The Spanish Association of Coloproctology (AECP) and the Coloproctology Section of the Spanish Association of Surgeons (AEC), propose this consensus document about complicated diverticular disease that could be used for decision-making. Outpatient management, Hartmann's procedure, laparoscopic peritoneal lavage, and the role of a laparoscopic approach in colonic resection are exposed.
Desde la Asociación Española de Coloproctología (AECP) y la Sección de Coloproctología de la Asociación Española de Cirujanos (AEC), se propone un documento de consenso sobre la enfermedad diverticular complicada que pueda ser de utilidad en la toma de decisiones. En él se expone, principalmente, la actualidad en el tratamiento ambulatorio, la intervención de Hartmann, el lavado laparoscópico peritoneal, así como el papel del abordaje laparoscópico en la resección colónica.
Complicated diverticular disease of the colon is one of the 5 gastrointestinal conditions with the greatest impact on the national healthcare system. The presence of perforations has increased from 2.4% per 100,000 inhabitants in 1986 to 3.8 in 2000.1 This growing trend is a challenge for all surgeons who perform emergency surgery.
This increase has been accompanied by certain changes in treatment, such as outpatient management, resolution avoiding the use of a stoma, or the relatively new proposal that entails peritoneal lavage in purulent peritonitis parallel to the development of laparoscopy as a means of surgical approach, without forgetting that the Hartmann procedure (HP) continues to be one of the most widely used therapeutic options.
There is currently extensive experience and sufficient scientific evidence for surgeons to be able to follow well-defined patterns. In spite of this, we believe that it is useful for the Spanish Association of Coloproctology (Asociación Española de Coloproctología, AECP) and the Coloproctology Division of the Spanish Society of Surgeons to propose basic and specific guidelines based on the most recent scientific evidence in order to help clinicians make decisions in their clinical practice. The following 4 aspects of diverticular disease have been chosen in an attempt to establish solid and basic agreements: outpatient treatment, laparoscopic lavage and drainage, HP and the role of the laparoscopic approach in colonic resection for the current management of diverticular disease. However, we are aware that these factors are being constantly reviewed with the passage of time.
The methodology used in the creation of the consensus document was the following:
- •
A workgroup was organized, including 4 surgeons specialized in coloproctology from different national hospitals within the Spanish National Healthcare System (TBS, MFM, HMO, LPD), 2 experts in coloproctology (SB, JMRV), and a work coordinator (RRC).
- •
The consensus document was divided into 4 areas of interest in complicated diverticular disease: outpatient treatment, HP, laparoscopic lavage and drainage, and the role of the laparoscopic approach in colon resection for diverticular disease (elective and urgent surgery).
- •
Bibliographic searches were conducted in the PUBMED, MEDLINE and Cochrane Library search engines, using keywords related with each of the sections and including the most relevant articles from the last 10 years. Furthermore, additional interesting publications were located from the references listed by the articles identified in the initial search.
- •
The 20th National Conference of the Spanish Association of Coloproctology was held in Elche on May 19, 2016, which included a round table: Consensus Document of the AECP: Diverticular disease: presentation of evidence and questions answered by experts. Each of the 4 surgeons presented the updated bibliographic review of each of the lines proposed and closed the round table with conclusions based on scientific evidence and the opinion of each of the experts.
- •
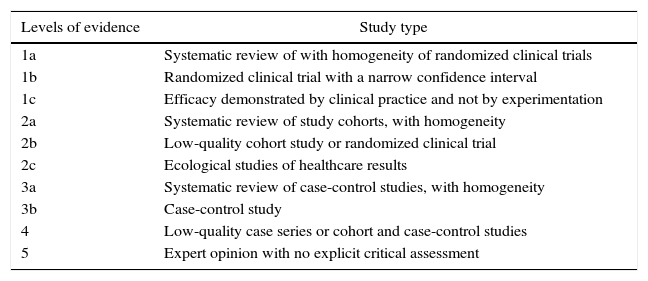
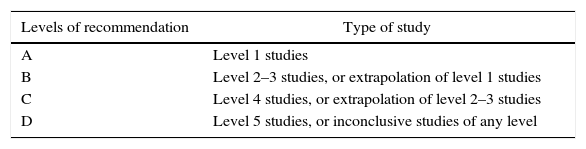
After the conference, the first document was written, which took into account this information, all the evidence obtained in the bibliographic search and the opinions of the experts. Each surgeon, supervised by the work coordinator, wrote the part corresponding with his/her area of interest. All the evidence and recommendations have been classified in accordance with the Centre for Evidence-Based Medicine, Oxford (CEBM)2 (Tables 1 and 2).
Table 1.Levels of Evidence (CEBM).
Levels of evidence Study type 1a Systematic review of with homogeneity of randomized clinical trials 1b Randomized clinical trial with a narrow confidence interval 1c Efficacy demonstrated by clinical practice and not by experimentation 2a Systematic review of study cohorts, with homogeneity 2b Low-quality cohort study or randomized clinical trial 2c Ecological studies of healthcare results 3a Systematic review of case-control studies, with homogeneity 3b Case-control study 4 Low-quality case series or cohort and case-control studies 5 Expert opinion with no explicit critical assessment - •
After the first document was completed, it was assessed by the scientific committee of the AECP, as well as by experts of the work group. After making appropriate modifications and incorporating their suggestions, the definitive document was completed.
The most frequent complication of diverticular disease is acute diverticulitis, which, in most cases, is uncomplicated or mild acute diverticulitis (75% of the diagnoses of symptomatic diverticular disease).3 Uncomplicated acute diverticulitis is classically defined as inflammation limited to the colonic wall or pericolic fat, in the absence of perforation, abscess, fistula or bleeding (Hinchey I). This definition would be modified in later classifications to also include patients with pericolic abscesses smaller than 5cm (Hinchey Ib).4
Medical treatment for uncomplicated acute diverticulitis has changed in recent years and, currently, outpatient management is considered optimal for selected patients both by most international clinical guidelines1,5–7 and in international consensus documents based on the opinion of experts,8 since it has been shown to be equally safe and effective, but less expensive.
According to international guidelines, in these cases the diagnosis of uncomplicated acute diverticulitis should be radiological, in addition to clinical and analytical. Although computed tomography is traditionally considered the gold standard in the diagnosis of an acute episode of diverticulitis, ultrasound can also be diagnostic8,9 and useful in monitoring treatment.
In addition, according to clinical recommendations, patients who are candidates for outpatient treatment should meet selection criteria: absence of fever or signs of sepsis, no significant comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, renal or cardiac insufficiency, immunosuppression), good oral tolerance, no cognitive or psychiatric alterations and adequate social support.
These recommendations are based on the results obtained in different studies on the outpatient treatment of uncomplicated acute diverticulitis,9–11 none of which was randomized. Similarly, it is concluded that outpatient treatment is safe for most patients with mild diverticulitis in recent systematic reviews by Jackson et al.12 or Tursi.13 Of all the included studies, we only found one multicenter randomized trial (DIVER trial)14 analyzing 132 patients with mild diverticulitis in 2 groups: outpatient treatment vs hospitalization. In both groups, patients received antibiotic treatment for 10 days. The primary endpoint of this study was failure of treatment and the secondary objective was to assess quality of life and costs. Once again, the conclusion obtained was that the outpatient treatment of selected patients with uncomplicated diverticulitis is safe and involves fewer costs.
Although in the different studies the concept of uncomplicated or mild acute diverticulitis is heterogeneous, patients with no intraabdominal abscess (Hinchey grade Ia) are generally included. However, although we also found studies in the literature that extend outpatient treatment to patients with abscesses ≤2–3cm (Hinchey grade Ib),9,11 these are not randomized studies and represent a smaller group of patients, making it difficult to draw conclusions.
Most authors or clinical guidelines do not make specific recommendations for outpatient treatment in cases of right acute diverticulitis, as it appears that the indication depends more on the severity of the episode than on the location. However, there are studies, such as that by Park et al.,11 in which ambulatory management for uncomplicated acute diverticulitis in the right colon also seems safe.
In the management of mild diverticulitis, antibiotics continue to be an important part of treatment. While in some protocols patients are discharged with a schedule of oral antibiotics for outpatient treatment, in others the administration of intravenous fluids and antibiotics for 24h is preferred before discharge.12
The most commonly used oral treatment regimen by the different authors continues to be the standard 7–10 days with amoxicillin-clavulanic acid vs 2nd or 3rd generation cephalosporins or quinolones plus metronidazole,12,13 although the regimens are heterogeneous according to the different centers. However, the latest Cochrane review15 concludes that there are no differences in outcomes between the different therapies, not even between the use/non-use of antibiotics. Likewise, different randomized studies16,17 demonstrate that, in the treatment of uncomplicated diverticulitis, the use of antibiotics —either by oral administration or short therapy (4 vs 7–14 days)—does not influence the rate of complications. In the same manner, the randomized multicenter trial (AVOD study)18 of 623 hospitalized patients concluded that antibiotic therapy does not accelerate patient healing or prevent recurrence. More recently, the results of the DIABOLO19 randomized multicenter study indicate that the use of antibiotics could be avoided in the first episode of uncomplicated acute diverticulitis (Hinchey Ia). However, there are currently no randomized studies that analyze the role of antibiotic therapy in the outpatient treatment of uncomplicated acute diverticulitis. Consequently, we do not yet have sufficient arguments to make recommendations about the administration of antibiotics or limits for use in these patients, and further studies will be necessary to abandon the recommendation of antibiotic treatment in the outpatient management of uncomplicated diverticulitis.
Evidence: outpatient treatment of uncomplicated acute diverticulitis is the optimal management for most patients since it has been shown to be safe, effective, and lower in cost (level of evidence 1b, grade of recommendation A).
Evidence: patients who are candidates for outpatient treatment should meet selection criteria, such as no signs of sepsis or significant comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, cardiac or kidney failure, immunosuppression), good tolerance of oral intake, and family support (level of evidence 1b, grade of recommendation A).
Evidence: although the use of antibiotic treatment could be limited in some cases of uncomplicated acute diverticulitis, there is insufficient evidence to abandon its routine use in the outpatient management of these patients (level of evidence 3, grade of recommendation C).
Hartmann's Procedure (HP)Since 1921, when Henri Hartmann first described his technique for the resection of sigmoid cancer, it has been modified and has become popular. It has also become the gold standard treatment in urgent resective surgery of the sigmoid colon, as it is a fast, reproducible technique that avoids the risk of anastomotic failure. However, the great disadvantage is the need for a stoma, requiring a second surgery to reconstruct the intestinal tract; meanwhile, in many cases the stoma becomes definitive.20
Despite the great advances made in surgical techniques and approaches, today HP continues to be within the therapeutic algorithm of complicated acute diverticulitis and is the most commonly used procedure in emergency surgery.21,22
In Hinchey grade III-IV diverticulitis, in which resection is indicated, there is great controversy about whether to use a primary anastomosis (PA) or a Hartmann's procedure (HP).
There are many studies on this subject, but all of them have selection bias and lack of randomization, so the conclusions are questionable at the very least.
In 2011, Roig20 published a multicenter retrospective study, spanning 5 years and studying 452 patients who underwent HP; 78.8% were emergency surgeries and 21.2% scheduled surgeries. 28.9% of the patients had diverticular disease. The purpose of the study was to analyze the rate of tract reconstruction, which was performed in 35.2% of patients with a median follow-up of 10 months. The reconstruction percentage was greater after emergency surgery and, in the isolated case of diverticulitis specifically, it reached almost 55%. Morbidity was not negligible, and the observed risk factors included: smoking, hypertension, hypoalbuminemia, ASA classification and surgeon specialization. The authors concluded that: HP may save lives, but its indications should be selective; PA in emergency surgery is feasible except in fecal peritonitis; and, not all surgeons are capable of performing emergency PA. A recent review of experts23 confirmed that contraindications for PA included fecal or purulent peritonitis associated with risk factors such as malnutrition, immunosuppression or hemodynamic instability. These findings are corroborated by Toro24 in a review that included 18 articles (none randomized) and by Mueller25 in 2011, which concluded that anastomotic leakage is more associated with patient comorbidity (ASA), than disease stage (intraoperative Hinchey). Other authors who compared HP or PA in urgently treated peritonitis excluded patients with septic shock, immunosuppression or ASA IV as candidates for PA.26
In a multicenter prospective study (12 hospitals), published in 2006 by Constantinides, 415 patients were treated surgically for complicated diverticulitis, using PA in 59.8 and HP in 40.2%. Out of the multiple variables studied, they concluded that emergency surgery, ASA and Hinchey classification and not being a colorectal surgeon are predictive factors for HP and that, even in the multivariate analysis, not being a colorectal surgeon continues to be a predictive factor for HP.27 However, the study carries a certain bias as it was not randomized: only the patients with worse baseline conditions and more advanced diverticulitis underwent HP. The importance of the surgeon has been emphasized by several studies.20,23
The first randomized study was not published until 2012.28 The design presented a methodologically correct structure: multicentric, prospective, with an estimated sample size of 300 patients in each arm: 300 PA and 300 HP. However, due to problems related with patients/family members as well as the surgeons themselves, specifically in the randomization of these patients operated on for perforated diverticulitis, only 15% of the estimated sample size was achieved: 90 patients, 34 PA with diverting stoma and 56 HP. No evidence was found of significant differences in terms of morbidity and mortality in the first intervention, but in the subsequent reconstructive surgery there was higher morbidity in the case of HP.
The first finalized randomized study29 was published in 2012. Four hospitals participated, and out of the 62 patients with perforated diverticulitis and purulent or fecal peritonitis included, 30 underwent HP and 32 underwent PA with protective diverting ileostomy. No significant differences were observed for either morbidity or mortality in both groups on the first intervention. Nonetheless, in the reconstruction, closure of the ileostomy was observed to be clearly superior versus colostomy in terms of percentage of closure, complication rate, operative time and hospital stay. In their conclusion, the authors suggested that it would be truly interesting to identify which patients could undergo PA without diverting ileostomy, as in those cases there would be a clear advantage of PA over HP. In any event, the sample size was too small to be able to draw any conclusions with elevated scientific evidence.
In 2015, a DELPHI study was published about the treatment of acute diverticulitis, which identified more points of controversy among the experts than agreement. In terms of surgery, the recommendations are that its choice is dictated by septic parameters and that HP is indicated in fecal peritonitis.30
- -
Evidence: the Hartmann procedure is indicated in urgent surgery for diverticular disease whenever there is hemodynamic instability, regardless of the degree of peritonitis; in generalized fecal peritonitis (Hinchey IV) and even in purulent peritonitis (Hinchey III) associated with risk factors for anastomotic dehiscence, such as immunosuppression, malnutrition (level of evidence 1b, grade of recommendation A).
The treatment of acute diverticulitis has progressed in recent years and the tendency is toward more and more conservative treatment. Possibly the greatest controversy is found in Hinchey III/IV diverticulitis, in which different procedures (HP, colon resection and anastomosis, or laparoscopic lavage and drainage) may play a role.
Laparoscopic lavage and drainage was published for the first time in 1996 by O'Sullivan with a series of 8 patients.31 Two had medical complications, but they all recovered with no need for later surgery. Since then, several studies have been completed to define its role in the treatment of complicated diverticulitis.
Currently, laparoscopic lavage and drainage is cited in the most recent clinical guidelines, despite the lack or scarcity of solid scientific evidence. Defenders of this technique indicate the main advantage is avoiding laparotomies and diverting procedures, thereby reducing subsequent complications. This is supported by less postoperative pain (and use of analgesia), fewer surgical site infections, potentially fewer incisional hernias, as well as an improved postoperative period. It is also argued that, if later colon resection is necessary, there are fewer adhesions after laparoscopic lavage, making surgery less complicated.32–34
During recent years, different systematic reviews have been published about the role of this treatment, with encouraging results. In this manner, Alamili et al.32 included 8 studies (none of them randomized) with a total of 213 patients. They included the cases of complicated diverticulitis with localized or generalized peritonitis and excluded those with fecal peritonitis, extensive generalized peritonitis, or the spontaneous observation of perforation. They presented a percentage of conversion of 3%, a mean stay of 9 days and 10% complications. During follow-up, 38% required elective surgery (sigmoid resection with primary anastomosis). Mortality was 1.4%. They concluded that lavage with antibiotics seems to be an alternative to radical surgery in selected patients.
In 2010, Toorenvliet et al.35 completed another systematic review with 2 keyword combinations: diverticulitis AND laparoscopy AND lavage; and, diverticulitis AND peritonitis AND laparoscopy. After a search of 411 articles and after dismissing those that were not relevant due to their title, summary or text, 13 studies were included (none of them randomized) with a total of 231 patients (77% Hinchey III). Abdominal and systemic sepsis were successfully controlled in 95.7% of patients. Mortality was 1.7% and morbidity 10.4%. Only 1.7% required ostomy. The authors concluded that, although there were no studies with high methodological quality, what has been published to date shows promising results with high efficacy, low mortality, low morbidity and minimal need for colostomy.
More recently, Cirocchi et al.36 published a review of 19 articles with 871 patients and concluded that peritoneal lavage can be considered a safe and effective option for the treatment of Hinchey stage III diverticulitis and that it can represent a “bridge procedure” with the objective of avoiding HP. This should be considered in patients without systemic toxicity and in hospitals with experience in minimally invasive surgery.
These initial results led to the development of 4 clinical trials (some of which have still not published results): the Ladies trial,37 DILALA trial,38 SCANDIV trial39 and LAP-LAND trial.40
The Ladies trial37 is a multicenter clinical trial based on the participation of more than 35 Dutch hospitals. The study has 2 arms (LOLA-arm and DIVA-arm) according to the type of peritonitis presented by each patient. Patients with purulent peritonitis were randomized between lavage plus laparoscopic drainage, HP or sigmoidectomy with PA (LOLA-arm). Those with fecal peritonitis were randomized between HP and resection with PA (DIVA-arm). One of the problems presented by this trial is that the recruitment of the LOLA-arm was suspended early on, in 2013, for safety reasons. Management data for 38 patients treated with lavage were published,41 with a morbidity and mortality of 44.7% in 4 patients (2 multiple organ failure, one aspiration and one inoperable lung carcinoma).
The DILALA trial38 is a Scandinavian clinical trial, in which the patients were randomized after laparoscopic confirmation of the diagnosis of Hinchey III acute diverticulitis in a laparoscopic lavage group and another HP group. The initial results have just been published42 of 83 patients (after exclusions, 39 in the lavage group and 36 in the HP group). The morbidity and mortality after lavage do not differ when compared with HP. The lavage requires less operative time (P<.0001), shorter recovery time in the recovery unit (4 vs 6h; P<.05) and shorter hospitalization (6 vs 9 days; P<.05). The authors concluded that, in Hinchey III patients, it is a safe and feasible treatment in the short term.
The SCANDIV trial39 is a multicenter clinical trial based on the participation of 21 hospitals from Sweden and Norway, whose results have been recently published. The patients are randomized into treatment groups of lavage plus drainage vs colon resection (randomization prior to surgery), with the inclusion of 199 patients (101 in lavage and 98 in colon resection). Severe complications in the following 90 days were not significantly different between the groups (30.7% in the lavage group vs 26% in the resection group; P=.56), and the mortality rate was 13.9% in lavage vs 11.5% in resection (P=.67). The percentage of re-intervention was significantly greater in the lavage group than in the resection group (20.3% vs 5.7%; P=.01). The authors concluded that, among patients with perforated diverticulitis and urgent surgery, the use of peritoneal lavage vs resection does not reduce severe complications and can worsen the results of the secondary objectives. These findings do not propose the use of the laparoscopic lavage for the treatment of perforated diverticulitis.
The last clinical trial (lapLAND trial)40 compares HP or resection with anastomosis and protective stoma vs laparoscopic lavage (randomization before laparoscopy). It was estimated that the study would be completed in December 2015, so the results should be published soon.
In this context, it could be concluded that laparoscopic lavage and drainage could be a therapeutic option in Hinchey III acute diverticulitis in selected patients; however, there is currently no solid evidence to support their use.
Evidence: in spite of there being several well designed, controlled and randomized studies, the results are controversial. Therefore, a recommendation cannot be made at this time based on the scientific literature.
Role of the Laparoscopic Approach in Colon Resection Due to Diverticular DiseaseElective SurgeryThe indications for elective surgery in diverticular disease have experienced an evolution in recent years, as it has been demonstrated that the risk of recurrence after an episode of diverticulitis resolved with medical treatment is actually lower than previously considered, even in young patients.43 Moreover, in those patients who present recurrence, the successive episodes are not necessarily more severe.44 Today, most clinical guidelines recommend individualizing the indication in patients who remain asymptomatic or oligosymptomatic between episodes.1,5 The need for elective surgery seems clearer and less controversial in cases of complicated diverticular disease (stenosis, fistulae).1
Regarding the type of approach, there is currently sufficient evidence to recommend laparoscopy as an approach of choice in elective resective surgery due to diverticular disease, and it is thus recommended in the guidelines of several scientific societies.1,45 The results of the 3 randomized clinical trials and one meta-analysis that include the majority of the case series published to date show evidence that laparoscopy is associated with less postoperative mortality and morbidity, shorter hospitalizations, and a tendency toward lower overall cost.46–48 The first double-blind randomized clinical assay comparing both approach modalities, the Sigma trial,46 included 104 patients with 2 or more previous episodes of Hinchey I and II diverticulitis, diverticular bleeding or symptomatic stenosis, from 5 hospitals with experience in laparoscopic colorectal surgery. The conversion rate to open surgery was 19%. Although the overall morbidity was similar in both groups (42.3% vs 53.8%; P=.2), the laparoscopic group had fewer complications defined by the authors as important (anastomotic dehiscence, intraabdominal abscess, intraabdominal bleeding, evisceration, small bowel lesion, acute myocardial infarction and pulmonary thromboembolism) (9.6% vs 25%; P=.038), less pain and shorter hospitalization (5 vs 7 days; P=.046), compared to the open surgery group. In the long-term follow-up (6 months), whose results were published subsequently,49 there were no differences in quality of life measured by the SF-36 between the 2 groups, beyond a greater satisfaction with the esthetic results in the laparoscopic group, but a reduction of 27% was seen in the overall 6-month morbidity compared to the open approach (17% vs 44%; P=.003).
Afterwards, 2 additional randomized trials have been published that did not show a significant difference in the results, but these studies had difficulties in the recruitment due to the preference of the patients for laparoscopic surgery.47,48 One of them included a study of costs that demonstrated a tendency toward less expenditure in the laparoscopic group (including the treatment of complications with a mean follow-up of 30 months, especially incisional hernias), but without reaching statistical significance.47 The most complete meta-analysis50 analyzed 22 cases series (including the Sigma trial), with a total of 10,898 patients, 1538 of which (14%) underwent a laparoscopic approach (overall rate of conversion 8.4%). The authors concluded that elective laparoscopic resection in diverticular disease is safe, presents less overall morbidity (RR 0.56; [0.4–0.8]; P=.001) and has faster postoperative recovery compared to the conventional open approach, with no differences in terms of mortality or later recurrence of the diverticular disease.50 Nonetheless, they recognized the need to differentiate between cases in which surgery is indicated due to recurrent episodes of uncomplicated diverticulitis and those in which the indication is the presence of fistula or stenosis. According to a comparative study that included 203 laparoscopic resections, 91 of which were due to complicated diverticular disease, in recent years the rate of conversion tends to be higher (1.8% vs 9.9%; P=.02), as is the morbidity associated with resection; however, the differences are not statistically significant (16.1% vs 26.4%; P=.10).51 Nonetheless, despite the controversy that still exists, laparoscopic resection in these more complex cases seems safe and provides results comparable to uncomplicated cases at hospitals with sufficient experience.45
Evidence: elective laparoscopic resection of the sigmoid colon in uncomplicated cases of diverticular disease is safe and provides benefits for patients compared to the conventional open approach (level of evidence 1, grade of recommendation A).
Evidence: in cases that are complicated by the presence of fistulae or associated stenosis, elective laparoscopic resection can also be appropriate at hospitals with sufficient experience in laparoscopic surgery (level of evidence 3, grade of recommendation C).
Urgent SurgeryAlthough laparoscopic surgery has shown clear benefits over traditional open surgery in elective surgery due to diverticular disease, until now no consensus has been reached about the role that laparoscopic resection can play in the urgent treatment of perforated diverticulitis.1 There are no randomized clinical trials comparing both resective surgery modalities in the context of urgent surgery: the evidence is limited to short series of prospective cases or retrospective reviews of multicentric databases, mainly with cases of 2-stage laparoscopic surgery (urgent laparoscopic HP and reconstruction of the posterior tract).
Laparoscopic HP has been proposed as an option with less morbidity than open HP in cases of perforated diverticulitis (Hinchey III and IV), without hemodynamic instability.52 Theoretically, this approach allows for faster recovery with less patient morbidity and would likewise simplify posterior reconstructive surgery, which ideally could also be done laparoscopically with low conversion rates, at least according to the experiences published in recent years by reference hospitals.53 Nonetheless, in a retrospective study of 1236 HP due to perforated diverticulitis, 70 of which (5.6%) were done laparoscopically, no significant reduction was found in mortality (4.5% vs 3%) or morbidity (30% vs 25%) compared to the open approach, even though a statistical analysis was completed to minimize the impact of confounding factors due to selection bias (for instance, the most serious patients underwent open HP more frequently).54
The most recent review about this unresolved question includes 5 case series with 104 patients,55 in which 84 laparoscopic HP and 20 laparoscopic PA were carried out. Overall mortality was 3%, with an overall morbidity of 21% and a conversion rate of 13.5%. It is relevant to emphasize that 76% of the patients who underwent HP were offered tract reconstruction surgery in a second stage, and in all cases this second procedure was able to be done laparoscopically (0% conversion). However, this study probably represents the results from hospitals with great experience, so they should be interpreted with caution.
In fact, the current reality is that the use of the laparoscopic approach in this context is minor. According to the analysis of a large multicenter database of 67,645 patients treated with urgent sigmoid resection for perforated diverticulitis in the United States between 2003 and 2007, only 3.9% were treated laparoscopically, with an elevated conversion rate (55%).56 The rates are probably similar in our country (Spain).
As the development and training of surgeons in laparoscopic surgery grows, these percentages are likely to increase. In spite of everything, with the evidence that is currently available, it has yet to be demonstrated whether the benefits of the laparoscopic approach of elective surgery are extendable to the context of patients requiring urgent surgery for peritonitis.
Evidence: urgent laparoscopic resection of the sigmoid colon in cases of perforated diverticulitis with generalized peritonitis is feasible in experienced hands, but there is not sufficient evidence to recommend it as an approach of choice (level of evidence 3, grade of recommendation C).
Conflict of InterestsThe authors have no conflict of interests to declare.
We would like to express our gratitude to the Scientific Committee and the members of the Board of Directors of the AECP for their contributions and collaboration. Their assistance has been invaluable in the search for the greatest consensus.
Please cite this article as: Rosado-Cobián R, Blasco-Segura T, Ferrer-Márquez M, Marín-Ortega H, Pérez-Domínguez L, Biondo S, et al. Enfermedad diverticular complicada: toma de posición sobre tratamiento ambulatorio, intervention de Hartmann, lavado-drenaje peritoneal y cirugía laparoscópica. Documento de consenso de la Asociación Española de Coloproctología y Sección de Coloproctología de la Asociación Española de Cirujanos. Cir Esp. 2017;95:369–377.