Parathyroid adenomas are benign tumors that produce parathyroid hormone. Their incidence is around 20 cases/100000 inhabitants/year. Approximately 90% are sporadic and present as a single adenoma, while the remainder usually have a polyglandular presentation and are associated with hereditary polyglandular endocrine diseases. The parathyroid glands originate from the third and fourth pharyngeal arches and descend along with the rest of the cervical structures during embryogenesis to be later located in various positions between the superior mediastinum and cervical region, as well as between the fibers of the vagus nerve.1 During a review of the literature, only 17 other cases of intravagal adenoma have been found.2–7 We present a new case.
The patient is a 41-year-old man with no history of interest who, for several years, has had self-limiting episodes of generalized abdominal pain that have lasted several days. Within the initial diagnostic tests, calcium levels were studied (14.2mg/dL), and the patient was subsequently diagnosed with primary hyperparathyroidism with no renal or articular involvement. The examination showed no pathological findings except for a tumor measuring approximately 2cm, not adhered to neighboring structures, in the left cervical area III. Ultrasound reported the same nodule to be hypoechoic, with abundant internal vascularization. The sample from the fine-needle aspiration was nonspecific. The scintigraphy with sestamibi identified the mass as an ectopic parathyroid adenoma. No preoperative laryngoscopy was requested.
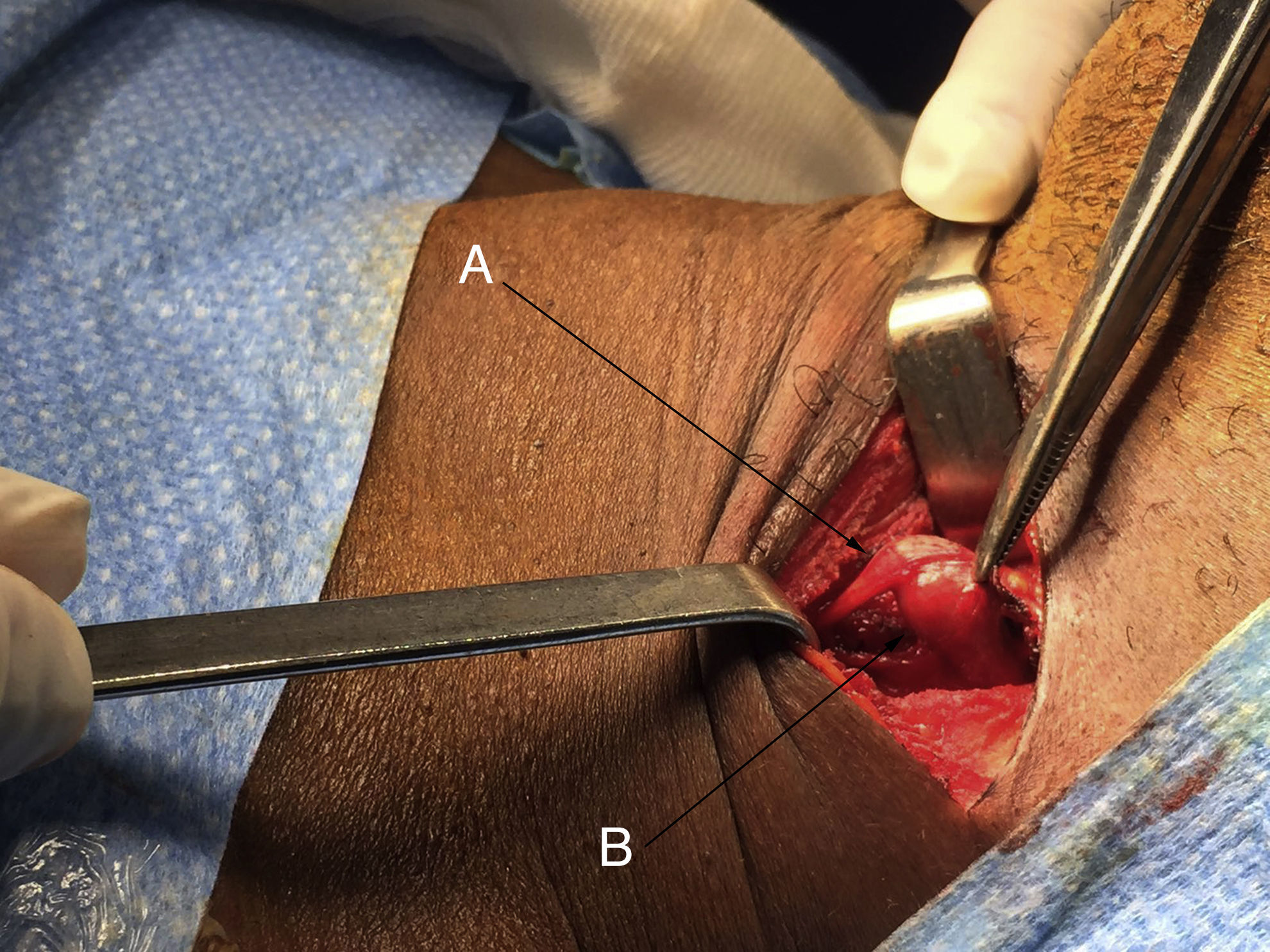
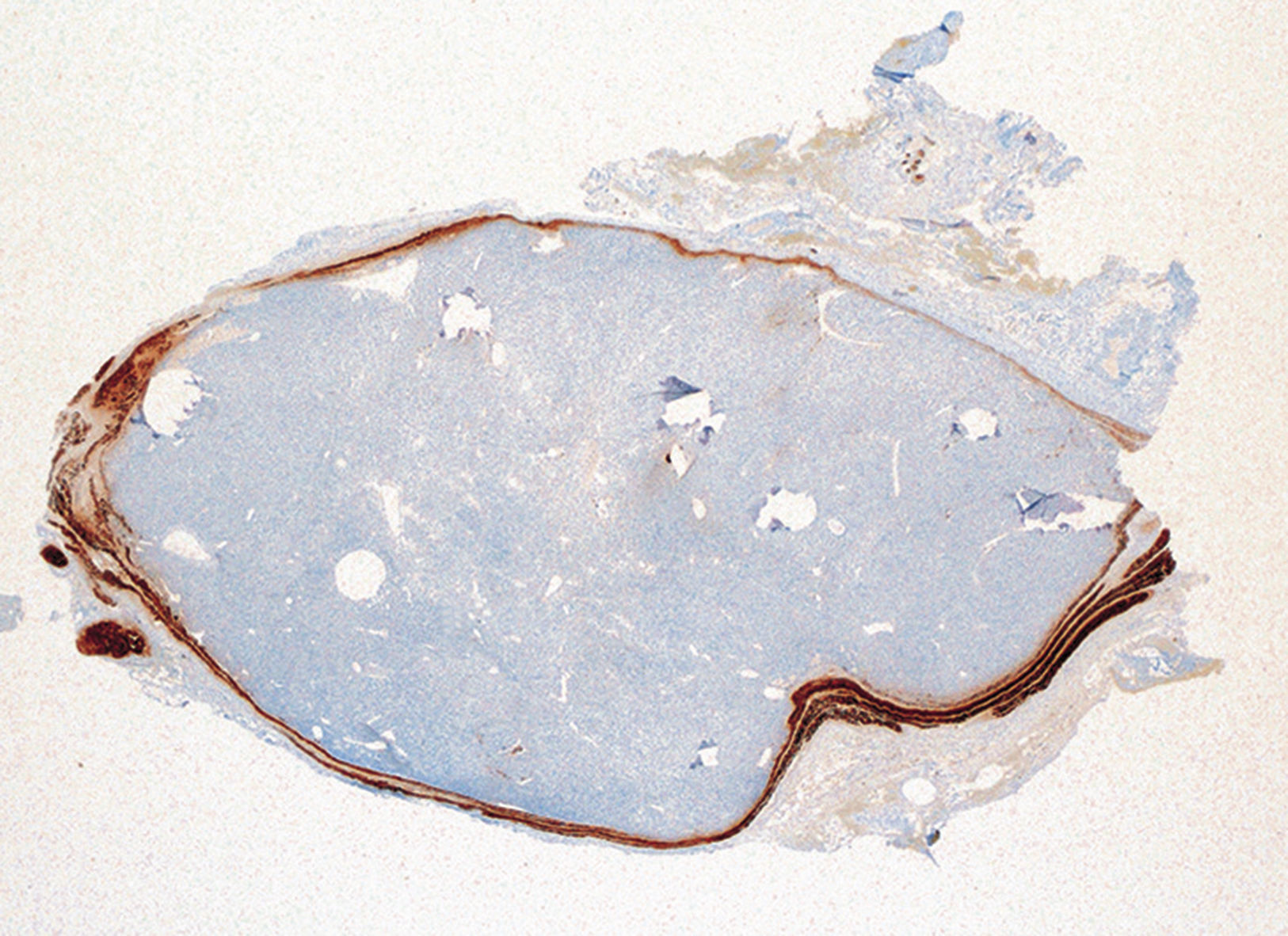
Surgery was performed with a direct approach in cervical region II–III, and a tumor was identified in the left vagus nerve, below the bifurcation of the carotid artery (Fig. 1). The vagus nerve ran along its craniocaudal axis, emitting a weak, positive, intermittent signal with neural stimulation. Enucleation of the mass and preservation of the vagus nerve was not possible, so the tumor was resected, which provided an intraoperative pathological result compatible with parathyroid adenoma. The definitive pathology report described a parathyroid adenoma (0.94g) surrounded by neural tissue (Fig. 2). The patient was discharged on a short-stay surgery regimen with a calcium level of 10.5mg/dL and an iPTH level of 9.2pg/dL, showing left recurrent paralysis from the immediate postoperative period.
Currently, after a follow-up of one year and 2 months, the patient presents calcium and parathyroid hormone levels within normal limits. In spite of the improvement after rehabilitation, he continues to have dysphonia and phonasthenia at the end of the day (GRBAS scale 2-0-2-3-0). As mentioned above, the parathyroid glands originate from the third and fourth pharyngeal arches, descending to the dorsal region of the thyroid during the sixth week of embryogenesis.1 Some 6%–22% of the time, these glands are not located in said region, forming ectopic glands. Approximately 60% of the ectopic glands are dependent on the inferior parathyroid glands and 40% on the superior glands.7–9 This is possibly due to the fact that the pathway covered by the inferior glands is longer than the superior. In this manner, the ectopic inferior parathyroid glands can be located in the thymus, anterior mediastinum, thyroid parenchyma, thyrothymic ligament or submandibular region. The superiors glands are usually in the tracheoesophageal sulcus, retroesophagus or posterior mediastinum. There is also the possibility of forming supernumerary glands, a feature that has been described in 13% of the population. The presentation of a supernumerary gland increases the probability that its location is ectopic.9
Thus, given the great embryological variability of the parathyroid tissue, although unusual, it is not impossible for parathyroid glands to form inside the vagus nerve. This may be due to the fact that the endoderm of the branchial arches and the neural ectoderm have a common locoregional origin.1 In this context, a series of autopsies carried out on 32 infants under the age of one identified intravagal parathyroid tissue in up to 4 (6%) out of the 64 nerves.10
To date, only 17 cases of intravagal parathyroid gland have been published in the English and French literature.2–7 A part of the cases were supernumerary glands and presented as persistent or recurrent primary hyperparathyroidism. In 12 of them, enucleation was achieved with no nerve injury. The surgical approach varied markedly, and in the last 2 cases a direct approach was used, as in ours case and unlike previous ones. Advances in imaging techniques have improved the preoperative identification of the lesions causing hyperparathyroidism. The direct approach is indicated in these cases, which avoids to a great extent the complications associated with the classic approach.
In conclusion, although it is exceptional, it is possible to identify a parathyroid adenoma in an intravagal location, especially in those cases of persistent or recurrent hyperparathyroidism with imaging tests that identify a suspicious tumor in this location. In these cases, the direct approach must be prioritized and enucleation must be done whenever technically feasible.
Thanks to the General Surgery Teaching Unit at the Hospital de Galdakao-Usansolo for their collaboration, including Dr. Salvador Mateo, Dr. Igor Alberdi and Dr. Marta Calvo.
Please cite this article as: de Andres Olabarria U, Martínez Roldán A, Basáñez Amuchastegui A, del Pozo Andrés E, Ibáñez Aguirre FJ. Adenoma paratiroideo intravagal con cirugía de abordaje directo. Cir Esp. 2018;96:175–176.