Idiopathic granulomatous mastitis (IGM) is a rare benign entity (<1% of biopsies)1 of unknown etiology that is occasionally difficult to diagnose due to its similarity with other entities, such as breast cancer, or its histology, which is similar to inflammatory granulomatous diseases. Its evolution is unpredictable, and there is currently no consensus on the optimal treatment for these patients.
We present the case of a 45-year-old woman under treatment for hypothyroidism, who consulted about a supra-periareolar nodule in the right breast measuring 2cm that had been progressing over the previous month, causing spontaneous skin retraction. Axillary examination was normal. Mammography and ultrasound showed asymmetry of the retroareolar fibroglandular tissue of the right breast measuring 2.2cm×1.6cm, BI-RADS 4b, but no observed nodules or microcalcifications. In the core needle biopsy (CNB) sample, there appeared to be chronic acute inflammation with the presence of non-necrotizing abscessing granulomas and giant-cell reaction, with no signs of malignancy. In the immunohistochemistry techniques (Gram and Ziehl-Neelsen) no microorganisms were identified. In view of the clinical and histological-radiological disagreement, magnetic resonance imaging was performed, which detected asymmetry in the anterior right breast measuring 2.6cm×1.3cm that was hypointense in T1 sequences and hyperintense in STIR; after the administration of contrast, the area showed early, heterogeneous enhancement with a dynamic ascending-plateau curve.
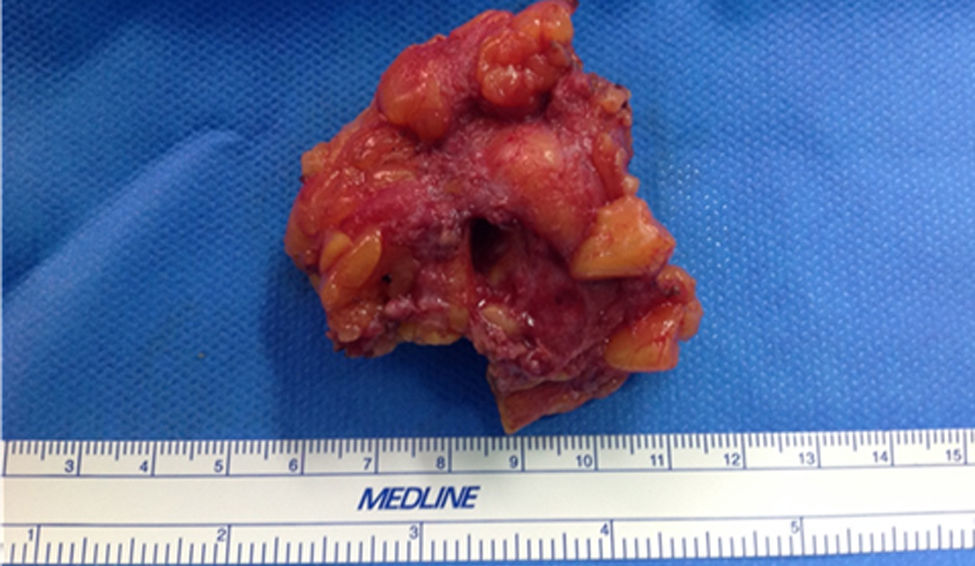
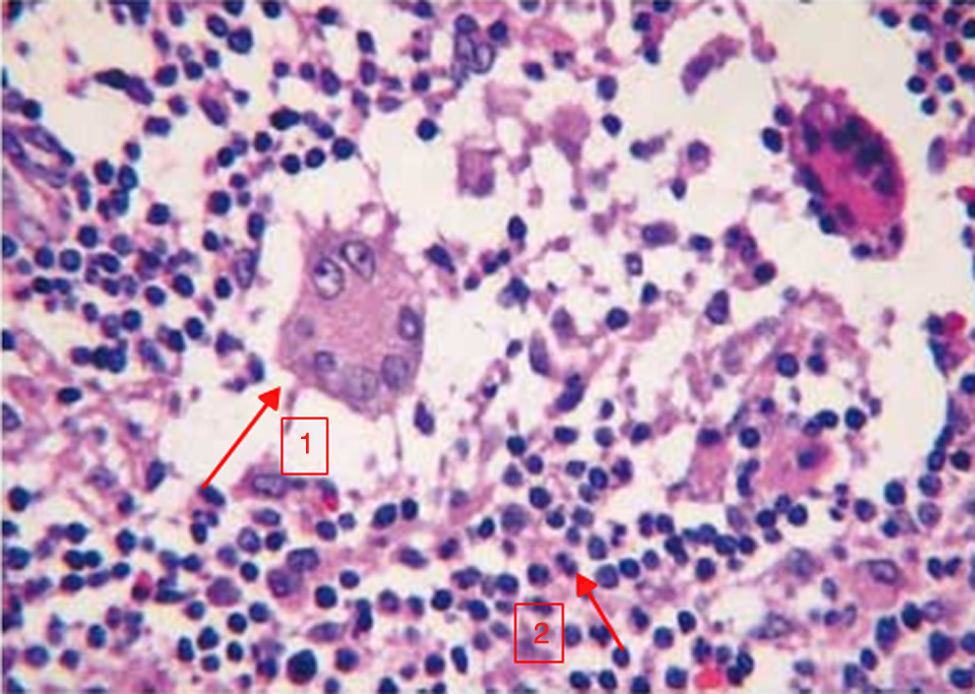
After presenting the case in committee, a surgical intervention was decided upon, involving excision of the indurated area, including a cavity with purulent content (Fig. 1). The definitive histology study reported a chronic inflammatory process with frequent accumulations of histiocytes, moderate lymphoplasmacytic inflammatory infiltrate, with formation of a central pseudocyst and moderate acute inflammation, as well as non-necrotizing granulomas with the presence of multinucleated cells, sometimes Langhans type, all of which suggested idiopathic granulomatous lobular mastitis (Fig. 2). Acid-fast bacilli were not isolated with the Ziehl-Neelsen technique, nor were fungal structures with PAS-diastase or microorganisms with the Gram technique. The patient was discharged with no disease recurrence after 3 months of follow-up.
IGM is a benign chronic inflammatory disease of the breast that was first described in 1972 by Kessler and Wolloch.2 Its clinical presentation is highly variable (mastitis, fistulas, nodules, etc.), although in 50% of reported cases, like our patient, the initial diagnosis is breast cancer.2–4 IGM appears in women of childbearing age (<50 years in most cases described) with recent pregnancies (1.5–5 years).3–6 The presentation is usually one-sided, with one or more periareolar mammary masses, sometimes with cutaneous inflammation that can lead to abscess, fistula or chronic suppuration.5,6 Its etiology is unknown, although several theories have been postulated: (1) autoimmune, given the similarities with thyroiditis and granulomatous orchitis. This theory is supported by the good response to steroid therapy, however, there is no evidence of abnormalities of the immune system, such as antibody formation or antigen-antibody complexes; (2) local immune response, probably due to damage to the lobular epithelium secondary to trauma, chemical irritants or infection, which would allow luminal secretions to escape toward the lobular connective tissue, causing a granulomatous reaction with migration of lymphocytes and macrophages; (3) hormonal causes, considering the increasing incidence of this condition in women with oral contraceptives (33% of patients); and (4) associated with erythema nodosum, lupus or the existence of a still unidentified infectious organism.1,5–9
Given its clinical and radiological similarity with breast cancer, the diagnosis is mainly histopathological and by ruling out other diseases, finding a granulomatous inflammatory reaction, giant multinucleated Langhans cells and lymphocytes in the lobules.8–10 Occasionally, fat necrosis is observed with accumulation of polymorphonuclear cells, forming abscesses that can lead to fibrosis with distortion of the lobe architecture, producing atrophy and degeneration of the epithelium, as well as dilation of the mammary ducts. Other unusual findings include squamous metaplasia of the mammary ducts and large abscesses. Stains and cultures for bacteria, fungi, and acid-fast organisms are typically negative. The main differential diagnosis is breast cancer and, after CNB, granulomatous diseases (breast tuberculosis, sarcoidosis, cat scratch disease, granulomatous reaction, fat necrosis, duct ectasia, acute mastitis, Wegener's granulomatosis, Taenia solium infection, Salmonella typhi, Histoplasma capsulatum and Wuchereria bancrofti).3,8,9
The treatment of choice for IGM has not yet been established and its tendency toward local recurrence must be considered (38%–50% cases).5,6 Thus, and according to reported cases, its management varies from conservative treatment with corticosteroids (Prednisone® 60mg daily) to surgical treatment, either with surgical excision or with mastectomy according to the size of the lesion, and complete resection is recommended. Due to secondary reactions to steroids and frequent recurrence after their reduction and suspension, methotrexate or azathioprine are used for their steroid-sparing capacity, thereby maintain the remission of the mastitis.6–10
In conclusion, IGM is a benign entity that is uncommon, and its differential diagnosis is made mainly with breast cancer.
Please cite this article as: Marín Hernández C, Piñero Madrona A, Gil Vázquez PJ, Galindo Fernández PJ, Parrilla Paricio P. Mastitis granulomatosa idiopática. Una rara entidad benigna que puede simular un cáncer de mama. Cir Esp. 2018;96:177–178.