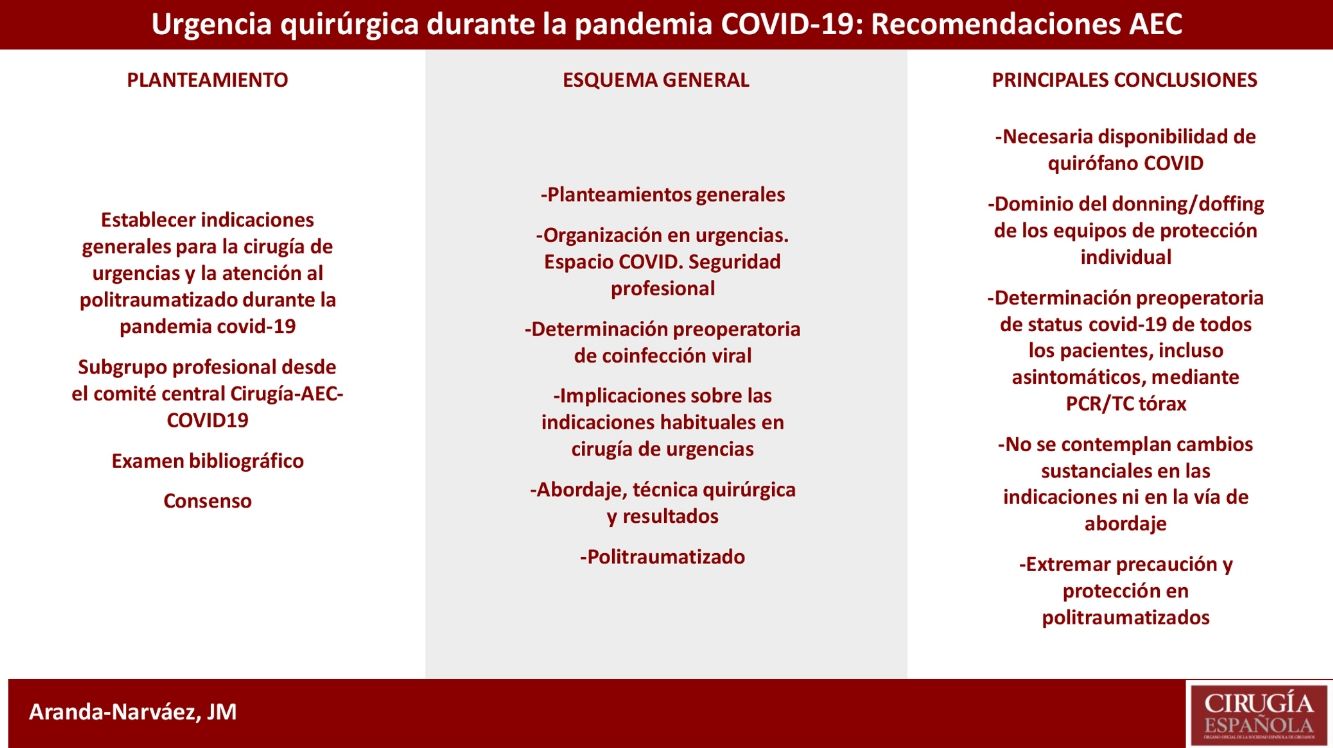
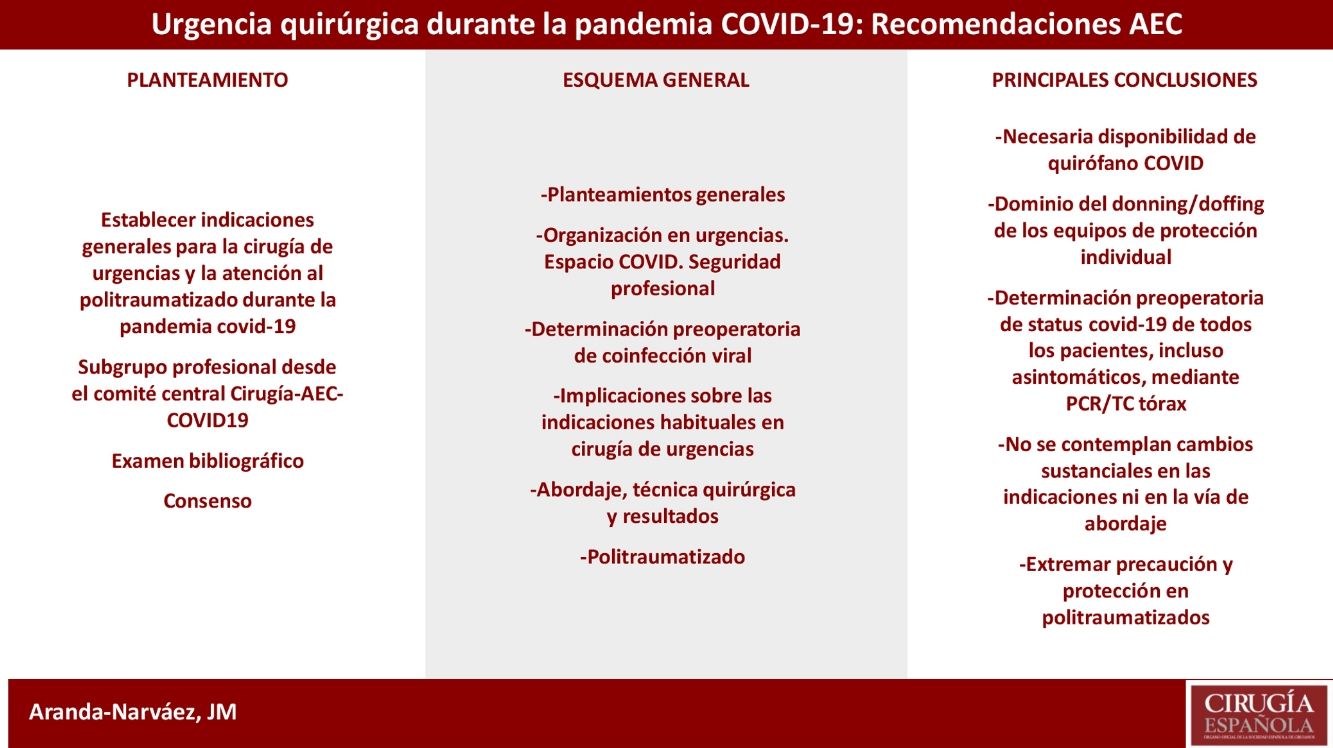
New coronavirus SARS-CoV-2 infection (coronavirus disease 2019 [COVID-19]) has determined the necessity of reorganization in many centers all over the world. Spain, as an epicenter of the disease, has been forced to assume health policy changes in all the territory. However, and from the beginning of the pandemic, every center attending surgical urgencies had to guarantee the continuous coverage adopting correct measures to maintain the excellence of quality of care. This document resumes general guidelines for emergency surgery and trauma care, obtained from the available bibliography and evaluated by a subgroup of professionals designated from the general group of investigators Cirugía-AEC-COVID-19 from the Spanish Association of Surgeons, directed to minimize professional exposure, to contemplate pandemic implications over different urgent perioperative scenarios and to adjust decision making to the occupational pressure caused by COVID-19 patients.
La infección por el nuevo coronavirus SARS-COV-2 (enfermedad por coronavirus 2019 [COVID-19]) ha determinado la necesidad de la reorganización de muchos centros hospitalarios en el mundo. España, como uno de los epicentros de la enfermedad, ha debido asumir cambios en la práctica totalidad de su territorio. Sin embargo, y desde el inicio de la pandemia, en todos los centros que atienden urgencias quirúrgicas ha sido necesario el mantenimiento de su cobertura, aunque igualmente ha sido inevitable introducir directrices especiales de ajuste al nuevo escenario que permitan el mantenimiento de la excelencia en la calidad asistencial. Este documento desarrolla una serie de indicaciones generales para la cirugía de urgencias y la atención al politraumatizado desarrolladas desde la literatura disponible y consensuadas por un subgrupo de profesionales desde el grupo general Cirugía-AEC-COVID-19. Estas medidas van encaminadas a contemplar un riguroso control de la exposición en pacientes y profesionales, a tener en cuenta las implicaciones de la pandemia sobre diferentes escenarios perioperatorios relacionados con la urgencia y a una adaptación ajustada a la situación del centro en relación con la atención a pacientes infectados.
The coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 has had a colossal impact on health systems around the world. Four months after the start of the pandemic, the total number of confirmed cases in the world is close to 2 500 000 and exceeds the figure of 170 000 deaths directly attributed to the disease. In Spain, the number of infected individuals exceeds 200 000, with a mortality rate higher than 10% and a heterogeneous impact on different regions.1 It is possible that these data have been underestimated, to a greater or lesser degree, as a direct result of the different policies adopted in different territories in terms of population screening or mortality data based solely on reliable verification of the virus. Regardless, these data reflect a health crisis with global implications.
Given the spread of this pathology, several hospitals have had to reorganize their spaces, systems and even their staff to provide an adequate response, and longer or shorter decision-making times have been determined by the speed of disease progression in the local community. However, even from the beginning of the pandemic, emergency surgeries, with their volume and treatment impact, had to be continued and were prioritized at all hospitals, regardless of the alert scenario.
In order to establish guidelines that would allow surgeons to base actions on guidelines developed and supported by a central organization, the Spanish Association of Surgeons (AEC) created the Surgery-AEC-COVID-19 Group, whose function covers different aspects of the pandemic that influence the activity of surgeons. After an exhaustive bibliographic review, the Group issued consensus recommendations, which were not able to surpass the level of evidence of expert opinion. Due to the importance of maintaining appropriate management policies for urgent surgical pathologies using the same working methodology, a parallel group of professionals has developed the specific document below, which is summarized on the Association’s website.2,3
General thoughtsCoronaviruses are viruses with an RNA genome capable of synthesizing about twenty proteins, including one that projects like a crown around its surface, giving them their name. Since the last century, these viruses have been known to cause mild respiratory infections. However, in 2002 in China (SARS-CoV coronavirus) and in 2012 in Saudi Arabia (MERS-CoV coronavirus), we witnessed two serious epidemics that caused approximately two thousand deaths.4 Although SARS-CoV-2 is of animal origin, no coronavirus identical to the one that is causing the global epidemic of 2020 has been identified in any species. Certain bats have similar viruses, but there is no solid evidence about the origin of the COVID-19 disease in humans. Transmission appears to be by person-to-person aerosols, where it can remain for hours, and it has also demonstrated stability for days when deposited on surfaces. The virus is sensitive to ultraviolet rays and heat, becoming inactivated at 56 °C for 30 min. It also appears to be inactivated with lipid solvents, ethanol, and chlorine disinfectants. Fecal-oral, urine and blood transmission also seem possible, although there is less evidence in this regard.5
The mean incubation period is 5 days.6 In 80% of cases, symptoms are mild-moderate and include fever, dry cough and fatigue. Less frequently, it is associated with congestion, anosmia, myalgia, headache and diarrhea. In severe cases, dyspnea and/or hypoxemia appear one week after infection, and can rapidly progress to acute respiratory failure, septic shock, metabolic acidosis, coagulopathy, and multiple organ failure in 50%.7,8 The mortality rate reported in Spain is 10%, although this is probably an underestimated figure. In the initial stages, laboratory findings show a normal or decreased leukocyte count with lymphopenia, thrombocytopenia, increased liver enzymes, lactate dehydrogenase, creatine kinase, myoglobin, C-reactive protein (maintaining normal procalcitonin), and erythrocyte sedimentation rate. In more advanced stages, elevated D-dimer, troponin and ferritin have been observed as well as laboratory data compatible with renal failure and acute-phase inflammatory markers.9
In this pandemic situation with a very high number of infected patients, symptomatic or asymptomatic, urgent surgical pathologies continue to exist and are the only surgeries that cannot be delayed or cancelled when there is no other medical alternative. Thus, our main objective must be aimed at preserving life-saving medical activities, protecting healthcare workers and, consequently, protecting the general population.
According to a Chinese study carried out in 72 000 patients, digestive involvement due to SARS-CoV-2 caused gastrointestinal symptoms in 10% of cases. Symptoms included diarrhea (2%-10%) and vomiting (1%-10%) one or two days before the onset of fever and respiratory symptoms.10 Another article from the same source reported that 3% of infected patients presented digestive symptoms without associated respiratory symptoms.11 These data lead us to estimate that the digestive involvement is higher than reported, as there are probably many patients with exclusively digestive symptoms who are not tested, so gastrointestinal symptoms could be close to 20%-25% globally. Clinically differentiating this viral involvement from signs of an abdominal surgical emergency is not always easy. It is therefore necessary to be very systematic when taking the clinical history, in which an epidemiological anamnesis should be included, and to use the previously mentioned analytical considerations and the radiological diagnosis.
Organizational factors for urgent surgery in the COVID era: Safety of healthcare workersUrgent care must be guaranteed by adapting general recommendations to the specific framework of each medical center in accordance with the alert scenarios communicated by the AEC.2,3 It is recommended to have an exclusive operating room for COVID-19 patients who have either confirmed or highly suspected infection that cannot be confirmed due to pathologies requiring immediate treatment. It is necessary to create a specific patient transfer route that must be as direct and short as possible, adopting specific prevention and safety measures: use of specific elevators and areas, cleared corridors, areas, placing cloths with bleach along passageways, and adequate disinfection afterwards.
The staff who are in the operating room should be minimized and limited to as few as possible, depending on the complexity of the procedure. Surgeons will only access the operating room at the precise moment to begin the surgery, avoiding being present for other activities in which they do not take part and could be potentially contagious, such as the intubation process. Procedures should be performed by the most trained and skilled staff available in order to minimize the surgical time and any potential complications.
During the procedure, precautionary measures should be taken with the utmost care, following the recommendations below:12,13
- •
Keep doors closed at all times.
- •
Designate a single entry and exit area for surgical staff.
- •
Entry areas should be designated with signs prohibiting the entry of others.
- •
Use class III waste containers.
- •
Remove all non-essential material from the operating room, using protectors for the surfaces to be used.
- •
Avoid entering with personal objects: mobile phones, IDs, etc.
- •
Cloths impregnated with bleach should be placed in the access areas.
- •
Adequate and specific cleaning should follow a specific protocol.
- •
Surgical protocol should follow the general recommendations previously issued by the Association.2,3
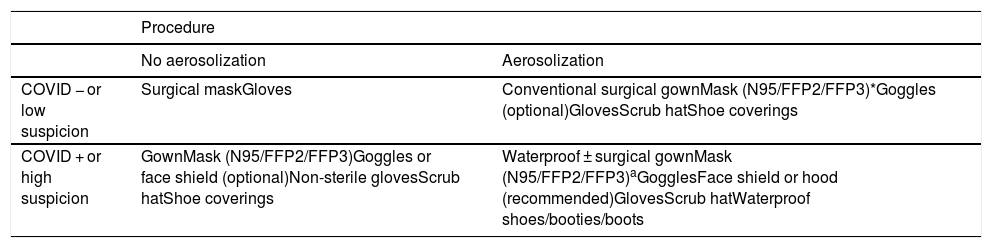
All hospitals must guarantee the availability of personal protective equipment (PPE), including all elements. In the current context of a pandemic with an unacceptable percentage of infected medical professionals (currently close to 30,000 healthcare workers), personnel protection protocols must be strictly complied with. In urgent care, there is no standard time interval in which the existence of a viral coinfection is determined, so these protection measures must be extended with permissiveness. However, given the importance of maintaining equipment availability, rational use of protective equipment is necessary. PPE must be worn in all diagnostic, therapeutic or exploratory procedures that are considered ‘close contact’, but one type of protection or another is used depending on whether the procedure produces aerosolization and the positive, negative or undetermined COVID -19 infection.
In the case of a procedure that does not produce aerosolization, such as a simple physical examination or a patient interview, it should be sufficient to maintain a minimum distance for safety and some basic measures based on the patient’s COVID-19 status.
For procedures that produce aerosolization (orotracheal intubation, surgical intervention, etc.), the measures should be stepped up, regardless of the patient’s status, given the high numbers of asymptomatic and false negatives reported by the available tests.
Table 1 shows the minimum measures that must be taken in each case.14
Protective equipment according to the procedure and patient.
| Procedure | ||
|---|---|---|
| No aerosolization | Aerosolization | |
| COVID − or low suspicion | Surgical maskGloves | Conventional surgical gownMask (N95/FFP2/FFP3)*Goggles (optional)GlovesScrub hatShoe coverings |
| COVID + or high suspicion | GownMask (N95/FFP2/FFP3)Goggles or face shield (optional)Non-sterile glovesScrub hatShoe coverings | Waterproof ± surgical gownMask (N95/FFP2/FFP3)aGogglesFace shield or hood (recommended)GlovesScrub hatWaterproof shoes/booties/boots |
It is essential for all staff to have undergone training on the donning and doffing of PPE, have a checklist of the steps to take, and be supervised to avoid mistakes. The donning/doffing steps are listed in the general recommendations document of the AEC.2,3
Preoperative determination of viral coinfectionIn the current context, it is recommended to determine the COVID-19 status of all patients with surgical urgency, regardless of whether they present symptoms of viral coinfection. The following tools are available:
- •
Real-time polymerase chain reaction (RT-PCR)
- •
Serological tests
- •
Radiology tests (chest radiograph/thoracic computed tomography [CT]/Point-Of-Care UltraSound [POCUS]).
Sampling nasal and pharyngeal secretions to determine viral RNA using the RT-PCR technique is the standard diagnostic test, but its ability to detect positives can be as low as 57%, even in patients with fever.15 Although the procedure requires an approximate time of 4 h, in actual clinical practice it requires a time of no less than 6 h between taking the sample and obtaining the results.
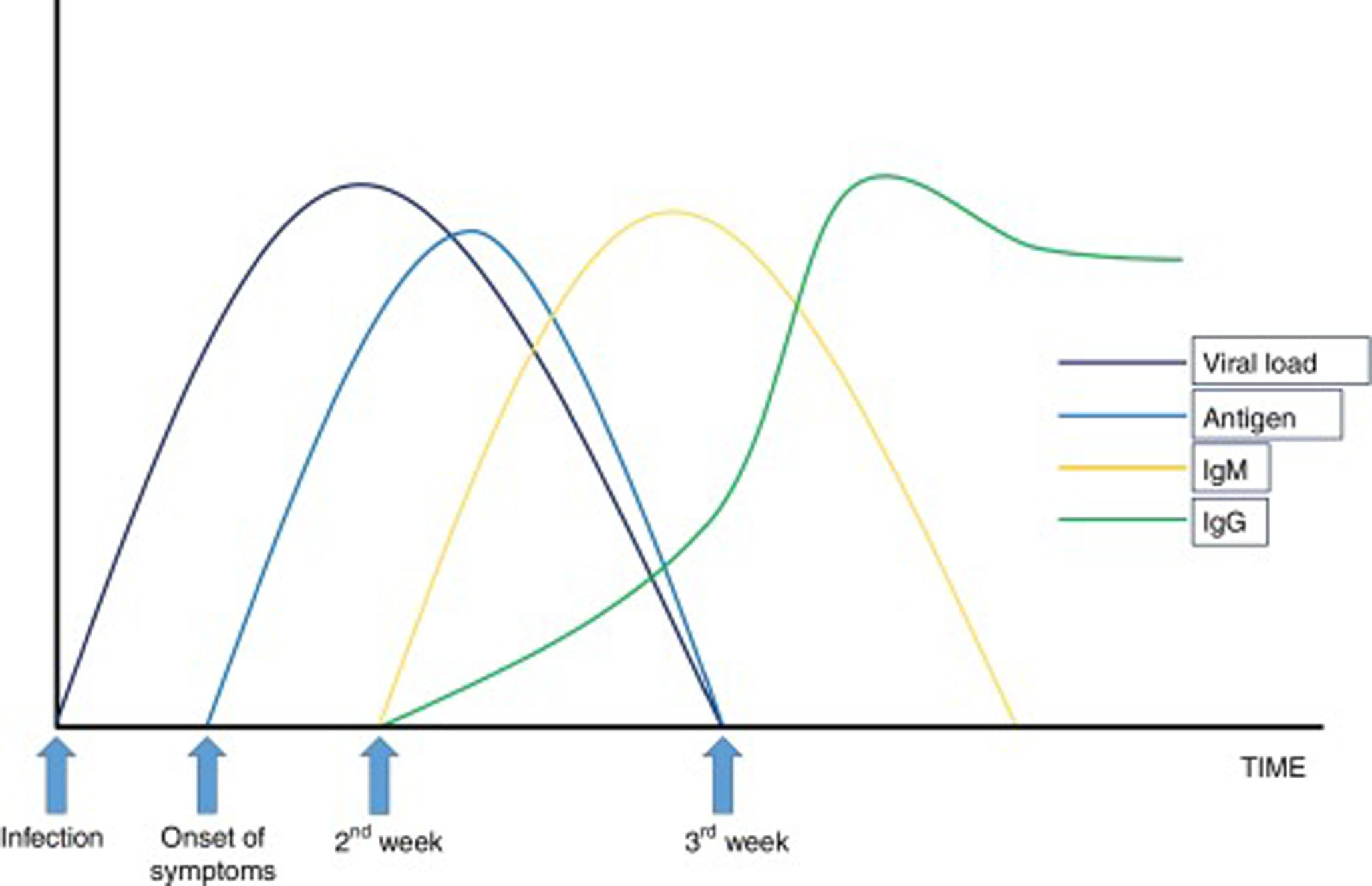
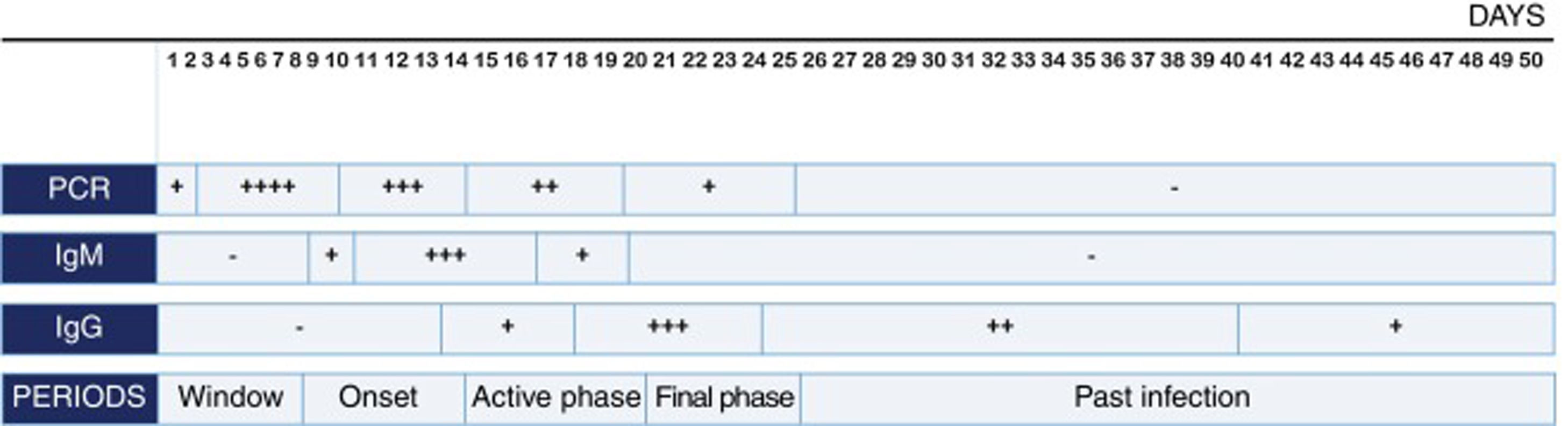
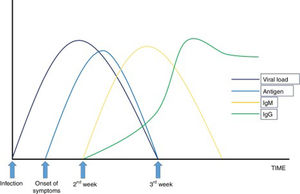
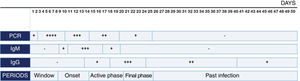
Serological tests, based on the determination in serum of SARS-CoV-2 Ag or secretory immunoglobulins (Ig) A (more theoretical than practical), M and G, are complemented with the information provided by the RT-PCR. Rapid tests are based on immunochromatography and have a sensitivity greater than 75% after the 7th day of disease progression, with a positive predictive value above 95%. ELISA techniques have a sensitivity close to 100% when IgM and IgG detection are combined after 35 days of evolution of the process, but this sensitivity is lower closer to the onset of infection and depends on the protein used for antibody determination.16 Both techniques can be performed quickly in healthcare facilities, they do not require complex material and no difficulty is involved with handling the samples.17
Figs. 1 and 2 summarize the evolutionary profile of the infection and immune response for the correct interpretation of the different tests.
The appearance of ground glass infiltrates on chest radiology studies (simple chest X-ray or chest CT — whichever offers better diagnostic capacity) in the epidemiological context of high incidence and high clinical suspicion of SARS-CoV-2 infection can virtually diagnose the disease, even with negative RT-PCR.18 In cases with mild disease, up to 18% of patients may not have alterations on chest X-ray or thoracic CT at the onset of symptoms,19 but they are present in practically 100% of cases from day 6 on.20
Based on the well-known capacity of ultrasound to detect interstitial lung disease, subpleural consolidations and acute respiratory distress syndrome (ARDS) of any etiology, POCUS has proven very useful both in the early diagnosis of paucisymptomatic patients and in the follow-up of COVID-19. It is a “bedside” tool, repeatable as many times as necessary. Protection measures must always be observed so the equipment does not become fomites for disease transmission. Fourteen areas (3 posterior, 2 lateral and 2 anterior, in each lung) are scanned through the intercostal spaces to cover as much area as possible. The objective is to observe the morphology (integrity) of the pleural line, both with the linear and convex probes. The implementation of an ultrasound score to standardize the findings is currently being studied.21
By unifying all these statements, some general considerations arise on how to proceed in the diagnosis of COVID-19 status in patients requiring urgent surgery. For patients whose treatment cannot be delayed, it is virtually impossible to use the RT-PCR test for SARS-CoV-2 virus. In these patients, we must base our actions on the clinical history, if possible, of both patients and their relations (recent acute respiratory history in the patient or family/cohabitants), analytical parameters (lymphopenia, since the elevation of C-reactive protein will be of little value due to the usual elevation in the context of acute abdominal pathology) and radiology, either a simple chest radiograph or thoracic CT scan and abdominal CT scan if the patient’s condition allows, which could show in both cases the characteristic pattern of predominantly subpleural ground glass infiltrates. If the hospital allows, it is advisable to establish a specific radiological circuit for confirmed patients or those with high suspicion of COVID positivity.22 If available, rapid kits that detect antibodies by immunochromatography are useful. However, given the characteristics of the tests, negativity does not exclude diagnosis.
When surgery can be delayed, it is possible to perform RT-PCR to detect viral load, which should be complemented with chest radiology, preferably thoracic CT scan. In usual clinical practice, these patients will have undergone CT of the abdomen as part of the diagnosis; it is indicated to extend this examination to the thorax and even consider the need for CT scans in processes diagnosed exclusively by ultrasound. When available, SARS-CoV-2 serological techniques can be used. In these patients, it would be preferable to perform ELISA over rapid tests due to the better sensitivity of the former and since the time factor is not as important.
For patients who are admitted for conservative management of any urgent pathology, while the pandemic situation remains active, it is recommended to also proceed with ruling out infection by the novel coronavirus.
Implications in the standard indications for urgent surgeryIn general terms, surgical indications themselves should not change during the pandemic, so an attempt will be made to offer the patient the most appropriate treatment at all times.3 But, as under normal conditions, the surgical indication is influenced by factors dependent on the patient’s general condition, inherent risk of the procedure or pre-existing diseases. During the COVID-19 pandemic, a series of cofactors are added that, beyond changing the indication, lead us to consider alternative options in a very anomalous context. Hence, three circumstances can influence the final therapeutic decision: the possibility of infection of the patient and/or healthcare workers, the existence of SARS-CoV-2 infection, and the impact on the hospital structure, especially regarding the availability of intensive care beds.23
Likewise, the weight of each of these factors is in turn determined by the so-called ‘phases’ or ‘scenarios’ during the pandemic, which the dynamic scale proposed by the AEC refers to. Logically, the number of COVID-19 hospitalizations and the impact on hospital resources are fundamental concerns. Urgent surgical activity is maintained in all scenarios until phases IV (high alert) and V (emergency; more than 75% of conventional and ICU beds occupied by COVID-19 patients). In phase V, however, surgery is contemplated in patients who would not survive if surgery is delayed for a few hours, requiring preoperative triage in collaboration with local ethics committees. Thus, in phases I-III, urgent surgical indications could remain unchanged. However, in phases IV and V, conservative treatments could be considered in some patients in whom the benefit of considering a less resolutive option clearly outweighs the risk of infection, transmission, worsening of pre-existing COVID-19 disease or the unjustified consumption of resources. The fundamental question is to weigh the impact of the intervention itself on the patient’s condition due to COVID-19 versus the clinical result of not treating an urgent process.3 Poor postoperative results have been reported in patients scheduled for surgery, although the extrapolation to urgent patients is complex.24 In contrast, short series have described acceptable results in complicated emergent cases in which the surgical indication was maintained.25 The aggressiveness of surgery itself could be a trigger for a disproportionate immediate inflammatory response,26 which could be deleterious in infected patients. Nonetheless, this nonspecific response is already present in urgent patients, and intervention is (especially in infectious conditions) the best way to begin to mitigate it. On the other hand, in phase IV, only the surgical resolution of vital emergencies is contemplated. The justification for proposing conservative treatments is based on the results of studies indicating that these options offer an acceptable margin of safety, but in no case have they been shown to be more effective. Likewise, the vast majority of conditions in which these alternatives could be considered all require a confirmed diagnosis, almost always by abdominopelvic CT scan, which, in the current context must inexorably be extended to the thorax in order to rule out a SARS-CoV-2 concomitant infection.
Thus, conservative treatment of uncomplicated appendicitis could be considered with at least 3–5 days of intravenous antibiotic treatment, and assuming a recurrence rate in the first year close to 30%.27 Likewise, acute uncomplicated cholecystitis could be treated conservatively, again assuming readmission rates, therapeutic failure and more complex surgeries, which are not negligible.28,29 Finally, the spectrum of conservative management could be broadened to an out-of-hospital regime (in combination with eventual percutaneous drainage, if necessary) in more advanced stages of acute diverticulitis, always with a local inflammatory focus,30 although there is no solid scientific evidence to support this statement. Expanded indications for percutaneous cholecystostomies could be justified in COVID-19 patients during the pandemic due to the potential of worsening the respiratory condition as well as the possibility of receiving antiplatelet treatment due to the high incidence of pulmonary thromboembolism in these patients.31,32
One of the most complex aspects in the current situation is decision-making in extreme scenarios. There are many factors involved when deciding whether a patient is operated on, especially when the prognosis is uncertain or unequivocally poor. These include the severity of the urgent/emergency process, COVID-19 infection, and the possible absence of resources depending on the hospital bed occupancy predictions that guarantee appropriate postoperative care, especially in critical care units. The evaluation of each patient must be extremely thorough and carried out jointly by a multidisciplinary team that includes anesthesiologists as well as an intensive care unit (ICU) coordinator. Furthermore, ethical considerations are key in these cases.33 While in some hospitals there are documents to explicitly establish ‘ceiling of treatment’ protocols, this recommended measure is not widely available. Thus, it seems reasonable to involve the local ethics committee for decisions when logistics allow for their participation. Also, medical professionals should be authorized to make those decisions that, due to their necessary immediacy, do not allow for consultations. It is especially important to establish adequate communication channels, which currently can be extremely complex. In many cases, direct communication with the patient is carried out using protective measures that can depersonalize the doctor-patient interaction, while communication with family members is very likely to be by telephone.
Choice of approach, technique and postoperative resultsThe technique and approach chosen for surgery must be agreed upon by the team, taking in account the pathology, available resources, comorbidities, and suspicion or confirmation of COVID-19 infection. During surgery, the use of electrocautery and tissue dissection with ultrasonic energy sources can generate aerosol particles measuring 0.1μm and 0.35–6.5μm, respectively.34 Thus, it is essential to use PPE with FFP2/FFP3 masks during all procedures and to use watertight smoke aspiration systems. One recommendation is to use low-intensity energy sources to minimize the generation of vapors during tissue dissection and cauterization.
Especially at the beginning of the pandemic, certain publications issued a cautionary message regarding the use of laparoscopic procedures, arguing there was a greater potential for aerosolization. As progress has been made, other considerations have confirmed that laparoscopy, with strict safety protocol compliance, continues to provide the inherent advantages of the approach without constituting an added danger for surgeons. Minimally invasive approaches involve the interposition of a physical barrier between the surgeon and the possible source of infection, thereby avoiding occupational exposure and cross infection. Other advantages of the minimally invasive approach are that it minimizes accidents with sharp instruments to members of the surgical team,35 minimizes the respiratory impact in the postoperative period, and requires shorter hospital stays.36 In laparoscopic procedures, low insufflation pressures (8−11mmHg) are recommended using constant pressure insufflation systems instead of dual devices. To evacuate the pneumoperitoneum, it is necessary to have a closed system (commercial or DIY) before making an incision to assist the extraction of the piece or to finalize the intervention.37 The capacity of the High-Efficiency Particulate Air (HEPA, 99.97% effective for particles ≥0.3μm) or Ultra-Low Particulate Air (ULPA, 99.99% effective for particles ≥0.05μm) should be known for the commercial system available.38 Several DIY systems have been described. All must be closed systems without leaks that evacuate the pneumoperitoneum and surgical smoke into containers holding solutions with proven efficacy in terms of virus elimination capacity, such as 2.6% sodium hypochlorite.39,40
Other recommendations applicable to minimally invasive surgery are the use of the minimum number of trocars necessary, taking care to make the incisions small for tight fit of the trocar to avoid leaks; when possible, balloon trocars should be used. As for the position of the patient during surgery, the use of the forced or prolonged Trendelenburg position should be avoided as it may adversely affect respiratory physiology.
When a surgeon with experience in laparoscopic techniques is not available, or a closed commercial system for the safe evacuation of contaminated pneumoperitoneum is not available, or there is no experience or materials for create a compatible system, it is preferable to perform a laparotomy. The same principles must be respected: minimize the use of high-power energy sources that can generate contaminated smoke, and the smoke generated must be suctioned into closed systems. The use of surgical stapling devices is recommended to minimize surgical time and the risk of sharps incidents. The indication of stomata (permanent and temporary) generates another source of possible transmission that must be taken into account when it comes to their care both by healthcare personnel and family members, although their indication may be necessary to the detriment of any risky anastomosis, especially in high-alert scenarios.
Exposure and lighting during open approaches should be optimal to facilitate the procedure and shorten the time of the procedure as much as possible. Uncomfortable or too small incisions that add difficulty to the procedure should be avoided. It is advisable to use static spacers and abdominal wall protectors, as they not only facilitate exposure of the field, but also minimize the need for additional helpers.
The evolution and postoperative results of confirmed patients or those in the COVID-19 incubation period present a higher incidence of admission to the ICU compared to COVID-19 patients without surgery. Among the factors associated with an unfavorable evolution is advanced age, the association with comorbidity, immunosuppression of any type (including in association with underlying cancer pathology), surgical time and the degree of difficulty of the procedure conducted.41 There are findings that suggest that surgical interventions can accelerate or even exacerbate the progression of COVID-19, although the proportion is still unknown.
Polytrauma patient managementDue to the confinement currently in force in our country, the incidence of blunt trauma injuries due to motor vehicle accidents has decreased considerably. The same is true for penetrating injuries resulting from interpersonal violence. In any case, the maximum saturation of ICU beds and resuscitation units that some hospitals with a large number of COVID-19 patient admissions have been experiencing for weeks now may force them to reconsider the treatment of trauma patients with minimal chances of survival under normal conditions,42 even with optimal perioperative care (inevitable mortality criteria according to the American College of Surgeons classification, especially in geriatric patients with a probability of death >90%-95%). Polytrauma patients should be received in a specific module designed for this purpose. Due to the epidemiological context, and especially in hospitals in the most affected autonomous communities, all multiple trauma patients should be considered potentially infected, and therefore individual protection measures are required, such as waterproof gowns, goggles, high-protection masks, waterproof booties and gloves, which will be used throughout the patient’s care: transfer to CT, interventional radiology, operating room or ICU. In the current situation, the staff who are part of the trauma team providing initial care must be minimized, and maximum caution must be maintained in the management of the airway and in the placement of chest tubes due to the potential for generating aerosols, especially in the presence of hemodynamic instability that precludes COVID-19 screening. When it is necessary to place chest drains or perform thoracotomies for either pneumothorax or hemothorax, all protective measures should be taken. For other trauma pathologies, the necessary technique will be applied, depending on the findings. When an operating room is required for multiple trauma patients with uncertain COVID-19 status, the one reserved for this circumstance should be used.
Some publications recommend postponing evaluation procedures for trauma patients, such as exploratory laparoscopy of the diaphragm in wounds with a thoracoabdominal tract, which should be planned after the respiratory infection has been resolved in patients with COVID-19.43 Within the polytrauma patient context, it also seems reasonable to delay procedures, such as internal fixation of pelvic or other fractures after placement of external fixation, in patients with confirmed infection and radiological evidence of pulmonary involvement. To date, we have found no evidence to recommend modifying the indications and/or techniques of damage control surgery in the context of this pandemic.
FundingNone.
Conflict of interestsThe authors have no conflict of interests to declare related with this article.
Members of the Surgery-AEC-COVID-19 Collaborative GroupSalvador Morales Conde (coordinator), Estíbaliz Álvarez Peña, Mario Álvarez Gallego, José Manuel Aranda Narváez, Josep María Badía Pérez, José María Balibrea del Castillo, Sandra García Botella, Xavier Guirao Garriga, Eloy Espín Basany, Esteban Martín Antona, Elena Martín Pérez, Sagrario Martínez Cortijo, Isabel Pascual Migueláñez, María Dolores Pérez Díaz, José Luis Ramos Rodríguez, Inés Rubio Pérez, Raquel Sánchez Santos
Please cite this article as: Aranda-Narváez JM, Tallón-Aguilar L, Pareja-Ciuró F, Martín-Martín G, González-Sánchez AJ, Rey-Simó I, et al. Atención de la urgencia quirúrgica durante la pandemia COVID-19. Recomendaciones de la Asociación Española de Cirujanos. Cir Esp. 2020;98:433–441.