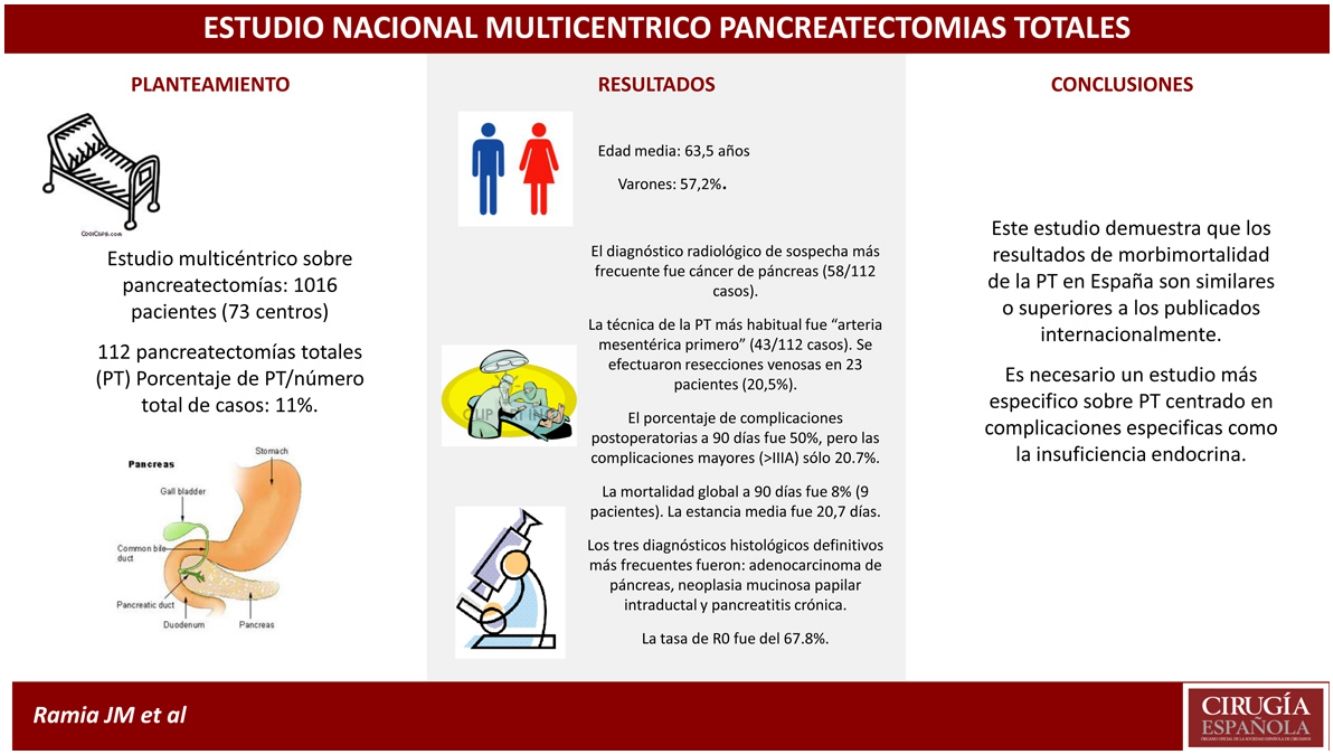
Total pancreatectomy (TP) is an uncommon operation, with indications that have not been clearly defined and non-standardized postoperative results. We present a national multicentric study on TP and a comparison with the existing literature.
MethodsA prospective observational study using data from the national registry of patients after pancreaticoduodenectomy and TP performed for any indication during the study period: January 1–December 31, 2015.
Results1016 patients were included from 73 hospitals, 112 of whom had undergone TP. The percentage of TP from the total number of cases was 11%. The mean age was 63.5 years, and 57.2% were males. The most frequently suspected radiological diagnosis was pancreatic cancer (58/112 cases). The most common TP technique was “mesentery artery first” (43/112 cases). Venous resections were performed in 23 patients (20.5%). The percentage of postoperative complications within 90 days was 50%, but major complications (>IIIA) were only 20.7%. The overall 90-day mortality was 8% (9 patients). The average stay was 20.7 days. The 3 most frequent definitive histological diagnoses were: adenocarcinoma of the pancreas, intraductal papillary mucinous neoplasm and chronic pancreatitis. The R0 rate was 67.8%.
ConclusionsThis study shows that the morbidity and mortality results of TP in Spain are similar or superior to previous publications. More precise TP studies are necessary, focused on specific complications such as endocrine insufficiency.
La pancreatectomía total (PT) es una intervención infrecuente, con unas indicaciones no claramente definidas y unos resultados postoperatorios no estandarizados. Presentamos un estudio multicéntrico nacional sobre PT y una comparación con la literatura existente.
MétodosEstudio prospectivo observacional realizado mediante el registro nacional de pacientes operados de duodenopancreatectomía cefálica y PT realizadas por cualquier indicación durante el periodo comprendido entre el 1 enero y el 31 diciembre del 2015.
ResultadosSe incluyó a 1.016 pacientes, pertenecientes a 73 centros; de ellos, 112 correspondían a PT. El porcentaje de PT/número total de casos es del 11%. La edad media fue 63,5 años y eran varones un 57,2%. El diagnóstico radiológico de sospecha más frecuente fue cáncer de páncreas (58/112 casos). La técnica de la PT más habitual fue «arteria mesentérica primero» (43/112 casos). Se efectuaron resecciones venosas en 23 pacientes (20,5%). El porcentaje de complicaciones postoperatorias a 90 días fue 50%, pero las complicaciones mayores (>IIIA) solo el 20,7%. La mortalidad global a 90 días fue del 8% (9 pacientes). La estancia media fue 20,7 días. Los 3 diagnósticos histológicos definitivos más frecuentes fueron: adenocarcinoma de páncreas, neoplasia mucinosa papilar intraductal y pancreatitis crónica. La tasa de R0 fue del 67,8%.
ConclusionesEste estudio demuestra que los resultados de morbimortalidad de la PT en España son similares o superiores a los publicados previamente. Es necesario un estudio más específico sobre PT centrado en complicaciones específicas, como la insuficiencia endocrina.
Total pancreatectomy (TP) was very popular in the 1960s and 70s because it was considered an excellent oncological procedure for pancreatic cancer as it treated all tumors in cases of multifocal involvement. It also avoided pancreaticojejunal anastomosis, which is the main cause of morbidity and mortality in pancreatic surgery.1–5 However, the high incidence of short- and long-term complications mainly related to the absence of the pancreas (such as severe hypoglycemia and the long-term complications of diabetes mellitus) also entailed a lower quality of life. Furthermore, as there was no demonstrated oncological benefit compared to less radical options and the pancreatic fistula rate dropped as a result of technical refinement, the number of TP performed in the following decades decreased.1–6
In the last 2 decades, however, the concept of preventive surgery in patients at high risk of developing cancer, the emergence of autologous transplantation, better glycemic control after TP or the performance of extended surgeries in advanced neoplasms seem to have led to a resurgence of TP.1,3,7 Currently, there are no clear indications for TP and they are based more on personal experiences than on solid scientific evidence.1,4
In 2015, the Hepato-Biliary-Pancreatic Surgery (HBP) Division of the Spanish Association of Surgeons (AEC) conducted a prospective study on pancreatic surgeries (TP and pancreaticoduodenectomies [PD]) performed in Spain. We present the morbidity and mortality results obtained with in TP.
MethodsSponsored by the HBP Division of the AEC, a nationwide prospective registry was designed for all patients undergoing PD and TP performed for any indication during the period from January 1 to December 31, 2015. Participation in the study was voluntary and open, and the only condition was that the hospital was either a public or private Spanish institution that had performed PD or TP in 2015, regardless of the annual volume (Appendix C, Addendum I). TP performed after PD for oncological reasons or anastomotic problems were not included.
A database was designed and sent to the hospitals when they agreed to participate in the study. Each medical center was responsible for the inclusion of their data in a form created on the www.typeform.com platform, linked to a single Excel database (Microsoft®, Microsoft Corp., Redmond, WA, United States) but unable to access the entire database. To comply with Data Protection requirements, each participating hospital was assigned a specific identification code, and each patient included was assigned an identification code known only to the coordinators of each unit. Only the 3 coordinators of the study had access to the definitive database, but they were unaware of the identity of the patients included. All patients included in the study signed a specific consent form. Fifty-four variables were studied, subdivided into 4 blocks: demographic data; diagnosis/preoperative treatment; operative variables and postoperative variables. The evaluation of specific postoperative complications of pancreatic surgery were categorized by severity according to the classification recommended by the International Study Group of Pancreatic Surgery (postoperative hemorrhage and delayed gastric emptying) and the International Study Group Liver Surgery (biliary fistula).8–10 Postoperative morbidity and mortality were measured after 90 days according to the Clavien-Dindo classification.11 From the database, patients who had undergone TP were selected, without exclusions.
The statistical analysis was merely descriptive, using mean, median, ranges for quantitative variables and percentage (%) for the study of non-numerical variables.
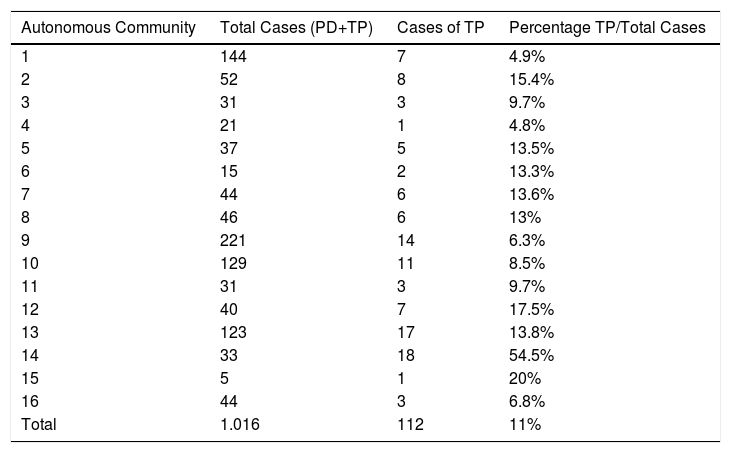
ResultsA total of 1016 patients from 73 hospitals were included in the database (see Appendix B, Addendum 1 for participants). In 904 patients, PD was performed, while 112 underwent TP, and these subjects made up our study group. Table 1 includes the distribution of the TP studied by autonomous communities. The percentage of TP out of the total number of cases included (TP+PD) was 11%, but this varied among the ‘autonomous communities’ of Spain, ranging from 4.9% to 54.5%. Median age was 61 years (range: 35–83), and the distribution by sex was: 64 males (57.2%), 45 females (40.2%), and this datum was not available 3 cases (2.6%). The distribution by ASA category was: 5 ASA i(4.5%); 59 ASA ii(52.7%); 40 ASA iii(35.7%); 6 ASA iv (4.7%); and this datum was not available for 2 patients (3.1%).
Distribution of TP Cases by Autonomous Communities (Regions).
| Autonomous Community | Total Cases (PD+TP) | Cases of TP | Percentage TP/Total Cases |
|---|---|---|---|
| 1 | 144 | 7 | 4.9% |
| 2 | 52 | 8 | 15.4% |
| 3 | 31 | 3 | 9.7% |
| 4 | 21 | 1 | 4.8% |
| 5 | 37 | 5 | 13.5% |
| 6 | 15 | 2 | 13.3% |
| 7 | 44 | 6 | 13.6% |
| 8 | 46 | 6 | 13% |
| 9 | 221 | 14 | 6.3% |
| 10 | 129 | 11 | 8.5% |
| 11 | 31 | 3 | 9.7% |
| 12 | 40 | 7 | 17.5% |
| 13 | 123 | 17 | 13.8% |
| 14 | 33 | 18 | 54.5% |
| 15 | 5 | 1 | 20% |
| 16 | 44 | 3 | 6.8% |
| Total | 1.016 | 112 | 11% |
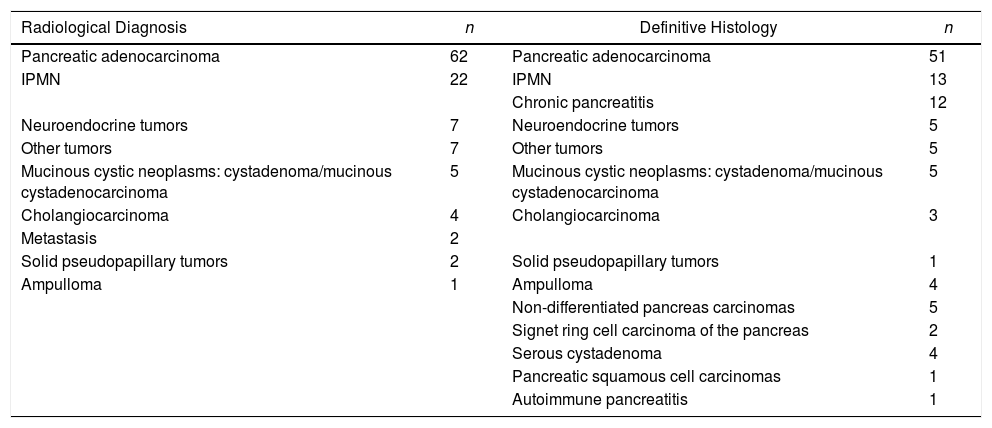
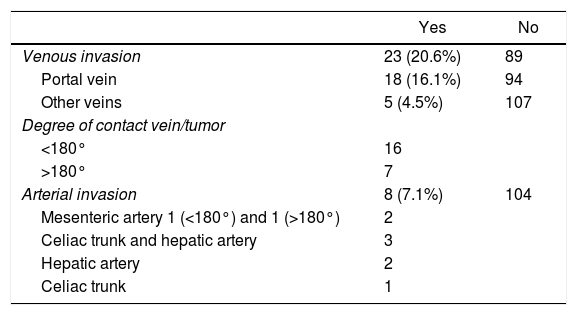
The diagnostic methods performed were: CT in all patients except one; 55% underwent MRI or magnetic resonance cholangiopancreatography; PET/CT was only used in 18.7%. The most frequent suspected preoperative radiological diagnosis was: pancreatic cancer (62 cases), followed by intraductal papillary mucinous neoplasm (IPMN) (22 cases) (Table 2). The radiological location of the tumor was: head of the pancreas in 74 patients (66.1%); body of the pancreas in 5 (13.4%); periampullary in 3 (2.7%); distal common bile duct in 3 (2.7%); ampullary in 2 (1.8%); duodenal in 1 (0.9%); and other locations in 14 (12.5%). Based on the radiological studies, 20.6% of the patients presented some type of venous invasion and 7.1% arterial invasion (Table 3). Six patients received neoadjuvant treatment (5.2%), 3 with chemotherapy and 3 chemoradiotherapy.
Preoperative Radiological Diagnosis.
| Radiological Diagnosis | n | Definitive Histology | n |
|---|---|---|---|
| Pancreatic adenocarcinoma | 62 | Pancreatic adenocarcinoma | 51 |
| IPMN | 22 | IPMN | 13 |
| Chronic pancreatitis | 12 | ||
| Neuroendocrine tumors | 7 | Neuroendocrine tumors | 5 |
| Other tumors | 7 | Other tumors | 5 |
| Mucinous cystic neoplasms: cystadenoma/mucinous cystadenocarcinoma | 5 | Mucinous cystic neoplasms: cystadenoma/mucinous cystadenocarcinoma | 5 |
| Cholangiocarcinoma | 4 | Cholangiocarcinoma | 3 |
| Metastasis | 2 | ||
| Solid pseudopapillary tumors | 2 | Solid pseudopapillary tumors | 1 |
| Ampulloma | 1 | Ampulloma | 4 |
| Non-differentiated pancreas carcinomas | 5 | ||
| Signet ring cell carcinoma of the pancreas | 2 | ||
| Serous cystadenoma | 4 | ||
| Pancreatic squamous cell carcinomas | 1 | ||
| Autoimmune pancreatitis | 1 |
IPMN: intraductal papillary mucinous neoplasm.
Vascular Invasion on Imaging Tests.
| Yes | No | |
|---|---|---|
| Venous invasion | 23 (20.6%) | 89 |
| Portal vein | 18 (16.1%) | 94 |
| Other veins | 5 (4.5%) | 107 |
| Degree of contact vein/tumor | ||
| <180° | 16 | |
| >180° | 7 | |
| Arterial invasion | 8 (7.1%) | 104 |
| Mesenteric artery 1 (<180°) and 1 (>180°) | 2 | |
| Celiac trunk and hepatic artery | 3 | |
| Hepatic artery | 2 | |
| Celiac trunk | 1 | |
TP was performed by subcostal laparotomy in 111 patients and laparoscopically in one case. The ‘mesenteric artery first’ TP technique was the most frequently used (43 cases), the ‘no-touch technique’ in 36 cases and the classical approach in 33 cases. Venous resections were performed in 23 patients (20.5%), with 15 complete and 8 partial portal resections, 15 end-to-end anastomoses, venorrhaphy in 7 patients and in one case venous patch. In the reconstruction technique, a single loop was used in 63 patients (58.9%), 2 loops (one biliopancreatic and one intestinal) in 45 (40.2%), and ‘not available’ in 4 cases. Bile loop access to the supramesocolic region was transmesocolic (107 patients), antecolic3 and retromesenteric.2 Access to the digestive loop was antecolic in 75 patients and transmesocolic in 37. The number of drains used were 2 in 91 patients, one in 18 patients and none in 3. Blood transfusion was not performed in 76 patients (67.8%). The mean number of transfused packed red blood cell units was 1.6 (range: 0–18).
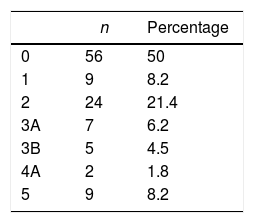
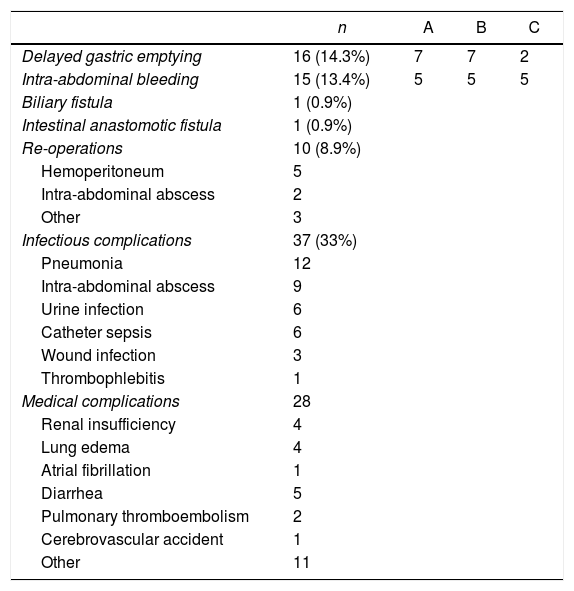
The percentage of postoperative complications within 90 days was 50%, and their distribution according to the Clavien-Dindo classification is shown in Table 4. When we consider the major complications alone (>Clavien-Dindo IIIA), the percentage decreases to 20.7%. Ten patients were re-admitted after being discharged from hospital (8.9%). The overall 30-day mortality was 5.35% (6 patients) and increased to 8% (9 patients) within 90 days. Complications are listed in Table 5. Mean hospital stay was 20.7 days (range: 7–88).
Type of Complications.
| n | A | B | C | |
|---|---|---|---|---|
| Delayed gastric emptying | 16 (14.3%) | 7 | 7 | 2 |
| Intra-abdominal bleeding | 15 (13.4%) | 5 | 5 | 5 |
| Biliary fistula | 1 (0.9%) | |||
| Intestinal anastomotic fistula | 1 (0.9%) | |||
| Re-operations | 10 (8.9%) | |||
| Hemoperitoneum | 5 | |||
| Intra-abdominal abscess | 2 | |||
| Other | 3 | |||
| Infectious complications | 37 (33%) | |||
| Pneumonia | 12 | |||
| Intra-abdominal abscess | 9 | |||
| Urine infection | 6 | |||
| Catheter sepsis | 6 | |||
| Wound infection | 3 | |||
| Thrombophlebitis | 1 | |||
| Medical complications | 28 | |||
| Renal insufficiency | 4 | |||
| Lung edema | 4 | |||
| Atrial fibrillation | 1 | |||
| Diarrhea | 5 | |||
| Pulmonary thromboembolism | 2 | |||
| Cerebrovascular accident | 1 | |||
| Other | 11 |
The histological study (Table 2) showed that the 3 most frequent diagnoses were pancreatic ductal adenocarcinoma, including adenocarcinomas over IPMN (50 patients), IPMN without malignant degeneration12 and chronic pancreatitis,13 but 30% of patients presented other histological diagnoses. The mean tumor size was 43mm (range: 10–250mm). The definitive tumor location was: head of the pancreas (n=51), the entire pancreas (n=44), body of the pancreas (n=8), ampulla (n=4), distal common bile dut (n=3) and ‘not available’ (n=2). The number of resected lymph nodes was 21.7 (0–73), in 26 patients (23.2%) the number of nodes obtained was less than 15, and 39 patients (47.5% of tumor patients) had lymph node involvement. The R0 rate of all the margins studied (retroperitoneal and vascular) was 67.8%.
DiscussionThe first TP was published in 1943 by Rockey in Portland (Oregon).2,3,6 After some initial enthusiasm, the existence of serious complications and few oncological benefits led to a drastic decrease in the number of TP performed.2,6,13 Currently, there has been a slight increase in TP use for certain indications.2,4,6,7,12,13
The most common indications for TP are: malignant tumors in the head of the pancreas where a free-margin resection (R0) cannot be ensured; chronic pancreatitis with complete gland involvement; multifocal IPMN with malignant potential; multiple primary, metastatic or neuroendocrine malignant tumors; patients with hereditary pancreatic cancer or other premalignant diseases. To these indications, we must also add the so-called ‘two-stage TP’, referring to when the pancreatectomy is later completed due to recurrence in the pancreatic remnant or rescue pancreatectomy after pancreaticojejunal anastomotic leak, although this indication has decreased in the last decade.1,5–7,12 More controversial indications are TP in elderly, fragile patients with a high risk of pancreatic fistula and diabetes before surgery, or in patients with complex vascular reconstruction.1,7
Below, we will comment in greater depth on the characteristics of the three most frequent indications, which account for 70% of the total indications in our series: pancreatic cancer, chronic pancreatitis and IPMN.
Pancreatic cancer is usually the most frequent indication in TP series, ranging from 38% to 66%, while in our series it represented 45% of patients.1,4,5 In the published series, the median survival is 15 months, with a 5-year survival rate from 11.3% to 15.9%. There is a growing acceptance that TP in pancreatic cancer enables R0 margins to be obtained, as it increases survival.13
TP can reduce pain, increase quality of life and lower the risk of cancer in patients with chronic pancreatitis. The indications for TP in chronic pancreatitis are not clearly defined, although the most accepted use is in patients with small duct and diffuse glandular involvement, and resistance to medical treatment.1 The possibility of combined autotransplantation could increase TP indications in these patients in the future.12,14
IPMN is being diagnosed more and more frequently.15 Multifocal or diffuse pancreatic involvement makes these lesions difficult to manage. The options are to perform partial resections (which can leave unresected malignant foci) or TP.1,15 The most accepted indications for TP in IPMN are: extensive multifocal disease, diffuse involvement of the main duct and inability to obtain margins without high-grade dysplasia.1,15,16 In 17%–23%, TP is the intervention chosen for patients with IPMN, which in one hospital reached 56% of the total planned TP and 36% of the unplanned procedures.4,5,15,16 It accounted for 11% of our cases.
The study of the series published on TP is not simple. Some series focus on a certain disease, usually pancreatic cancer. In others, the data are given by diseases. Sometimes, there is a control group made up of patients who have undergone PD. Others also include rescue TP during the postoperative period, and the studies are usually retrospective.
The percentage of TP out of the total number of pancreatectomies at each of the participating hospitals was very variable and ranged from 4.8% to 54.5% among the various Spanish autonomous communities; the average was 11%. This difference may be due to different indication criteria among the participating medical centers (for example, performing TP instead of a risky anastomosis, in patients with large vascular resections, or in patients with different diseases being treated). In the published series where this datum is provided, reports range between 8.3% and 28%.2,6,7,12
The percentage of laparoscopic surgery in our study was minimal (0.9%). In other countries, the rate reaches 30% at very specific centers.12 One advantage of TP compared to laparoscopic PD is the absence of pancreatojejunal anastomosis, which is one of the most complex technical points. This percentage will likely increase progressively in coming years.
The morbidity rate in the published TP series ranges between 31.1% and 87%, and is usually determined after 30 days.1,12 Our complication rate after 90 days was 50%, which dropped to 20.7% when only major complications >Clavien IIIA were analyzed, which is lower than the 32% published by Zakaria et al.12 The 30-day mortality rate for TP is 0%–12.5%, while our 30-day mortality rate was 5.35% and reached 8% after 90 days.1,2,4,12,13 A German study on pancreatic surgery, using hospital data from almost 5000 TP over a 5-year period, reported a TP mortality rate of 23%, which rose to 50% when TP was associated with colon resection.17 Hartwig et al. carried out a multivariate analysis on mortality, finding that operative times over 420min, intraoperative bleeding greater than 2000mL and arterial resections are associated with higher mortality.4 The vascular resection rate of the published series ranges from 11.8% to 50%3,12 and was 20% in our patients. The hospital stay in the literature is 10–14 days,4,5,12 while the stay in our study was longer (20.7 days).
We have only found 10 retrospective series since 2007 comparing TP and PD, with disparate results.1,18–23 The morbidity of TP is higher than PD in 3 series, lower in 2 series and similar in the rest.20,22,23 In the series by Casadei et al., the average stay is longer for PD, although the TP has a higher operative time and more vascular resections.7 The quality of life of both techniques is similar in the three related series.1,7,21 Survival in TP is lower in 3 series and similar in the rest.1,18,19 In short, it can be concluded that there are no clear differences in morbidity, mortality, quality of life or survival comparing TP and PD. The great bias of these studies is that the patients analyzed do not present comparable lesions, as the TP group frequently presents more advanced lesions, more vascular resections and a greater potential for malignancy. Likewise, there are no pancreatic fistulae in TP, which is the cause of the more severe morbidity of PD. But, above all, they are not randomized studies, so their results should be taken with caution.1,7
One of the strengths of our study is that it is a prospective study that has had the participation of a large number of pancreatic surgery units in our country. The weaknesses are that it is a multicenter study on non-specific pancreatic surgery for TP, where very important aspects have not been assessed (such as endocrine and exocrine insufficiency); also, there were different indications for TP and varying perioperative management among the hospitals. The E-AHBPA has initiated an exclusive prospective study about TP that may provide us with more specific information.
In conclusion, in this national study on pancreatectomies, we have found that most epidemiological data are similar to other large series. Pancreatic cancer, chronic pancreatitis and IPMN are the 3 most frequent indications. The 90-day morbidity and mortality rates are comparable to published international series.
Conflict of InterestsThe authors have no conflict of interests to declare.
Joan Fabregat Prous and Lluis Secanella, Hospital Universitari Bellvitge, Barcelona
Javier Larrea and Olea, Hospital Universitario Insular de Gran Canaria
Francisco Sanchez Bueno, Hospital Clinico Universitario Virgen de la Arrixaca, Murcia
Francisco Botello Martinez, Hospital Universitario Infanta Cristina, Badajoz
Javier Briceño, Hospital Reina Sofía, Córdoba
Alberto Miyar-de León, Hospital Universitario Central de Asturias, Oviedo
Mario Serradilla and Alejandro Serrablo, Hospital Universitario Miguel Servet, Zaragoza
Joana Ferrer Fabrega and S. Sanchez Cabús, Hospital Clínic, Barcelona
Miguel Angel Gómez Bravo and Javier Padillo, Hospital Universitario Virgen del Rocío, Sevilla
Laia Blanco and J. Balcells, Hospital Universitari Vall d́Hebron, Barcelona
Esteban Cugat and Maribel García Domingo, Hospital Mutua de Terrassa, Terrasa, Barcelona
Luis Muñoz Bellvis, Hospital Clínico Universitario de Salamanca, Salamanca
Maria Dolores Perez Diaz, Hospital General Universitario Gregorio Marañón, Madrid
Julio Santoyo Santoyo and Belinda Sanchez, Hospital Carlos Haya, Málaga
Tihomir Georgiev-Grupo ICD Salud, Hospital Fundación Jiménez Díaz, Hospital Universitario Rey Juan Carlos, Hospital Universitario Infanta Elena, Hospital General de Villalba
Trinidad Villegas, Hospital Virgen de las Nieves, Granada
Silvino Pacho, Complejo Asistencial Universitario de León, León
Luis Díez Valladares, Hospital Universitario Clínico San Carlos, Madrid
Jose Rebollar, Hospital Universitario de Álava, Vitoria-Gasteiz, Álava
Miguel Ángel Suárez Muñoz, Hospital Virgen de la Victoria, Málaga
Elías Domínguez, Complexo Hospitalario Universitario de Pontevedra, Pontevedra
Elena Martín Perez, Hospital de La Princesa, Madrid
Laia Falgueras, Hospital Josep Trueta, Girona
Ignasi Poves, Hospital del Mar, Barcelona
Vicenç Artigas, Hospital Sant Creu i Sant Pau, Barcelona
Luis Sabater, Hospital Clínico Universitario, Valencia
Agustin Garcia Gil, Hospital Clínico Lozano Blesa, Zaragoza
Jose Ignacio Miota de Llama, Hospital General Universitario Albacete, Albacete
Gerardo Manzanet, Hospital Universitari La Plana, Castelló de la Plana
Jose Carlos Pino, Hospital de Son Espases, Palma de Mallorca
Juan Carlos Rodríguez Sanjuán, Hospital Universitario Marqués de Valdecilla, Santander
F. Lluis, Hospital General de Alicante, Alicante
Fabio Ausania, Complexo Hospitalario Universitario de Vigo, Vigo, Pontevedra
Maialen Alkorta Zuloaga, Hospital Universitario Donostia, San Sebastián
Jorge Escartín, Hospital Arnau de Vilanova, Lleida
Manel Salas, Hospital Germans Trias i Pujol, Barcelona
Carlos Domingo, Hospital Doctor Peset, Valencia
Enrique Artigues Sánchez de Rojas, Consorci Hospital General Universitario, Valencia
José Antonio Barreras Mateos, Hospital General Universitario de Elda, Alicante
José María Fernández Cebrián, Hospital Universitario Fundación Alcorcón, Alcorcón, Madrid
Beatriz Pérez Cabrera, Hospital Universitario San Cecilio, Granada
D.Padilla Valverde, Hospital General Universitario de Ciudad Real, Ciudad Real
Alfonso Sanjuanbenito, Hospital Universitario Ramón y Cajal, Madrid
Ignacio Iturburu Belmonte, Hospital de Basurto, Bilbao
Natalia Bejarano and F. García Borobia, Hospital Parc Tauli, Sabadell, Barcelona
Pablo Toral Guinea, Hospital Virgen de la Salud, Toledo
Aylhin Lopez Marcano, Hospital Universitario Guadalajara, Guadalajara
Francisco Asencio Arana, Hospital Arnau de Vilanova, Valencia
Evaristo Varo, Complexo Hospitalario Universitario de Santiago, A Coruña
Rafael Esteban, Instituto Valenciano de Oncología (IVO), Valencia
Juan L Blas, Hospital Royo Vilanova, Zaragoza
José M. Jover Navalón, Hospital Universitario de Getafe, Madrid
Cristina Fernández Martínez, Hospital de Sagunto, Valencia
Enrique Daban Collado, Complejo Hospitalario de Jaén, Jaén
Antonio Calvo Duran, Hospital Universitario Puerta del Mar, Cádiz
J.C. Vicens and J. Romero, Hospital Son Llatzer, Palma de Mallorca
J.M. Badía, Hospital de Granollers, Barcelona
Raquel Sánchez, Quirúrgica Cirujanos Asociados, Barcelona
Ricardo de Miguel Ibáñez, Hospital Virgen de la Salud, Cuenca
Fernando Pardo, Clínica Universitaria de Navarra, Pamplona, Navarra
Carlos Francos von Hunefeld, Complejo Asistencial Hospital Nuestra Señora de Sonsoles, Àvila
Fernando Pereira, Hospital Universitario de Fuenlabrada, Madrid
Francisco Garcia Molina, Hospital de Jerez de la Frontera, Cádiz
Ignacio Rodríguez Prieto, Hospital Universitario Infanta Cristina, Madrid
Alfredo Alonso Poza and Carlos Gilsanz, Hospital Universitario del Sureste, Madrid
Jose Miguel Martínez Albert, Hospital de Manises, Valencia
Miguel Angel Morcillo, Hospital de Orihuela, Alicante
Sagrario Martínez Cortijo, Hospital General Nuestra Señora del Prado, Talavera, Toledo
José Martín Fernández, Hospital Universitario Príncipe de Asturias, Madrid
Jesús Baquedano, Hospital Central de la Defensa, Madrid
José Castell, Hospital Universitario La Paz, Madrid
Javier Aguiló, Hospital Lluis Alcañis, Xátiva, Valencia
Juan Carlos Bernal, Hospital de Requena, ValenciaSupplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.cireng.2019.07.009.