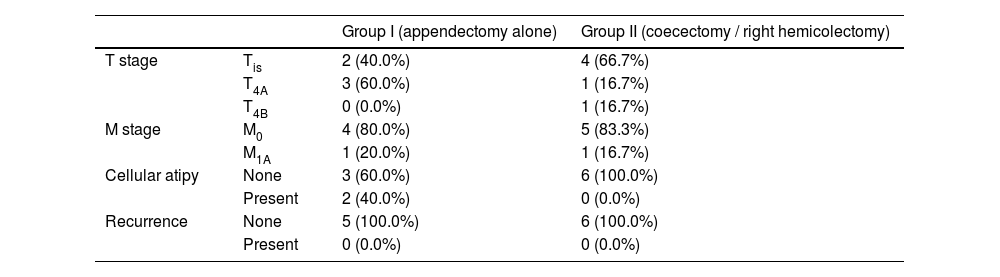
Low grade appendiceal mucinous neoplasm (LAMN) is a new entity used for a group of appendicieal mucinous tumors known as mucocele before. Recently, the consensus established by the members of the Peritoneal Surface Oncology Group International (PSOGI) Executive Committee in 2016 decided to classify epithelial mucinous neoplasms of the appendix as serrated polyps, LAMN, high grade appendiceal mucinous neoplasm and mucinous adenocarcinoma.1 Then in 2020 the consensus established by the members of PSOGI Executive Committee defined LAMN as mucinous neoplasm with low grade cytologic atypia and any of: loss of muscularis mucosa, fibrosis of submucosa, “pushing invasion” (expansile or diverticulum-like growth), dissection of acellular mucin in wall, undulating or flattened epithelial growth, rupture of appendix, mucin and/or cells outside appendix.2 By definition, all LAMN are considered grade 1 well differentiated tumors. LAMN is different from other tumors in the gastrointestinal tract because it does not have a T1 or T2 stage.2,3 Lymph node involvement is extremely rare in low grade appendiceal mucinous neoplasms.1,2 LAMNs are seen in 0.2%–0.3% of all appendectomy specimens and it constitutes less than 1% of all cancers.4 Due to the rarity of LAMNs, there is almost no established treatment guideline with controversies on the extent of surgery and the role of chemotherapy regimens. This study aimed to evaluate varying surgical approaches in localized LAMN. A retrospective database search for LAMN in our institution between June 1st, 2017 and June 1st, 2021 revealed 16 patients. 3 patients with pseudomyxoma peritonei (PMP) at the time of diagnosis and 2 patients with colon adenocarcinoma, incidentally diagnosed during the operation as LAMN were excluded from the study. Eleven patients were evaluated. Seven of 11 patients were female (63.6%) and the median age was 63 years (range: 19–71). Preoperative diagnosis was acute appendicitis in 2 patients, and in the rest, it was appendiceal tumor or right lower abdominal mass. Tumor markers (CEA and Ca 19-9) were in normal range at the initial diagnosis. Patients’ sociodemographic features like sex and age at the time of surgery, their preoperative diagnosis, their tumor marker (CEA and Ca 19-9) levels at the time of diagnosis and tumor’s pathological features like tumor size, surgical margins, existence of cellular atypia and TNM stage, events during follow-up and total follow-up time were determined. Patients were grouped as patients treated only with appendectomy (5 patients) and as patients treated with coecectomy or right hemicolectomy (CRH) (6 patients). Pathological features of the tumors in groups were given in Table 1. In pathology specimen median size of LAMN was 4.5 cm and surgical margins were free of tumor in all cases. Two patients operated initially due to acute appendicitis had perforation and acellular mucin at the right lower quadrant. One patient with perforation at the initial operation had diagnostic laparoscopy in the 6th month of follow-up. The other patient with perforation was only followed up. Median follow-up time was 25 months (4–43). Follow-up procedure consist of thoracal, abdominal and pelvic computed tomography scan and serum tumor markers scheduled after surgery, then every 6 months for 5 years, and yearly thereafter. None of the patients had recurrence. In this series, majority of the patients were female (63.6%), this is consistent with the literature.5–7 Median age was was 63 years. In the literature the patients were usually diagnosed in their 6th or 7th decades.6,7 All of the patients had normal levels of CEA and Ca 19-9 and there was no recurrence of the disease. Both PSOGI and literature suggest that normal levels of CEA, Ca 19-9 and Ca125 could be used to select patients for expectant treatment.2,4 Also none had positive surgical margins; this is also suggestive for watch and waits strategy with appendectomy only.5–7 In this series there were 5 patients with T4 tumor, 3 of them left just with appendectomy. Two patients had M1a tumor with acellular mucin in the right lower quadrant of the abdominal cavity, one left with appendectomy and the other had undergone right hemicolectomy. None had recurrence. Guaglio et al. in their study5 stated that if LAMN had been radically resected with appendectomy, even with limited peritoneal spread, it recurred unlikely; furthermore, appendix wall perforation and the presence of mucin, cells, or both outside the appendix did not carry a higher risk of metachronous peritoneal dissemination. Boshnaq et al.6 in their series also expressed that in patients with positive surgical margin or in perforated LAMN with cellular or acellular mucin on the serosal surface of the appendix or the mesoappendix, right hemicolectomy seems to offer no additional benefit over appendectomy alone. Furthermore Sueda et al.7 in their retrospective study have found that even though a majority of patients who presented with perforation did not develop PMP, tumor perforation at presentation was the unique factor significantly associated with PMP. PMP did not affect overall survival in this population but was associated with decreased disease-specific survival at 5 years. The risk for PMP after complete resection of LAMN even with limited peritoneal dissemination seems minimal, so in cases without gross pathology in coecum and/or right lower abdominal quadrant, where the tumor seems to be restricted to appendix even with perforation and mucin on the surface, the “watch and wait” strategy can be the optimal treatment of LAMN.5–9 Though we should keep in mind that the studies on LAMN has only 5-year-follow-up time.
Pathological features of the tumors in groups.
| Group I (appendectomy alone) | Group II (coecectomy / right hemicolectomy) | ||
|---|---|---|---|
| T stage | Tis | 2 (40.0%) | 4 (66.7%) |
| T4A | 3 (60.0%) | 1 (16.7%) | |
| T4B | 0 (0.0%) | 1 (16.7%) | |
| M stage | M0 | 4 (80.0%) | 5 (83.3%) |
| M1A | 1 (20.0%) | 1 (16.7%) | |
| Cellular atipy | None | 3 (60.0%) | 6 (100.0%) |
| Present | 2 (40.0%) | 0 (0.0%) | |
| Recurrence | None | 5 (100.0%) | 6 (100.0%) |
| Present | 0 (0.0%) | 0 (0.0%) |
Nil.
Conflict of interestThe authors declare that they have no conflict of interest.