SARS-CoV-2 pandemic has caused an important impact in our country and elective surgery has been postponed in most cases. There is not known information about the decreasing and impact on surgery. Mortality of surgical patients with SARS-CoV-2 infection is estimated to be around 20%.
MethodsWe conducted prospective data recruitment of people inpatient in our Digestive and General Surgery section of Girona's University Hospital Dr. Josep Trueta from 03/14 to 05/11. Our objective is to analyze the impact that SARS-CoV-2 pandemic over elective and urgent surgery.
ResultsDuring the peak occupation of our center Intensive Care Unit (303.8%) there was a reduction on elective (93.8%) and urgent (72.7%) surgery. Mortality of patients with SARS-CoV-2 infection who underwent surgery (n=10) is estimated to be a 10%. An 80% of these patients suffer complications (sever complications in 30%).
ConclusionsThe actual study shows a global reduction of the surgical activity (elective and urgent) during de SARS-CoV-2 pandemic. Global mortality of patients with SARS-CoV-2 infection are low, but the severe complications have been over the usual.
La pandemia por SARS-CoV-2 ha causado un importante impacto en nuestro medio, con la necesidad de demorar la cirugía programada y urgente. Las cifras referentes a la disminución de la actividad quirúrgica y el impacto del periodo aún no se conocen con exactitud. Se estima una mortalidad de hasta un 20% en los pacientes operados con infección peroperatoria por SARS-CoV-2.
MétodosDel 14/03 al 11/05 del 2020 se han recogido los datos de los pacientes ingresados en el servicio de Cirugía General y Digestiva del Hospital Universitari Dr. Josep Trueta de Girona, para analizar el impacto de la pandemia sobre la cirugía electiva y urgente.
ResultadosDurante el periodo de ocupación pico de la Unidad de Medicina Intensiva de nuestro centro (con un máximo de 303,8%), la cirugía electiva y la urgente se redujeron un 93,8% y un 72,7%, respectivamente. La mortalidad de los pacientes operados con infección por SARS-CoV-2 en nuestro estudio (n=10) fue del 10%; las complicaciones fueron del 80% (siendo graves un 30%).
ConclusionesEl presente estudio muestra una reducción global de la actividad quirúrgica tanto electiva como urgente durante la pandemia. La mortalidad global de los pacientes operados con infección por SARS-CoV-2 ha sido baja, pero la tasa de complicaciones graves ha sido superior a la global.
Since the start of the global pandemic declared by the World Health Organization (WHO) on March 11, 2020,1 the global outbreak of SARS-CoV-2 has resulted in multiple healthcare consequences in our setting. In the case of Spain, 231765 cases had been diagnosed by May 11, 2020, with 88707 hospitalizations and 18352 deaths, making us one of the countries with the greatest initial impact, following in the wake of China and Italy.2
In the case of General and Digestive Surgery (GDS), little information is available about the consequences of perioperative infection in patients, and there is very limited evidence due to the small number of articles and patients collected in these. Reported data show a high rate of associated mortality.3 The most affected patients have been older (over the age of 60), with comorbidities such as hypertension, diabetes mellitus, obesity, malnutrition, adrenal insufficiency, cardiovascular disease, active cancer and chronic obstructive pulmonary disease (COPD).4–9
The lockdown officially began on March 14 in Spain.10 From that moment on, the number of scheduled surgeries was reduced, following the recommendations of different surgical societies. The Hospital Universitari Dr. Josep Trueta de Girona (HJT) is a public tertiary referral hospital for a population of more than 800000 inhabitants, in which elective surgery was almost completely canceled starting March 21. The guidelines established for the management of patients in need of elective surgery conclude with general recommendation to avoid non-delayable surgeries.11–15 The recommendations were based on two pillars: the high mortality of surgical patients with perioperative SARS-CoV-2 infection (up to 20% according to Chinese series3) and the need to reorganize efforts toward the high demand for medical care caused by SARS-CoV-2.11
Finally, there is the subjective impression that the volume of surgical emergencies dropped, and that there was less surgical activity. Even so, no studies have been published in this regard. Other specialties have indicated a decrease in emergencies treated in the hospital, together with an increase in complications and associated morbidity and mortality rates.16 In order to answer this question, we have prospectively collected data from patients operated on during the different phases of the SARS-CoV-2 pandemic with the aim to help us improve how we face possible similar events in the future.
MethodsWe prospectively collected the data of patients admitted to the GDS service of the HJT from February to May 2020.
Data were collected on the number of scheduled and urgent surgeries, surgeries in patients infected by SARS-CoV-2, as well as patients with normally surgical pathologies who were treated conservatively. As a reference, data have been taken from the 4-week period prior to the national emergency situation.
All the patients underwent PCR testing with a nasal swab sample.
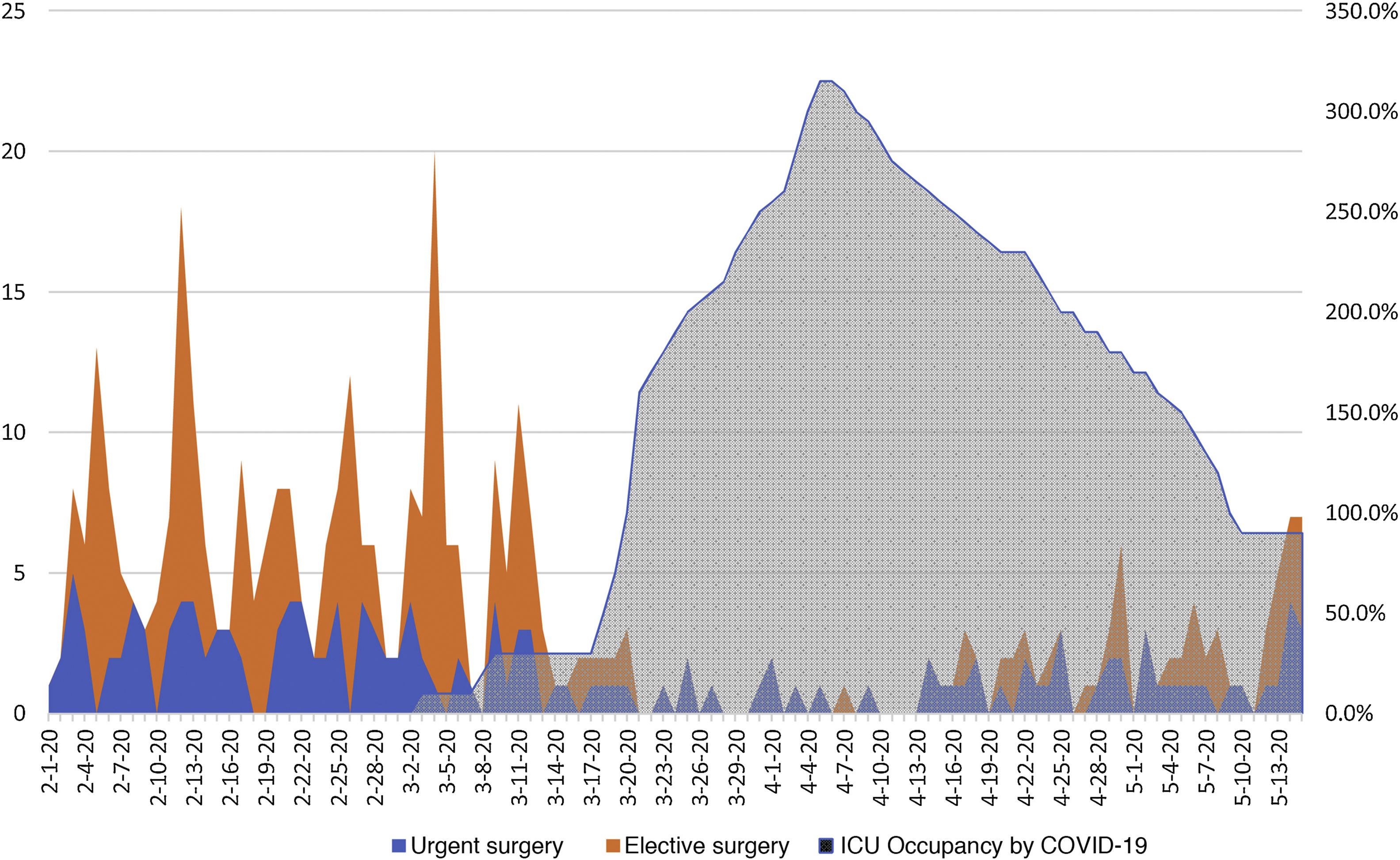
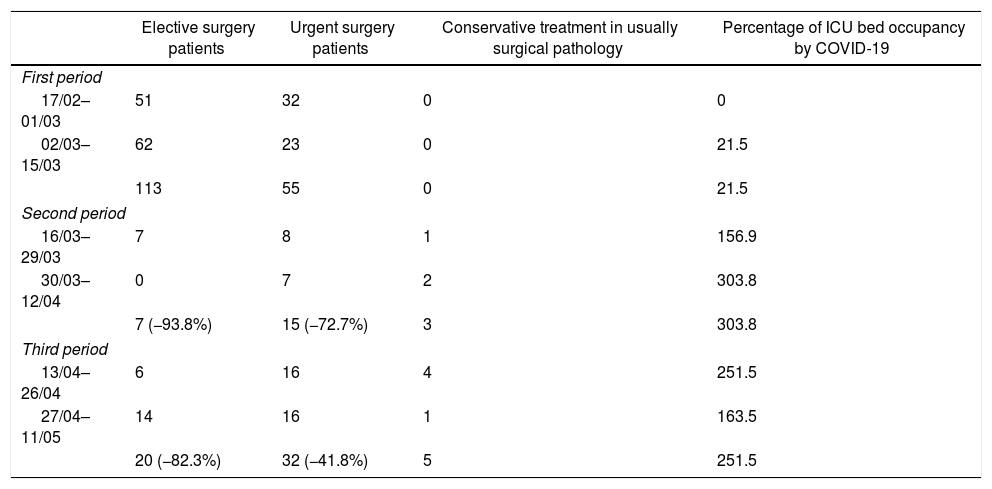
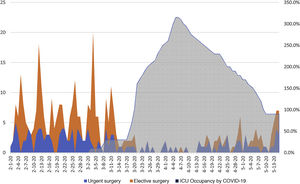
The main objective of the study was to evaluate the evolution of scheduled and urgent surgeries in the period between March 14 and May 11, 2020.17 To establish a reference pattern, data was collected from patients who had undergone surgery starting on February 1, 2020. Three periods were defined to facilitate the reporting of results and their analysis: the first period (02/17–03/15) represents the pre-lockdown status; the second (03/16–04/12) represents the period of maximum occupancy by patients with SARS-CoV-2 infection in the Intensive Care Unit (ICU); and the third (04/13–05/11) is the period of decline in ICU occupancy prior to the start of deconfinement.
The secondary objective of the study is to analyze the survival, morbidity and mortality rates of patients who had been admitted and/or operated on by the GDS service of our hospital during the previously described period.
Data were analyzed with Microsoft Excel® (v19.0) (Microsoft, Washington, USA). We calculated the mean percentage of critical care beds occupied by patients with SARS-CoV-2 infection and its increase for each period compared to the pre-lockdown period, with a baseline number of beds of 20. Data for age, sex, and comorbidities were obtained with the Charlson Comorbidity Index18 (CCI) and complications using Clavien–Dindo19 during the immediate postoperative period, including 15-day mortality. Median CCI and age were calculated for each subgroup of patients. The remaining data are provided in absolute numbers and as a percentage of the total.
ResultsAnalysis by periodsDuring the pre-alarm period, 113 patients underwent elective surgery and 55 patients had urgent surgery (Table 1). No patient with SARS-CoV-2 infection was operated on or infected during their hospital stay. The maximum occupancy percentage of the ICU by patients with SARS-CoV-2 infection in this period was 21.5% (mean occupancy for the first half of March).
Distribution of the number of patients and ICU bed occupancy rate by patients with SARS-CoV-2 infection.
| Elective surgery patients | Urgent surgery patients | Conservative treatment in usually surgical pathology | Percentage of ICU bed occupancy by COVID-19 | |
|---|---|---|---|---|
| First period | ||||
| 17/02–01/03 | 51 | 32 | 0 | 0 |
| 02/03–15/03 | 62 | 23 | 0 | 21.5 |
| 113 | 55 | 0 | 21.5 | |
| Second period | ||||
| 16/03–29/03 | 7 | 8 | 1 | 156.9 |
| 30/03–12/04 | 0 | 7 | 2 | 303.8 |
| 7 (−93.8%) | 15 (−72.7%) | 3 | 303.8 | |
| Third period | ||||
| 13/04–26/04 | 6 | 16 | 4 | 251.5 |
| 27/04–11/05 | 14 | 16 | 1 | 163.5 |
| 20 (−82.3%) | 32 (−41.8%) | 5 | 251.5 | |
The percentages in parentheses represent the decrease versus the first period.
In contrast with these data, during the second period, the ICU of our center experienced its peak occupancy, with a maximum of 303.8% (mean at the end of March and the first half of April) (Fig. 1); elective and urgent surgery were dropped to 7 and 15 patients treated, respectively. Three patients were operated on with a confirmed preoperative diagnosis of SARS-CoV-2 infection.
In the third period, the ICU bed occupancy rate decreased to 163.5%. Although a normal surgical situation had not been restored, the number of electively operated patients increased to just 20 (less than one a day). The urgent surgery performed exceeded twice the previous period (32 patients), as well as the number of patients operated on with SARS-CoV-2 infection reaching its maximum (7 patients).
During the first period, there were no patients with surgical pathology treated conservatively. During the second period, 3 were treated conservatively, and in the third period, 5. Most of these patients were diagnosed with acute cholecystitis (n=5), all of whom were treated with antibiotic therapy, with or without cholecystectomy. The rest were occlusive colon carcinomas (n=4) and acute appendicitis (n=1), which were treated with colon stents as a bridge to surgery and antibiotic therapy, respectively. One of the patients died of biliary sepsis; the rest progressed favorably.
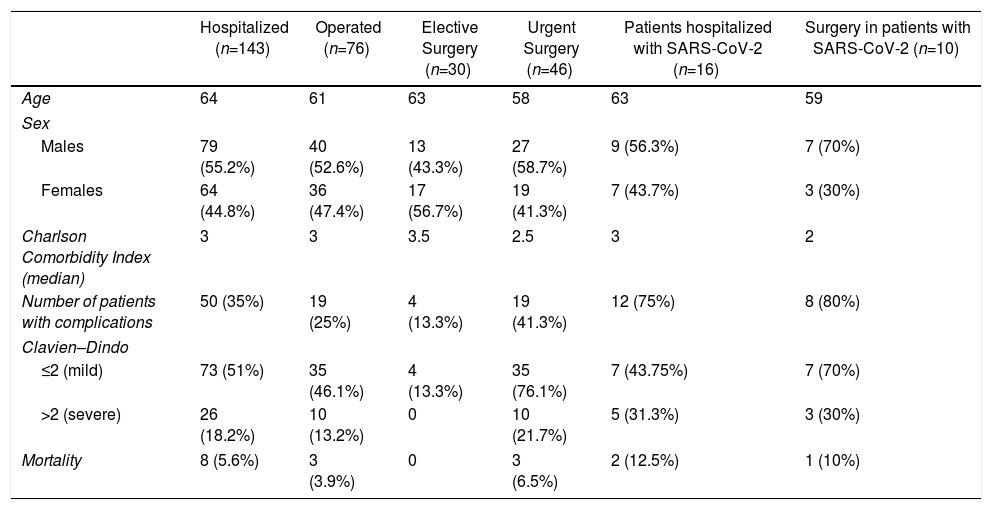
Analysis of patient characteristicsDuring the previously defined period, 143 patients were admitted to our GDS service (Table 2); 55.2% were men, 44.8% were women, and the median age was 64 years. The median CCI was 3 points. In total, 50 patients (35%) presented some type of complication during their stay, while 18.2% were serious (Clavien–Dindo>2). The general mortality rate of the period was 5.6%.
Analysis of the different categories collected prospectively according to the treatment subgroups and infection or not by SARS-CoV-2.
| Hospitalized (n=143) | Operated (n=76) | Elective Surgery (n=30) | Urgent Surgery (n=46) | Patients hospitalized with SARS-CoV-2 (n=16) | Surgery in patients with SARS-CoV-2 (n=10) | |
|---|---|---|---|---|---|---|
| Age | 64 | 61 | 63 | 58 | 63 | 59 |
| Sex | ||||||
| Males | 79 (55.2%) | 40 (52.6%) | 13 (43.3%) | 27 (58.7%) | 9 (56.3%) | 7 (70%) |
| Females | 64 (44.8%) | 36 (47.4%) | 17 (56.7%) | 19 (41.3%) | 7 (43.7%) | 3 (30%) |
| Charlson Comorbidity Index (median) | 3 | 3 | 3.5 | 2.5 | 3 | 2 |
| Number of patients with complications | 50 (35%) | 19 (25%) | 4 (13.3%) | 19 (41.3%) | 12 (75%) | 8 (80%) |
| Clavien–Dindo | ||||||
| ≤2 (mild) | 73 (51%) | 35 (46.1%) | 4 (13.3%) | 35 (76.1%) | 7 (43.75%) | 7 (70%) |
| >2 (severe) | 26 (18.2%) | 10 (13.2%) | 0 | 10 (21.7%) | 5 (31.3%) | 3 (30%) |
| Mortality | 8 (5.6%) | 3 (3.9%) | 0 | 3 (6.5%) | 2 (12.5%) | 1 (10%) |
The patients who underwent elective surgery had a higher burden of comorbidities (median CCI 3.5 points). However, this did not translate into a higher percentage of postoperative complications compared to other groups, as only 13.3% of patients had some type of complication, all of which were mild (Clavien–Dindo≤2). Patients who underwent urgent surgery, especially in the subgroup of operated COVID-19 patients, had the lowest CCI (n=2). None of the patients requiring elective surgery died.
The patients with the highest percentage of complications had confirmed SARS-CoV-2 infection. This rate was higher in the subgroup of operated patients (80%), and 30% experienced serious complications (most requiring intensive care). The relative mortality rate of the surgical group with SARS-CoV-2 infection was 10%, while, the rate of the total of patients admitted with SARS-CoV-2 infection was 12.5%.
The surgical procedures performed and diagnoses in patients with SARS-CoV-2 infection were: laparoscopic appendectomy for acute appendicitis (n=2), adhesiolysis without intestinal resection due to intestinal obstruction (n=2), right hemicolectomy with mucous fistula due to ischemia of the right colon (n=2), suture of perforated duodenal ulcer (n=1), diverting colostomy due to abscessed rectal neoplasm (n=1), drainage of intra-abdominal collection (n=1), and acute post-pancreatitis drainage (n=1).
Out of the total number of patients treated surgically (n=76), SARS-CoV-2 infection was diagnosed after surgery in 5 (6.8%). In 24%, no COVID-19 test was performed (the 18 patients underwent surgery in the first period). In 5 patients, the result of SARS-CoV-2 infection was known prior to surgery (urgent surgery that could not be postponed). In the remaining patients (62.8%), the negative result was known prior to surgery. Out of the total number of patients admitted to our unit with infection, in 4 it was diagnosed 15 days after admission, so we assume a nosocomial infection rate of 2.8%.
At our hospital, 167 patients were admitted to the ICU during the study period, 1.8% of whom required surgery. Two cases required right hemicolectomy with a mucous fistula due to colon ischemia, and in one of the cases associated cholecystectomy due to gallbladder ischemia. In the remaining case, the patient had acute pancreatitis requiring surgical drainage due to poor evolution, after which he died (mortality rate of 33.3% in patients admitted to the ICU with gastrointestinal surgery).
DiscussionThe global pandemic caused by SARS-CoV-2 has been an international public healthcare emergency,1 and the countries most affected in the initial phase were China, Italy and Spain.2 By the end of May 2020, more than 235000 cases had been confirmed in Spain, 150000 patients had recovered, and nearly 29000 had died.
Given the emergency situation and hospital collapse, several international societies recommended delaying avoidable surgery, both oncological and urgent.14,15 In the latter case, antibiotic treatment was recommended in the case of patients with SARS-CoV-2 infection and diseases that are usually managed surgically, such as appendicitis or acute cholecystitis.13 In our hospital, we have observed an increase in the number of acute cholecystitis, appendicitis and occlusive neoplasms managed with conservative treatment.
The motivation behind these recommendations was the need to allocate human and technical resources to the most necessary areas, as well as the possible discontinued support of patients requiring lengthy ICU stay or prolonged resuscitation. Articles have also been published describing high mortality and complications in patients operated on during the pandemic, especially in the subgroup of those affected by SARS-CoV-2.3
Lei et al.3 reported a 20.6% mortality rate in surgical patients operated on with perioperative SARS-CoV-2 infection. This article was the first published and had the greatest number of patients operated on with COVID-19, analyzing their morbidity and mortality. The patients included were treated for several different conditions. Twelve patients had undergone surgery for digestive pathology, and some were surgeries involving high morbidity and mortality, such as pancreatic or esophageal surgery. In our study, 10 patients underwent surgery with SARS-CoV-2 infection, resulting in a mortality rate of 10%; the mortality of this group was higher than that of patients undergoing elective surgery during the same period (0%) and also higher than the mortality rate in urgent surgery (6.5%). Although the mortality rate in our series was not as high as recent published series, we should point out the high percentage of postoperative complications for our setting, including 30% serious complications, most of these being a prolonged ICU stay.
In our hospital, we have been able to verify the extraordinary gravity of the situation, starting with about 20 critical care beds in the ICU to an increase of more than 300% during the maximum peak of patients affected by SARS-CoV-2. This increase was accompanied by a 93.8% decrease in elective surgery, going from 113 elective surgeries in the 4-week period prior to confinement to 7 surgeries performed the following 4 weeks. Di Martino et al.20 published a similar decrease in scheduled surgery during the peak incidence of the SARS-CoV-2 pandemic.
Italian cardiologists noted a decrease in cardiac arrests treated in hospitals.16 To the date of our review, few articles describe a decrease in urgent and elective surgical pathology attended by the GDS services.
According to the data from our series, urgent surgery dropped by 72.7%. The decrease from 55 urgent surgeries to 15 could be explained by several reasons: symptomatic patients did not go to hospitals for fear of infection and being aware of the situation of healthcare collapse; the reduction of elective surgery and consequently of urgent surgery derived from complications; and, finally, the increase in conservative management of certain pathologies whose usual treatment is surgery.
Our study has several limitations, such as the small sample size of patients with SARS-CoV-2 infection, the limited follow-up period of the patients, and the descriptive nature of the study. It would be interesting to analyze of multicenter registries, such as the national AEC COVID-19 study, of patients undergoing surgical procedures during the SARS-CoV-2 pandemic. This registry, promoted by the AEC-COVID-19 Surgery Group of the Asociación Española de Cirujanos (AEC) will help standardize the data and help better understand the impact of the pandemic on surgical practice.
We want to highlight the collection of the total number of patients operated on in our hospital during the period from February to May, which allows us to describe the evolution of urgent and elective surgeries during pre-lockdown, the peak activity in the ICU, and the subsequent recovery, adding information to what is known so far.20 We must also highlight that, although it is limited to one study center, the reference population of our hospital is more than 800000 people. Furthermore, the patients included belonged to the GDS service; the study does not include patients treated by different specialties, as in larger well-known series.21
In conclusion, our study has tried to show the impact of the SARS-CoV-2 pandemic in two ways:
- -
There was a significant drop in elective and urgent surgery of more than 70% overall.
- -
The scheduled, elective surgery performed during the period did not seem to have greater morbidity or mortality, except in the group of positive COVID-19 patients. In these patients, serious complications and the mortality rate increased, although without reaching the numbers published in international series.
Based on this and on the low mortality rate of less complexity surgeries, we believe that, as long as the situation of hospital collapse allows, surgery that poses a low risk of needing intensive care should not be delayed.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Maldonado-Marcos E, Caula-Freixa C, Planellas-Giné P, Rodríguez-Hermosa JI, López-Ben S, Delisau-Puig O, et al. Estudio del impacto de la pandemia por SARS-CoV-2 en la práctica quirúrgica urgente y electiva en un hospital de tercer nivel. Cir Esp. 2021;99:368–373.