Ischemia of the gastric conduit after esophagectomy represents a setback that increases the risk of anastomotic leak. In order to prevent this severe complication, a surgical alternative has been proposed which consists in delaying the reconstruction until gastric perfusion improves. By adopting this strategy we can avoid two other surgical options that may significantly increase the risk of complications: (1) performing an esophagogastrostomy with a poorly perfused gastric tube and (2) resecting the gastric conduit followed by a complex reconstruction.
La comprobación de una isquemia del tubo gástrico al terminar una esofagectomía es un contratiempo que incrementa el riesgo de dehiscencia de la anastomosis esofagogástrica. Para prevenir esta grave complicación, se ha propuesto como opción quirúrgica alternativa diferir la anastomosis el tiempo necesario para que se recupere la irrigación gástrica. De este modo se evitarían otras 2 opciones quirúrgicas que acarrean graves riesgos para el paciente: 1) realizar la anastomosis esofagogástrica en un estómago con una vascularización precaria y 2) la resección del tubo gástrico con una posterior reconstrucción muy compleja.
The most commonly used type of digestive tract reconstruction after esophagectomy is the ascension of the digestive tube and esophagogastric anastomosis, which can be performed at the cervical or upper thoracic level. The arterial irrigation of this “tubulized” stomach depends on the right gastroepiploic arcade, gastric arterial flow and microvasculature. This means that the most proximal end of the digestive tube can present different degrees of ischemia that may favor the development of anastomotic dehiscence and put the patient's life at risk.
An alternative, infrequently used technique has been reported that surgeons can use when ischemia of the digestive tube is detected. We present such a case.
Case ReportThe patient was a 64-year-old male with a history of alcohol-related cirrhosis (Child–Pugh A), chronic obstructive pulmonary disease, type 2 diabetes, arterial hypertension, dyslipidemia, obesity (BMI 33kg/m2) and cancer of the glottis and supraglottis treated with radiotherapy in 2007. During a follow-up endoscopy of his liver disease, a depressible and friable lesion measuring 2.5cm was observed 20cm from the dental arches. Biopsy demonstrated the mass to be a low-grade squamous-cell carcinoma with early-stage infiltration of the lamina propria. The extension study did not identify any locoregional or distant dissemination. The case was presented to the Upper GI Tract Tumors Committee, and surgical treatment was decided. Prior to surgery, the patient underwent 6 weeks of cardiopulmonary training for functional optimization, reaching a significant increase in oxygen uptake and maximum tolerated load.
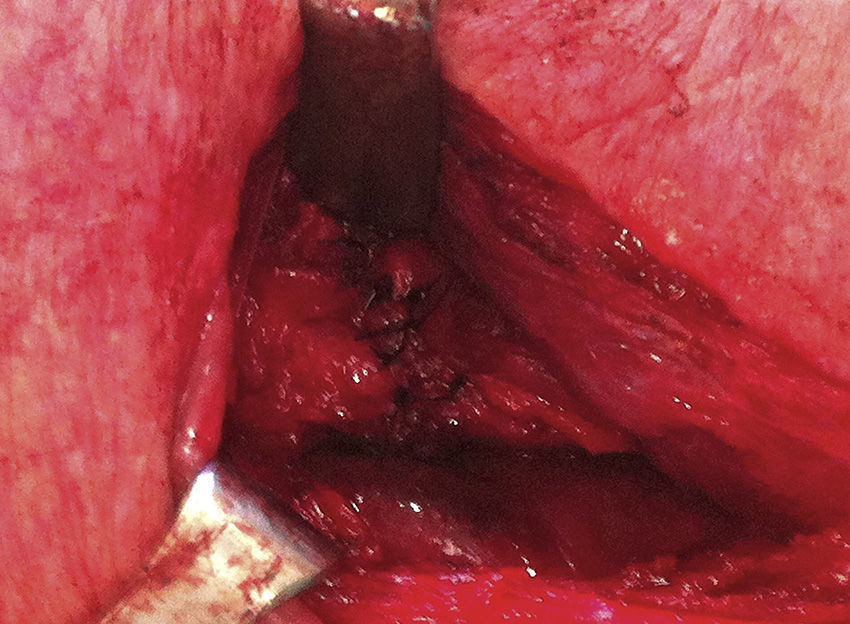
Surgical TechniqueWe performed transhiatal esophagectomy in 2 stages. In the abdominal stage, the entire stomach was mobilized, freeing the greater omentum along the greater curvature, while preserving the right gastroepiploic arcade and resecting the short gastric vessels and the left gastric artery. The esophagus was mobilized until above the tracheal carina. By means of a left cervicotomy, the cervical esophagus was released, the mass was identified and the esophagus was dissected 3cm under the cricopharyngeal muscle. The intraoperative pathology study confirmed a tumor-free resection margin of 2cm. After tubulization of the stomach, we performed pyloroplasty and drew the digestive tube up into the neck. At this time, we observed ischemia of the digestive tube, which was more evident at the upper edge. This was ratified after a gastrotomy and visualization of the mucosa. We decided not to carry out the esophagogastric anastomosis at that time and to delay the procedure until a later date. The proximal end of the digestive tube was removed, including the gastrotomy, with a mechanical stapler. This end was secured with a stitch of non-absorbable monofilament (Prolene® 2/0), which was exteriorized to serve as a reference point through the cervicotomy. An end esophagostomy was created and the cervicotomy was closed (Fig. 1). In addition, a feeding jejunostomy was performed.
The patient had a favorable recovery and was discharged from the hospital 11 days after surgery, with scheduled outpatient visits. The histopathologic study revealed a squamous carcinoma that infiltrated the submucosa surface (T1b-sm1), with no lymph node involvement and negative margins.
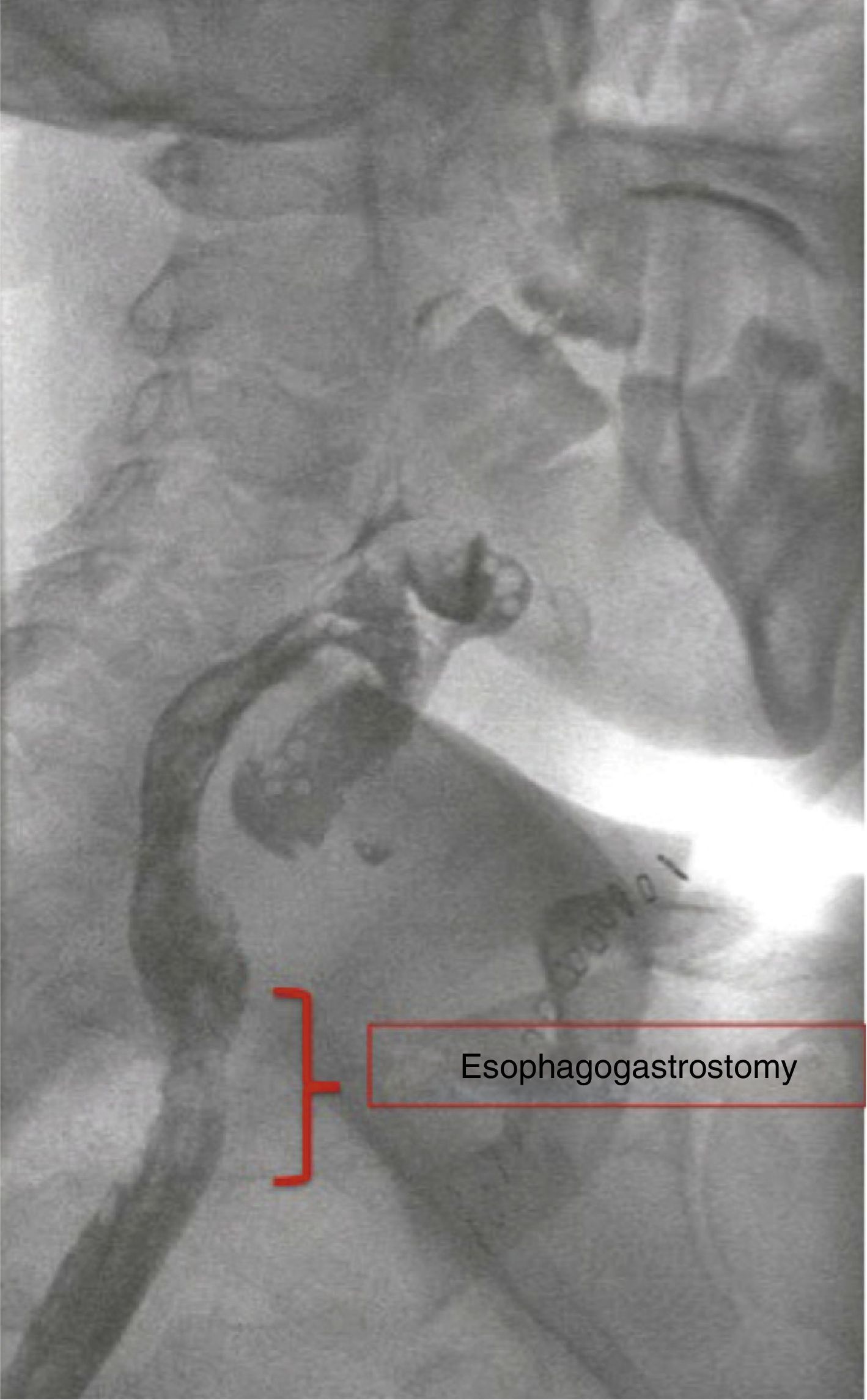
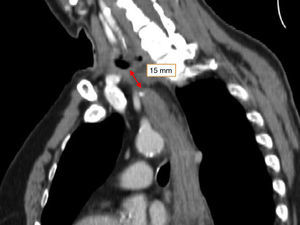
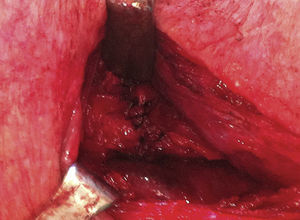
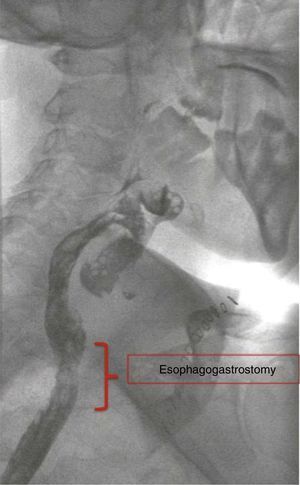
Eight weeks later, a thoracoabdominal computed tomography scan showed the esophagostomy in the lower left portion of the neck at a distance of 15mm from the upper end of the tubulized stomach. There was good uptake of the intravenous contrast medium at this level (Fig. 2). Given these findings, the cervicotomy was re-examined to reconstruct the digestive tract. There was evidence of good irrigation of the stomach, and the esophagogastric anastomosis was performed (Fig. 3). The patient's evolution during the postoperative period was uneventful. The anastomosis was checked with an upper GI series using contrast and fluoroscopy, which showed proper passage of the contrast material with no stenosis or filtrations (Fig. 4).
Patients who undergo esophagectomy are frequently older and have several comorbidities (diabetes, hypertension, chronic obstructive pulmonary disease, cardiac arrhythmia) or have been treated with neoadjuvant therapies. This situation, in conjunction with ischemia of the digestive tube that has been ascended for reconstruction of the tract, can lead to anastomotic filtration, sepsis or multiple organ failure and put the patient's life at risk.
In 2009, Oezcelik et al.1 published a strategy for the management of patients who had undergone esophagectomy and presented with ischemia of the digestive tube before creating the esophagogastric anastomosis. The technique entails delaying the anastomosis and leaving the digestive tube closed within the neck with a Prolene® 2/0 suture in the more proximal end of the stomach. The suture is exteriorized to serve as a guide for the esophagogastric reconstruction. In addition, a cervical esophagostomy is constructed and a jejunostomy is placed for feeding. Ninety days after esophagectomy, esophagogastrostomy is performed through the previous cervicotomy and the Prolene® 2/0 suture is used as a guide to locate the digestive tube.
The aim of this strategy is to consolidate the irrigation of the gastric tube using a process of ischemic conditioning.2–4 Oezcelik et al.1 reported a series of 35 patients who had been treated with this technique, and all of them had good irrigation of the gastric conduit at the time of the esophagogastric reconstruction, with no dehiscence, skin infections or postoperative sepsis. Three patients had stenosis, which was treated by dilation.
More than 20 years ago, other authors described the so-called “two-staged esophagectomy” in patients with high surgical risk: initial esophageal resection and cervical esophagogastrostomy 2–3 weeks later.5 The objective of this strategy was to reduce the complications associated with traditional esophagectomy in a single procedure, but without originally contemplating its application in patients with evident ischemia of the digestive tube in an attempt to recuperate its vascularization and proceed with reconstruction at a later time.
Despite the disadvantages of this strategy (2 interventions, esophagostomy and jejunostomy), its safety and effectiveness (as seen in the results of Oezcelik et al.1 and our case report) make it a possibility versus other options, such as anastomosis in a digestive tube with doubtful viability or resection of the digestive tube and later colonic interposition, which present higher morbidity and mortality rates.
Please cite this article as: Lanzarini E, Ramón JM, Grande L, Pera M. Esofagogastrostomía cervical diferida: Una opción técnica cuando se evidencia isquemia del tubo gástrico en el momento de la esofagectomía. Cir Esp. 2014;92(6):429–431.