. Also, in group 2 in which only the mucosa was cauterized, the fistulas healed in 80% of the patients.
The above findings indicate that perhaps the SRO is not responsible for the persistence of the fistula. The SRO forms as a result of excess pressure of pus in the high intersphincteric tract and it helps to release the pressure. So, it is possible that bacteria enter the fistula only through the primary internal opening at dentate line (PIOD), form pus in the fistula tract and pus (and bacteria) re-enters the rectum through the SRO. The bacteria, it seems, do not enter through the SRO into the fistula tract. This could be possible because, unlike anus, the rectum is a wider organ meant for storage of faeces. Therefore, the intraluminal pressure in rectum is not high enough to push bacteria into the fistula tract.5 Moreover, unlike the primary internal opening at dentate line (PIOD) which is fixed due to fixity of anus to the sphincter complex, the SRO in mid-rectum is relative less fixed which could make bacterial ingress more difficult into the SRO. Therefore, proper management of PIOD perhaps assumes greater significance than the management of SRO. Though, this hypothesis provides some explanation to the results of the study, but it needs to be corroborated by further research and long-term studies.
It is of paramount importance that with the help of MRI, the exact location of the supralevator abscess/tract is identified as whether it is in the intersphincteric plane or in the extrasphincteric plane. This has important implications in the management as the drainage of the supralevator abscess needs to be through the proper route.3,15,16 The supralevator abscess of intersphincteric origin should be drained through the endoanal route and not through the ischiorectal fossa to avoid forming a suprasphincteric fistula.3,15,16 On the other hand, an abscess due to high extension of a trans-sphincteric fistula should be drained through the ischiorectal fossa as draining it through the endoanal route would risk forming a complex extrasphincteric fistula.3,15,16 In the present study, preoperative MRI of every patient was analyzed in detail to ascertain the location of the supralevator extension. The supralevator tracts were in the intersphincteric space in all the patients in the present cohort. Therefore, management through the transanal (endoanal) route [TROPIS procedure] was done in all the patients.
It is standard accepted principle that the anorectal abscess should be first drained and the definitive surgery be carried out at a later date as the definitive surgery during the initial presentation increases the risk of incontinence.2,17–20 Similarly, supralevator abscess of intersphincteric origin can be drained through the endoanal route and mushroom/pezzer-type catheter be placed in the abscess cavity.2 The pezzer-type catheter drainage would reduce the length of the fistula and the cavity and the definitive procedure may be carried out later.2 At times, even fistulotomy may become possible in this method. However, we opted for definitive surgery for the patients with supralevator abscess during the initial presentation rather than going for staged procedures. The reason was that we had sufficient experience of performing definitive surgery on initial presentation. In a recently published study of TROPIS procedure in 325 high complex fistulas with a long-term follow-up (median-36 months), all the fistulas with associated abscesses were managed by definitive surgery during the initial presentation.1 There were 115 patients with abscess and 191 patients without abscess.1 The overall healing rate in the abscess and non-abscess groups was comparable [87% (100/115) and 88% (168/191) respectively, p=0.85].1 The difference between preoperative and postoperative continence scores between the abscess and non-abscess groups was also comparable.1 Even in the present study, there was no deterioration in continence after the surgery in any of the patients. Nonetheless, though the external sphincter is totally spared and only the internal sphincter is divided in TROPIS procedure, still a word of caution is needed. The possibility of deterioration in continence on long term follow-up when the ‘inflamed’ internal sphincter in the acute abscess is divided cannot be ruled out. Further, long-term studies would be needed to corroborate this.
The study has some limitations. It is a retrospective study. The number of patients in each group especially groups 2 and 3 were small. But considering the rarity of supralevator fistulas, getting a series of large number of supralevator anal fistulas with SRO would take very long period or multicentric collaboration.
To conclude, this is the first study to describe different methods to manage supralevator anal fistulas with an additional SRO (supralevator rectal opening). The fistula healing was good and comparable in all the three methods used (laying open the fistula tract from internal opening at dentate line up to the SRO, cauterization of mucosa around the SRO or doing nothing to the SRO). However, the sample size is small due to which it is difficult to draw any concrete conclusions. Further, long term studies are needed to corroborate the findings of this study.
Conflict of interestAll authors declare that they have no conflict of interest.