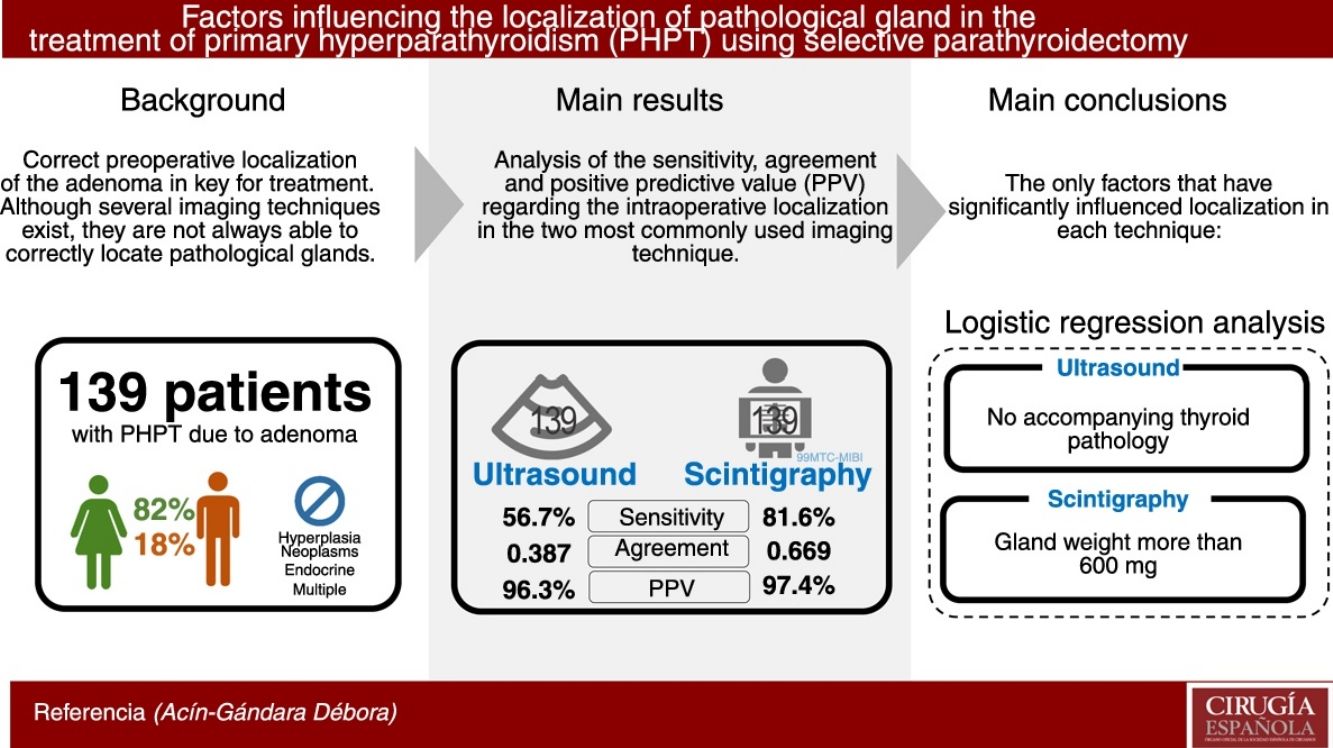
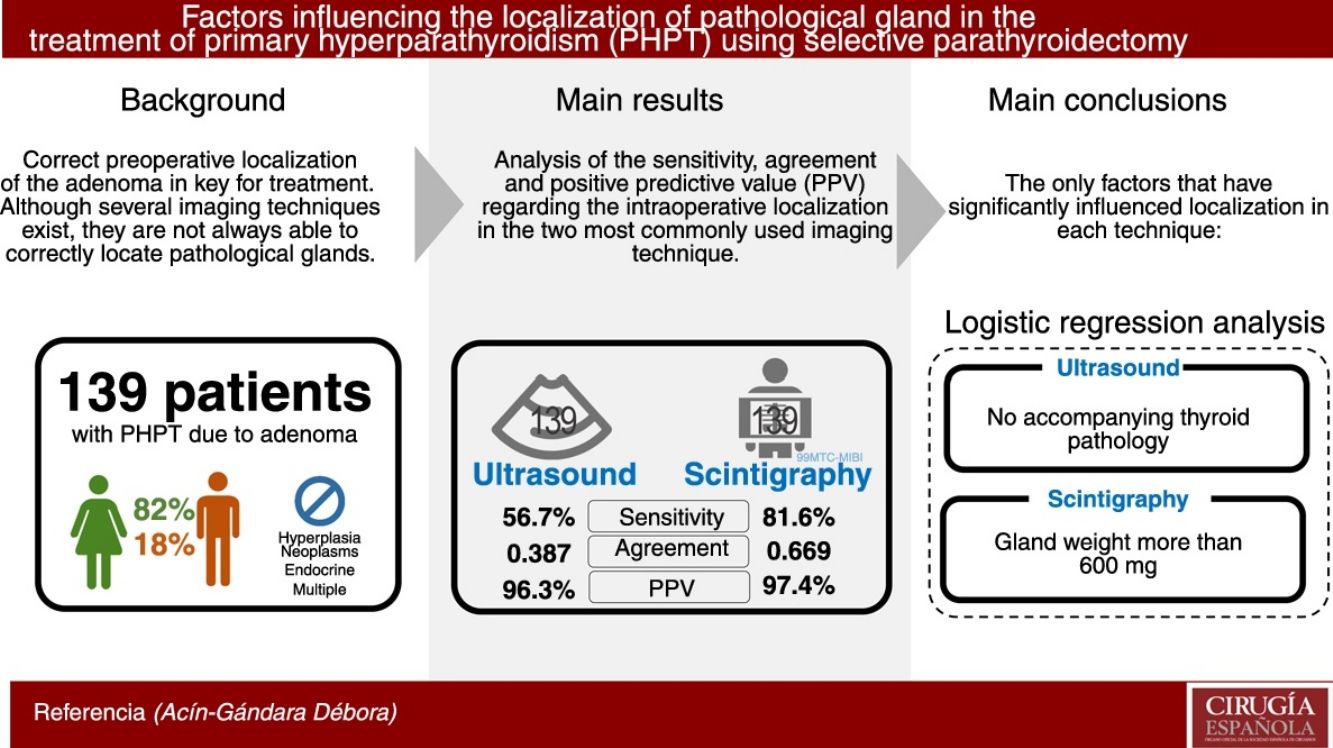
The treatment of choice for primary hyperparathyroidism (PHPT) when there is proper preoperative localization of the adenoma is minimally invasive parathyroidectomy. However, imaging techniques are not always able to provide the exact location. The objective is to identify potential factors that might influence the sensitivity and concordance of ultrasound (US) and 99mTc-methoxy-isonitrile parathyroid scintigraphy (MIBI-PS) and the actual location of the adenoma.
MethodsWe reviewed the data of patients who underwent parathyroidectomies for PHPT. All patients had undergone ultrasound and 99mTc-MIBI scintigraphy as a preoperative location study. Multiple endocrine neoplasms, other hyperplasias and non-cervical ectopic adenomas were excluded. The sensitivity, PPV and concordance have been estimated for the location of the gland in both tests compared with the intraoperative location, using a multivariable analysis of the factors that might influence their localization capacity.
Results139 patients (82% women) have been analysed. The US sensitivity was 56.7%, concordance (Kappa index) 0.387 and PPV 96.3%. The MIBI-PS sensitivity was 81.6%, the concordance (Kappa index) 0.669 and the PPV 97.4%. The factor that improved localization of the glands by US in the multivariable analysis was the absence of a concomitant thyroid pathology. The factor that improved the MIBI-PS results was a gland weight greater than 600 mg.
ConclusionsUS sensitivity improves when there is no concomitant thyroid pathology. MIBI-PS sensitivity improves when the gland weight is greater than 600 mg.
Una correcta localización preoperatoria del adenoma es clave en el tratamiento del hiperparatiroidismo primario (HPTP) mediante paratiroidectomía selectiva. Aunque existen múltiples técnicas de imagen, no siempre consiguen localizar correctamente la/s glándula/s patológica/s. El objetivo es estudiar los factores que puedan influir en la sensibilidad y la concordancia de la ecografía y la gammagrafía 99mTc-metoxi-isobutil-isonitrilo (MIBI).
MétodosPoblación a estudio: pacientes intervenidos con HPTP por adenoma con studio preoperatorio de localización con ecografía y gammagrafía 99mTc-MIBI. Los pacientes fueron tratados en nuestro centro entre 2004 y 2018. Se han excluido a los que no tuvieran ambas pruebas, las hiperplasias, las neoplasias endocrinas múltiples (MEN) y los adenomas ectó picos no abordables por vía transcervical. Se han estimado la sensibilidad, la concordancia y el valor predictivo positivo (VPP) de las técnicas de imagen con respecto a la localización intraoperatoria, analizando los potenciales factores que pueden influir en ello.
ResultadosSe ha analizado a 139 pacientes (82% mujeres, 18% varones). La ecografía ha tenido una sensibilidad del 56,7%, una concordancia (índice kappa) de 0,387 y un VPP del 96.3%. En el caso de la gammagrafía, la sensibilidad ha sido del 81,6%, la concordancia (índice kappa) del 0,669 y su VPP del 97,4%. En el análisis de regresión logística, el factor que ha influido en la localización mediante ecografía ha sido la ausencia de enfermedad tiroidea asociada. En el caso de la gammagrafía, el factor ha sido el peso glandular mayor de 600 mg.
ConclusionesLa sensibilidad de la ecografía mejora en ausencia de enfermedad tiroidea y la de la gammagrafía con el peso glandular mayor de 600 mg.
The treatment of choice in primary hyperparathyroidism (PHPT) due to a parathyroid adenoma is selective parathyroidectomy, provided there is correct preoperative localization. Ultrasound and 99mTc-MIBI scintigraphy are the most commonly used imaging techniques, but they do not always manage to correctly locate the pathological gland.
When there is agreement between the location of the adenoma on ultrasound and scintigraphy, the positive predictive value (PPV) is very high, making selective parathyroidectomy possible.1–3
Both tests have varying sensitivities reported in the literature: ultrasound ranges between 53 and 93%,1,4–8 and 99mTc-MIBI scintigraphy between 50% and 85%.5,7–10 In addition, there has been some debate about the factors that may influence gland localization with these techniques, such as adenoma size, ectopic glands, coexistence of thyroid disease and even preoperative calcium and PTH levels.1,6,11–17
The combination of ultrasound and scintigraphy is usually sufficient for preoperative localization, but in cases of difficult diagnosis (ectopic glands, persistence or recurrence), other imaging tests can be used:
- –
Single photon emission tomography/computed tomography (SPECT/CT) provides more precise localization. Its sensitivity (84%–95%) is greater than that of 99mTc-MIBI scintigraphy.18,19
- –
CT and magnetic resonance imaging (MRI) have a reported sensitivity of 46–8720 and 80%,12 respectively.
- –
Choline PET has a sensitivity of 96%–100% and a PPV of 96.3%–100%.8,10
The objective of the study is to analyze the factors influencing the validity and concordance of ultrasound and 99mTc-MIBI scintigraphy for the preoperative localization of pathological parathyroid gland(s) in PHPT due to adenoma.
MethodsPopulation under study: patients who underwent PHPT due to adenoma between 2004 and 2018, with preoperative localization studies using ultrasound and 99mTc-MIBI scintigraphy. We excluded from those study patients who did not have both tests and those with secondary or tertiary hyperparathyroidism, parathyroid hyperplasia, multiple endocrine neoplasms (MEN) and ectopic adenomas not accessible transcervically.
During the study period, the ultrasound examinations were performed by 6 radiologists who used 2 ultrasound machines by General Electric (Healthcare España, S.A.) (LOGIQ™S7 XDclear™ and LOGIQ™S8 XDclear™2.0+) with 10 and 12 MHz frequency probes.
The scintigraphy studies were conducted using the Millennium Gamma Camera by General Electric (Healthcare España, S.A.) by 2 Nuclear Medicine specialists. The technique involves the intravenous administration of 20mCi of 99mTc-MIBI, obtaining planar images after 10 and 120 min (initial thyroid phase/late parathyroid phase) and tomographic images after 60 min.
Data were recorded for the following study variables: gender, age, gland weight (mg), calcemia (mg/dL), preoperative PTH (pg/mL) and 25-OH vitamin D (ng/mL), presence of associated thyroid disease, altered thyroid function, previous cervical surgery, imaging tests performed, localization of the lesion in each imaging test, type of surgical intervention performed, localization of the intraoperative lesion and associated surgical procedures.
For the statistical analyses requiring it, the quantitative variables were stratified into dichotomous variables, taking into account clinical criteria: preoperative calcium (cut-off point 12 mg/dL), preoperative PTH (174 pg/mL), preoperative 25-OH vitamin D (30 ng/mL) and gland weight (greater than 600 mg, because several publications confirm a greater number of false negatives [FN] when using scintigraphy for localization when the weight is less than this figure).16,17,21
The qualitative variables that were not dichotomous, such as associated thyroid disease, have been grouped as yes/no.
Statistical AnalysisWe estimated the sensitivity, PPV and agreement of both tests for intraoperative localization. Localization was considered correct when the imaging test correctly identified the side where the pathological gland was located.
Quantitative variables are presented with their median and interquartile range (IQR), and qualitative variables are expressed with their frequency distribution.
To determine whether there were clinical characteristics that could influence the ability to detect adenomas, the kappa agreement indices were studied, stratified by the presence of accompanying thyroid disease, impaired thyroid function, previous cervical surgery, gland weight, preoperative calcium and PTH levels, testing the homogeneity of kappa statistics.
Likewise, the stratified sensitivity was calculated for each of the previously mentioned variables regarding the intraoperative localization of the lesion, and the crude odds ratio (OR) as well as the OR for each stratum analyzed have been estimated.
Two predictive logistic regression models have been performed to determine which of these factors independently influence the concordance and sensitivity of ultrasound and scintigraphy for localizing lesions.
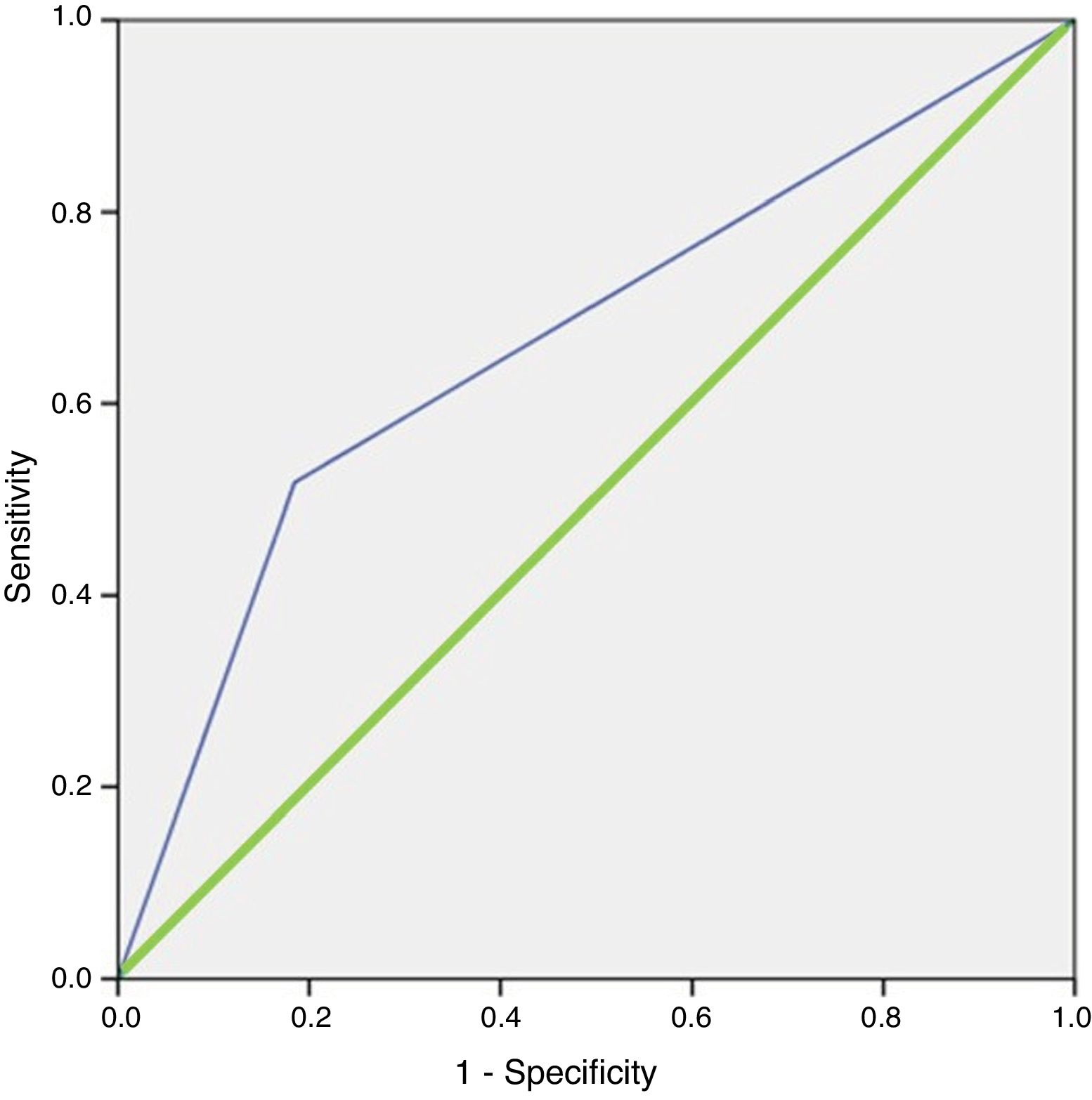
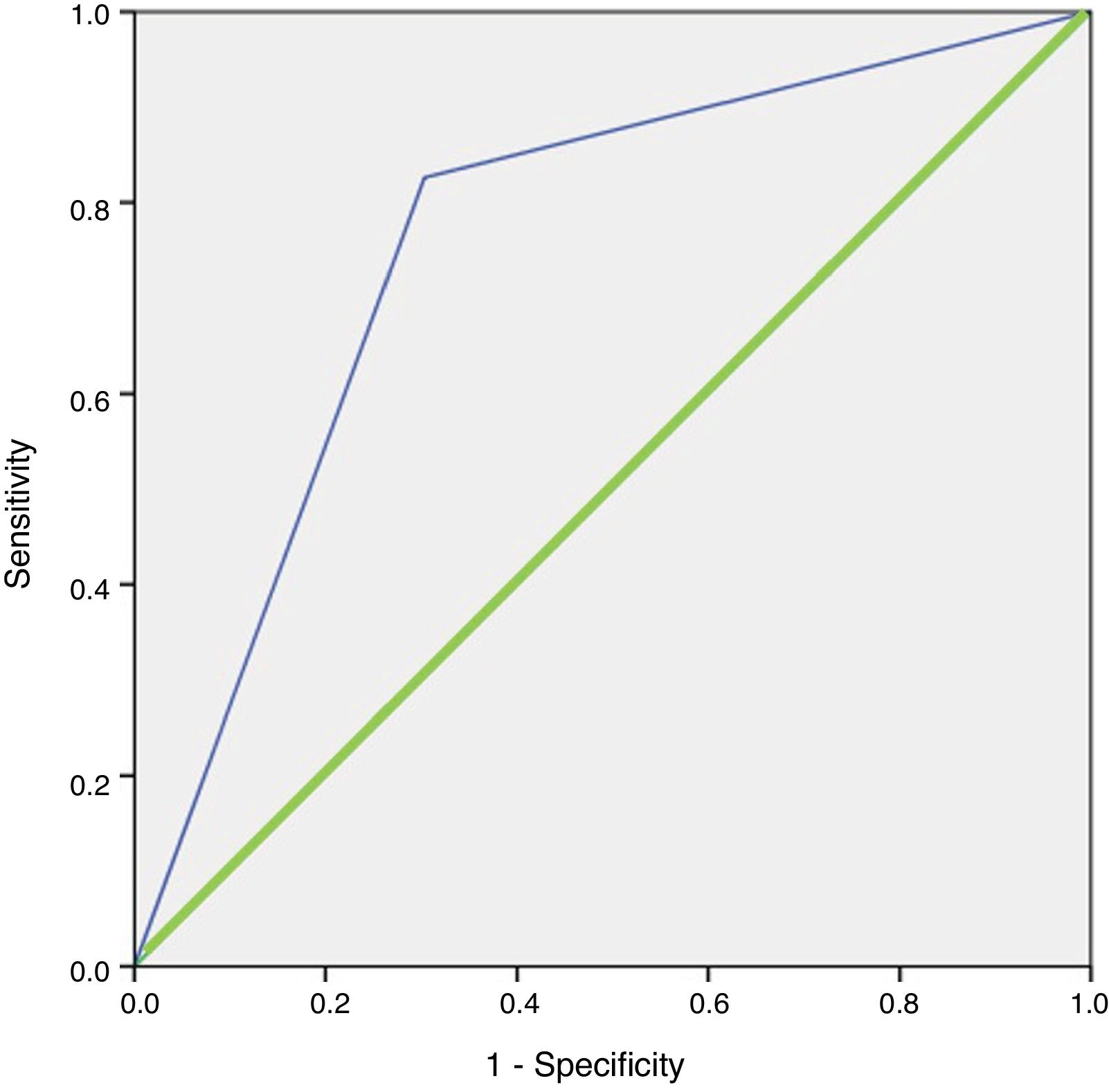
Finally, the ROC curves were plotted, and the area under the curve for the values predicted by the model was estimated. Likewise, goodness of fit was assessed with the Hosmer–Lemeshow test.
In all statistical analyses, p values <0.05 were considered statistically significant, and the results are presented with their 95% confidence intervals. For the statistical analyses, we used SPSS 21 statistical software (SPSS, Chicago, Illinois, USA) and the Epidat program for epidemiological data analysis (Version 4.2, July 2016; Consellería de Sanidade, Xunta de Galicia, Spain; Pan American Health Organization [PAHO-WHO]; CES University, Colombia).
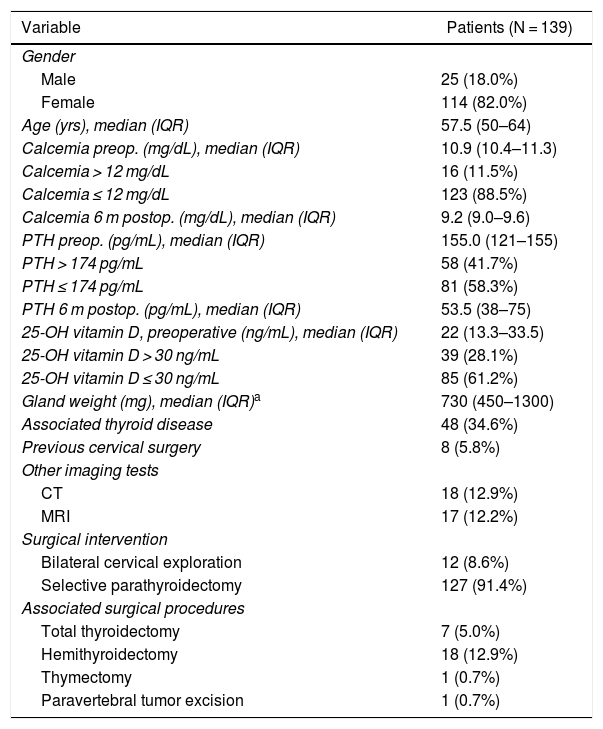
ResultsWe have analyzed a total of 139 patients who had been treated surgically for adenoma and had undergone ultrasound studies as well as 99mTc-MIBI scintigraphy as preoperative localization studies. The descriptive analysis of the series is shown in Table 1.
Descriptive Analysis With Demographic and Preoperative Data.
| Variable | Patients (N = 139) |
|---|---|
| Gender | |
| Male | 25 (18.0%) |
| Female | 114 (82.0%) |
| Age (yrs), median (IQR) | 57.5 (50–64) |
| Calcemia preop. (mg/dL), median (IQR) | 10.9 (10.4–11.3) |
| Calcemia > 12 mg/dL | 16 (11.5%) |
| Calcemia ≤ 12 mg/dL | 123 (88.5%) |
| Calcemia 6 m postop. (mg/dL), median (IQR) | 9.2 (9.0–9.6) |
| PTH preop. (pg/mL), median (IQR) | 155.0 (121–155) |
| PTH > 174 pg/mL | 58 (41.7%) |
| PTH ≤ 174 pg/mL | 81 (58.3%) |
| PTH 6 m postop. (pg/mL), median (IQR) | 53.5 (38–75) |
| 25-OH vitamin D, preoperative (ng/mL), median (IQR) | 22 (13.3–33.5) |
| 25-OH vitamin D > 30 ng/mL | 39 (28.1%) |
| 25-OH vitamin D ≤ 30 ng/mL | 85 (61.2%) |
| Gland weight (mg), median (IQR)a | 730 (450–1300) |
| Associated thyroid disease | 48 (34.6%) |
| Previous cervical surgery | 8 (5.8%) |
| Other imaging tests | |
| CT | 18 (12.9%) |
| MRI | 17 (12.2%) |
| Surgical intervention | |
| Bilateral cervical exploration | 12 (8.6%) |
| Selective parathyroidectomy | 127 (91.4%) |
| Associated surgical procedures | |
| Total thyroidectomy | 7 (5.0%) |
| Hemithyroidectomy | 18 (12.9%) |
| Thymectomy | 1 (0.7%) |
| Paravertebral tumor excision | 1 (0.7%) |
Bilateral cervical exploration was indicated in patients: with no adenoma localized on ultrasound or scintigraphy (10 patients) and with discordant imaging study results or double adenomas (2 patients). In addition, 6 of these patients also required hemithyroidectomy or total thyroidectomy for thyroid disease. The associated procedures were performed due to concomitant pathological findings (papillary or follicular carcinoma, multinodular goiter, thyroid nodule and a paravertebral schwannoma).
The pathology results confirmed adenoma in all patients, although it cannot always be differentiated from hyperplasia in the absence of exploration of the remaining glands. The median (IQR) gland weight was 730 mg (450–1300).
UltrasoundUltrasound identified one or more pathological glands in 80 cases (57.6%), 77 of which coincided with the surgical location (true positives [TP]) and 3 did not (false positives [FP]). Ultrasound did not identify 59 glands (FN). With these data, the sensitivity of the ultrasound was 56.7% (Table 2), with a PPV of 96.3%. The specificity and the NPV could not be estimated, since all the operated patients had an injury and there was no true negative (TN) in the sample.
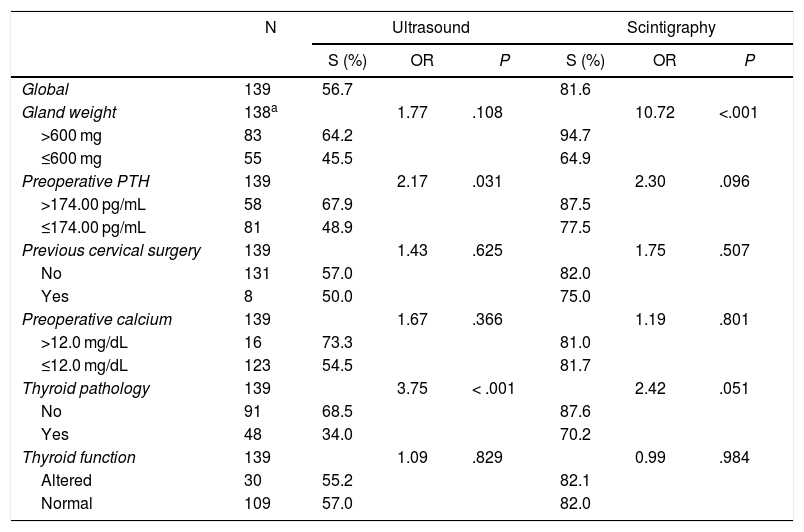
Sensitivity (S) and Odds Ratio (OR) of Localization Using Ultrasound and 99 mTc-MIBI Scintigraphy vs. Intraoperative Localization.
| N | Ultrasound | Scintigraphy | |||||
|---|---|---|---|---|---|---|---|
| S (%) | OR | P | S (%) | OR | P | ||
| Global | 139 | 56.7 | 81.6 | ||||
| Gland weight | 138a | 1.77 | .108 | 10.72 | <.001 | ||
| >600 mg | 83 | 64.2 | 94.7 | ||||
| ≤600 mg | 55 | 45.5 | 64.9 | ||||
| Preoperative PTH | 139 | 2.17 | .031 | 2.30 | .096 | ||
| >174.00 pg/mL | 58 | 67.9 | 87.5 | ||||
| ≤174.00 pg/mL | 81 | 48.9 | 77.5 | ||||
| Previous cervical surgery | 139 | 1.43 | .625 | 1.75 | .507 | ||
| No | 131 | 57.0 | 82.0 | ||||
| Yes | 8 | 50.0 | 75.0 | ||||
| Preoperative calcium | 139 | 1.67 | .366 | 1.19 | .801 | ||
| >12.0 mg/dL | 16 | 73.3 | 81.0 | ||||
| ≤12.0 mg/dL | 123 | 54.5 | 81.7 | ||||
| Thyroid pathology | 139 | 3.75 | < .001 | 2.42 | .051 | ||
| No | 91 | 68.5 | 87.6 | ||||
| Yes | 48 | 34.0 | 70.2 | ||||
| Thyroid function | 139 | 1.09 | .829 | 0.99 | .984 | ||
| Altered | 30 | 55.2 | 82.1 | ||||
| Normal | 109 | 57.0 | 82.0 | ||||
We analyzed the influence of the clinical variables, and only the absence of thyroid disease and PTH greater than 174 pg/mL were significantly associated with an improvement in the sensitivity and OR of the ultrasound (Table 2).
In the multivariable analysis, the only factor that influenced the location of the lesion was the absence of thyroid disease, with an OR of 3.567 (95% CI, 1.705–7.464). The area under the curve of the model was 0.666 (95% CI, 0.569–0.764). The model correctly classified 77.5% of the cases and had a sensitivity of 68.8% compared to what was observed with ultrasound (Fig. 1). The model demonstrated goodness of it, with a Hosmer-Lemeshow test p value = 0.437.
99mTc-MIBI ScintigraphyScintigraphy located one or more pathological glands in 114 cases (82%), 111 of which coincided with the surgical location (TP) and 3 did not (FP). The sensitivity of the scintigraphy was 81.6% (Table 2) and its PPV was 97.4%. The specificity and NPV could not be estimated because there was no TN.
As for the analysis of the detection capacity of the clinical variables studied, a gland weight greater than 600 mg improved the sensitivity and the OR of the scintigraphy, with statistically significant differences (Table 2).
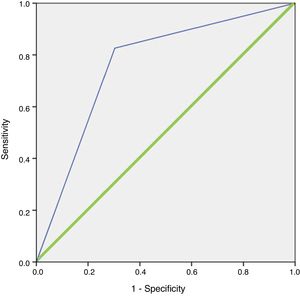
In the logistic regression analysis, this finding was confirmed, with an OR for locating the lesion when the weight was greater than 600 mg of 10.721 (95% CI, 3.397–33.837; p < 0.001). The model correctly classified 84.3% of the cases with a sensitivity of 100% versus what was observed with scintigraphy. The area under the curve of the resulting model after including these variables was 0.762 (95% CI, 0.656–0.867) (Fig. 2). The model demonstrated goodness of fit, with a Hosmer–Lemeshow p value = 0.151.
ROC curve of the logistic regression model for 99 mTc-MIBI scintigraphy.
Blue line (thin): representation of the ROC curve of the logistic regression model for 99mTc-MIBI scintigraphy. Green line (thick): representation of the reference line of a test with no discriminating capacity.
When we analyzed the concordance between the two imaging tests, the kappa index was 0.472 (95% CI, 0.367–0.578). Only 89 cases coincided in the diagnosis, with a sensitivity of 78.65% and a PPV of 100%.
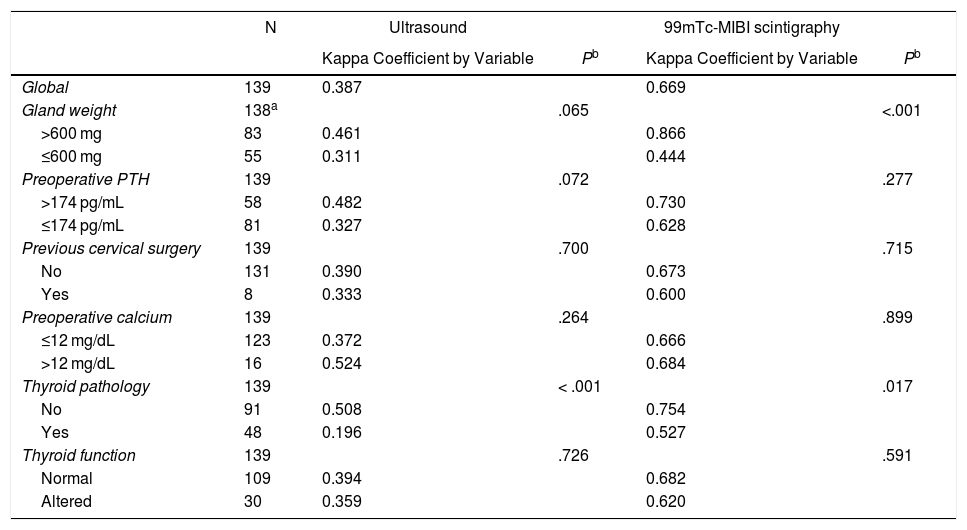
The kappa index between ultrasound and intraoperative localization was 0.387 (95% CI, 0.306–0.468), improving agreement and with statistically significant differences in the absence of thyroid disease (Table 3).
Agreement Between Localization by Ultrasound and 99 mTc-MIBI Scintigraphy With Surgical Localization According to the Variables Analyzed.
| N | Ultrasound | 99mTc-MIBI scintigraphy | |||
|---|---|---|---|---|---|
| Kappa Coefficient by Variable | Pb | Kappa Coefficient by Variable | Pb | ||
| Global | 139 | 0.387 | 0.669 | ||
| Gland weight | 138a | .065 | <.001 | ||
| >600 mg | 83 | 0.461 | 0.866 | ||
| ≤600 mg | 55 | 0.311 | 0.444 | ||
| Preoperative PTH | 139 | .072 | .277 | ||
| >174 pg/mL | 58 | 0.482 | 0.730 | ||
| ≤174 pg/mL | 81 | 0.327 | 0.628 | ||
| Previous cervical surgery | 139 | .700 | .715 | ||
| No | 131 | 0.390 | 0.673 | ||
| Yes | 8 | 0.333 | 0.600 | ||
| Preoperative calcium | 139 | .264 | .899 | ||
| ≤12 mg/dL | 123 | 0.372 | 0.666 | ||
| >12 mg/dL | 16 | 0.524 | 0.684 | ||
| Thyroid pathology | 139 | < .001 | .017 | ||
| No | 91 | 0.508 | 0.754 | ||
| Yes | 48 | 0.196 | 0.527 | ||
| Thyroid function | 139 | .726 | .591 | ||
| Normal | 109 | 0.394 | 0.682 | ||
| Altered | 30 | 0.359 | 0.620 |
The kappa index between scintigraphy localization and intraoperative findings was 0.669 (95% CI, 0.578–0.760), improving agreement and with statistically significant differences when the gland weight was greater than 600 mg and when there was no associated thyroid disease (Table 3).
DiscussionCurrently, the surgery of choice in PHPT due to adenoma is selective parathyroidectomy, provided there is correct preoperative localization. This is because 80%–90% of patients with PHPT have a solitary adenoma,22 which coincides with our series.
Ultrasound and 99mTc-MIBI scintigraphy are the most commonly used imaging tests for preoperative localization. Therefore, we have focused our analysis on these two studies.
The sensitivity of ultrasound in our study (56.7%) is at the lower end of the range described in the literature (53%–93%),1,4–8 which could be influenced by different factors. Ultrasound is an inexpensive and innocuous imaging technique, but it depends largely on the experience of the professional who performs it, which explains the wide range of sensitivities reported. In the study by Schneider et al. published in 2019, 225 out of 232 adenomas were correctly localized by ultrasound studies performed by an experienced endocrinologist or endocrine surgeon, concluding that ultrasound could be sufficient as the only imaging test in patients with PHPT when performed by an expert.23 The results were excellent due to the high experience of the professionals.
In the study we present, ultrasound scans have been performed by a large number of radiologists who are not exclusively dedicated to this pathology. This, as well as the type of ultrasound used, could influence the sensitivity obtained. However, it was not possible to analyze the latter, as 2 machines were used interchangeably throughout the period analyzed.
Apart from the technician’s experience, there are other factors that may affect the correct preoperative localization of ultrasound, which has been the objective of our study. The only independent factor that has improved the concordance of ultrasound in the multivariate analysis was the absence of accompanying thyroid disease, with an OR of 3.57 (95% CI, 1.71–7.46; p < 0.001). In the sample studied, there was a high percentage of thyroid disease (31.5%), which could have affected the low sensitivity. This finding has been described in the literature by different authors.1,6,15 Medas et al. reported thyroid disease associated with hyperparathyroidism in 44.8%, with ultrasound sensitivity decreasing from 75 to 46.7%.12 Frank et al., in a systematic review of 28 studies, concluded that the combination of ultrasound and scintigraphy presents greater sensitivity in cases of PHPT with associated thyroid disease.24 Lumachi et al. recommended combining both tests in these cases.13 Thus, when there is concomitant thyroid disease, prior to performing a selective procedure, it is essential that there be agreement between 2 image techniques and, if there is an uncertain diagnosis, bilateral cervical exploration should be performed.
The sensitivity of scintigraphy in our study (81.6%) is close to the upper limit of the published range (50%–85%).5,7–10 It can increase to 88%–90% when the pathological gland is solitary14 and be lower in cases of double adenoma. Medas et al. reported a sensitivity of 26.7% in double adenomas and hyperplasias.12
There are different factors described in the literature that may affect the sensitivity of this test, such as PTH levels below 150 pg/mL, preoperative calcium, associated thyroid disease, ectopic adenoma, gland size, etc.1,6,11–17,25 The only factor that has positively influenced the greater sensitivity of scintigraphy in the multivariate study was the gland weight greater than 600 mg, with an OR of 10.72 (95% CI, 3.39–33.84; p < 0.001). Berber et al. conducted a prospective study with 1,000 patients, reporting gland size and volume as independent factors that affected the sensitivity of ultrasound and 99mTc-MIBI scintigraphy.11 Other authors have verified this finding on scintigraphy15–17,21 and ultrasound.15 Calva-Cerqueira et al. found that 95% of adenomas that were correctly localized by scintigraphy weighed more than 250 mg, 75% more than 550 mg (PPV) and that 62% of those not localized weighed less than 550 mg.16 In the study by Stephen et al., the sensitivity of scintigraphy decreased with small adenomas, and the average weight of the TP was 1336 ± 1603 mg versus 475 ± 365 mg in the FN.21 The reason for this seems to be in the decrease or absence of 99mTc-MIBI deposition when the size of the adenoma is less than 1 cm or the weight less than 500 mg.15,17 Hence, the weight >600 mg was chosen as the cut-off point.
In the series studied, the strength of concordance between the two tests was moderate, sensitivity 78.7% and the PPV higher than reports in the literature (100% vs. 97%).2 Zheng et al. and Krausz et al. confirm the highest preoperative diagnostic accuracy when both imaging tests agree, making selective parathyroidectomy possible.1,3
When there is disagreement or lack of localization by both tests, other imaging techniques can be used, such as MRI, CT or choline PET. The latter presents high sensitivity for the localization of pathological gland(s) (96%–100%) and greater precision than ultrasound and scintigraphy.8,10,26 Good results are being obtained in the localization of small lesions, ectopic adenomas, PHPT with slightly elevated PTH or in patients with previous failed surgeries. At our hospital, we have begun to use it in cases of discordance between tests or non-localization, with initially promising results.
The limitations of this study are, first of all, that we analyzed only the laterality of the adenoma and not its exact position due to the small sample size. Secondly, 5.8% of patients with previous cervical surgery may have increased the heterogeneity of the sample and affected the results. And, lastly, we did not analyze the possible differences in accuracy of the 2 ultrasound machines that were used interchangeably throughout the study period.
With the data obtained from the study, we are able to conclude that:
- –
The sensitivity and concordance of ultrasound decrease in patients with PHPT and accompanying thyroid disease.
- –
In the case of scintigraphy, these rates decrease when the gland weight is less than 600 mg.
- –
Both tests have a high PPV.
- –
In inconclusive cases, in which there is disagreement in the localization or in the failed surgeries, other imaging techniques should be used, such as choline PET.
The authors have no conflict of interests.
Our sincere thanks to the Endocrinology Department for their involvement in the diagnosis, treatment and follow-up of these patients. We would also like to thank the Radiology, Nuclear Medicine and Pathology Departments for their involvement in the pre- and postoperative diagnoses.
Please cite this article as: Acín-Gándara D, Pereira-Pérez F, Medina-García M, Sebastián-Viana T. Factores que condicionan la sensibilidad de la ecografía y la gammagrafía en la localización del adenoma paratiroideo. Cir Esp. 2020;98:18–25.