The technical, human, scientific and treatment characteristics of the Units that manage complex pathologies have not been studied in depth.
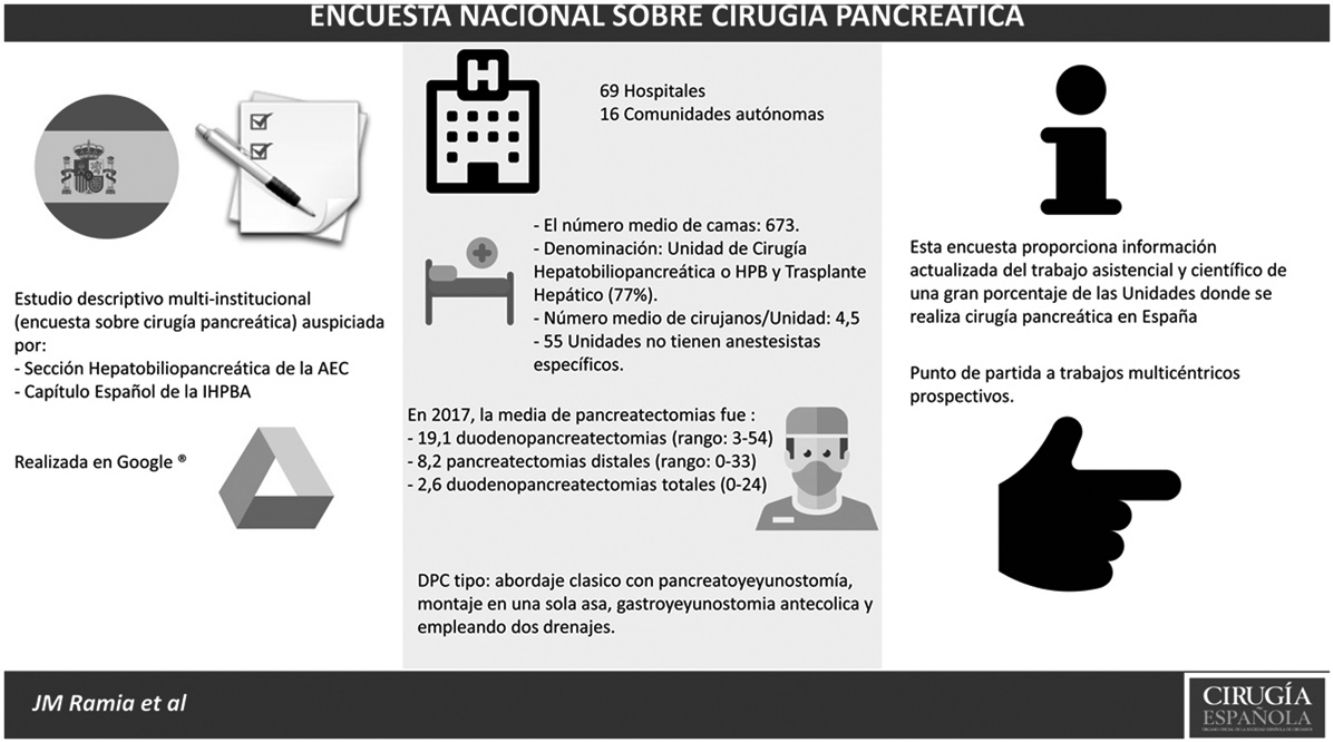
MethodsMulti-institutional descriptive study (survey) developed jointly by the Hepatobiliary-Pancreatic Division of the Spanish Association of Surgeons and the Spanish Chapter of the IHPBA (International Hepatopancreatobiliary Association) on the characteristics of the Units where pancreatic surgery is performed in Spain.
Results82 surveys were sent. 69 medical centers responded (84%), belonging to 16 autonomous regions of Spain. The total population of these regions was 23183262 (50% of the Spanish population). The average number of beds per hospital was 673. The unit that performs pancreatic surgery is a Hepatobiliary-Pancreatic Surgery Unit or HPB and Liver Transplant Surgery Unit in 56 hospitals (77%). The average number of surgeons is 4.5 per Unit. Fifty-five Units (80%) lack specific anesthetists. The number of pancreatectomies performed during 2017 at the hospitals surveyed was 1315 pancreaticoduodenectomies (PD), 566 distal pancreatectomies (DP) and 178 total pancreaticoduodenectomies (TPD). The mean per hospital was 19.1 PD, 8.2 DP and 2.6 TPD. PD was usually performed using a classic approach, with pancreatojejunostomy, single-loop technique, antecolic gastrojejunostomy and using two drain tubes. Only 7 units performed PD laparoscopically and only 13 units did not perform laparoscopic DP.
ConclusionsThis survey provides updated information about the majority of the Units where pancreatic surgery is performed in Spain and could also serve as a starting point for prospective multicenter studies.
Las características técnicas, humanas, científicas y asistenciales de las Unidades que atienden una patología compleja son poco estudiadas y conocidas.
MétodosEstudio descriptivo multiinstitucional (encuesta) desarrollado conjuntamente por la sección Hepatobiliopancreática de la Asociación Española de Cirujanos y el capítulo español de la IHPBA (Asociación Internacional Hepatopancreatobiliar) sobre las características de las Unidades donde se realiza cirugía pancreática en España.
ResultadosSe enviaron 82 encuestas. Respondieron 69 centros (84%) pertenecientes a 16 comunidades autónomas. La suma de habitantes de las áreas propias fue 23.183.262. El número medio de camas por hospital fue 673. La Unidad que realiza la cirugía pancreática es la Unidad de Cirugía Hepatobiliopancreática o Cirugía HPB y Trasplante Hepático en 56 hospitales (77%). El número medio de cirujanos es 4,5 por Unidad. Cincuenta y cinco Unidades (80%) carecen de anestesistas específicos. El número de pancreatectomías realizadas durante 2017 en los centros encuestados fue 1.315 duodenopancreatectomías cefálicas (DPC), 566 pancreatectomías distales (PD) y 178 duodenopancreatectomías totales (DPT). La media por centro fueron 19,1 DPC, 8,2 PD y 2,6 DPT. La DPC más habitual se realiza mediante abordaje clásico, con pancreatoyeyunostomía, montaje en un asa, con gastroyeyunostomía antecólica y 2 drenajes. Solo 7 Unidades efectúan la DPC por laparoscopia y solamente 13 Unidades no realizan PD laparoscópica.
ConclusionesEsta encuesta proporciona información actualizada del trabajo asistencial y científico de un gran porcentaje de las Unidades donde se realiza cirugía pancreática en España, y además puede servir de punto de partida a trabajos multicéntricos prospectivos.
Information about which hospitals perform a certain procedure, how many affected patients they treat, what sort of human and structural characteristics the units have, and which techniques they use is very scarce, both nationally and internationally. The literature on what characteristics a hospital and a surgical unit must fulfill to perform pancreatic surgery is likewise very limited. These characteristics would vary from country to country since healthcare systems are very different among different nations, and the characteristics required in one country cannot be extrapolated to another.1
The Hepatopancreatobiliary Division of the Spanish Association of Surgeons and the Spanish chapter of the IHPBA (International Hepato-pancreato Biliary Association) decided to jointly conduct a survey to identify which hospitals in Spain perform pancreatic surgery, what structural characteristics these hospitals and units have, how many patients are operated on at each hospital, their units’ scientific production, and what techniques are conducted. The aim was to obtain updated information on the state of pancreatic surgery in Spain, which could be the basis for subsequent multicenter studies similar to those carried out in other European countries.
MethodsMulti-institutional descriptive study. The Hepatopancreatobiliary Division of the Spanish Association of Surgeons and the Spanish chapter of the IHPBA have jointly developed an informative survey about the characteristics of pancreatic surgery units. This survey, carried out in Google Drive™, was sent to all hospitals that participated in the Pancreatic Surgery Registry in 2015. In addition, the list of participating hospitals was included in the email presenting the survey, and a request was made that if other hospitals that performed pancreatic surgery were known yet not included on the list, to please provide their contact information in order to include all the national medical centers that perform pancreatic surgery.
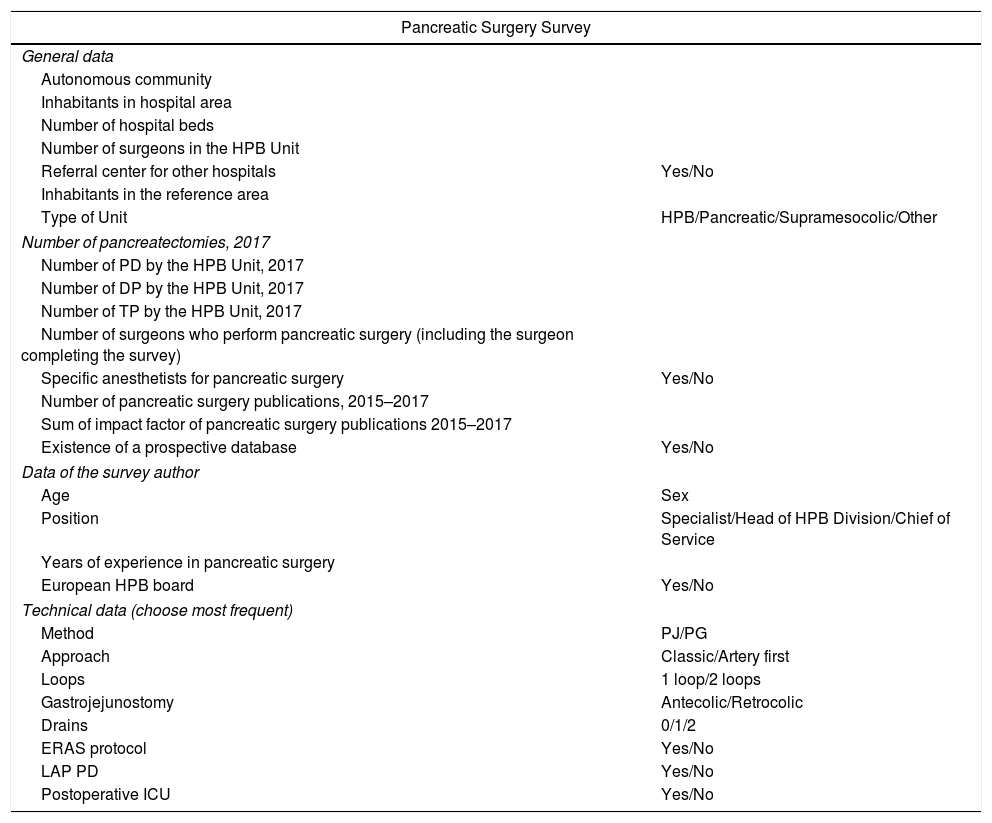
The survey included 4 groups of questions: general hospital data, unit data, data about the person filling out the survey and technical data (Table 1).
Pancreatic Surgery Survey.
| Pancreatic Surgery Survey | |
|---|---|
| General data | |
| Autonomous community | |
| Inhabitants in hospital area | |
| Number of hospital beds | |
| Number of surgeons in the HPB Unit | |
| Referral center for other hospitals | Yes/No |
| Inhabitants in the reference area | |
| Type of Unit | HPB/Pancreatic/Supramesocolic/Other |
| Number of pancreatectomies, 2017 | |
| Number of PD by the HPB Unit, 2017 | |
| Number of DP by the HPB Unit, 2017 | |
| Number of TP by the HPB Unit, 2017 | |
| Number of surgeons who perform pancreatic surgery (including the surgeon completing the survey) | |
| Specific anesthetists for pancreatic surgery | Yes/No |
| Number of pancreatic surgery publications, 2015–2017 | |
| Sum of impact factor of pancreatic surgery publications 2015–2017 | |
| Existence of a prospective database | Yes/No |
| Data of the survey author | |
| Age | Sex |
| Position | Specialist/Head of HPB Division/Chief of Service |
| Years of experience in pancreatic surgery | |
| European HPB board | Yes/No |
| Technical data (choose most frequent) | |
| Method | PJ/PG |
| Approach | Classic/Artery first |
| Loops | 1 loop/2 loops |
| Gastrojejunostomy | Antecolic/Retrocolic |
| Drains | 0/1/2 |
| ERAS protocol | Yes/No |
| LAP PD | Yes/No |
| Postoperative ICU | Yes/No |
PD: pancreaticoduodenectomy; ERAS: Enhanced Recovery After Surgery; HPB: hepatopancreatobiliary; LAP: laparoscopic; DP: distal pancreatectomy; PG: pancreaticogastrostomy; TP: total pancreatectomy; PJ: pancreatojejunostomy; ICU: Intensive Care Unit.
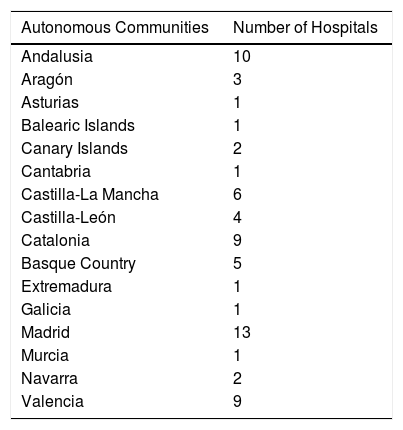
82 surveys were sent, and 69 hospitals responded (84% of the surveys sent) belonging to 16 autonomous communities (Table 2). Regarding the participating centers, 66 are publicly owned and 3 are private hospitals. Forty-eight centers are reference hospitals for other public healthcare areas (69.6%) and 21 only treat patients in their own public healthcare area.
Distribution of Hospitals by Autonomous Communities.
| Autonomous Communities | Number of Hospitals |
|---|---|
| Andalusia | 10 |
| Aragón | 3 |
| Asturias | 1 |
| Balearic Islands | 1 |
| Canary Islands | 2 |
| Cantabria | 1 |
| Castilla-La Mancha | 6 |
| Castilla-León | 4 |
| Catalonia | 9 |
| Basque Country | 5 |
| Extremadura | 1 |
| Galicia | 1 |
| Madrid | 13 |
| Murcia | 1 |
| Navarra | 2 |
| Valencia | 9 |
The sum of inhabitants in the areas of the hospitals consulted is 23183262. According to the provisional population data of the National Institute of Statistics, in 2018 there were 46659302 inhabitants in Spain, so the study area represents 49.7% of the total population of Spain. The number of inhabitants served by the reference hospitals is 21607524 (46.31%). Therefore, by adding the area covered by all participating hospitals and the area covered by those which are also referral hospitals (23183262+2121524), the total is 44790786 inhabitants, which represents 96% of the Spanish population.
The mean number of hospital beds is 673 (range: 150–1403). The distribution by number of beds is as follows, 0–500 beds: 25 hospitals (36%); 501–1000 beds: 37 (54%), and >1000 beds: 7 (10%). The unit performing pancreatic surgery is a Hepatopancreatobiliary Surgery Unit or HPB Surgery and Hepatic Transplantation Unit at 56 hospitals (77%), at 4 it is a Supramesocolic Surgery Unit, at 4 a Biliopancreatic Surgery Unit, at one hospital it is exclusively a Pancreas Surgery Unit, and other unit denominations at 4 hospitals. The average number of surgeons is 4.5 for each unit (range: 1–11) and the median is 4. Fifty-five units (80%) lack specific anesthetists for the unit performing pancreatic surgery.
From 2015 to 2017, 37 units did not publish any articles (53.6%), while 32 units published a total of 145 articles with an impact factor of 272.515. The average number of publications by the publishing participants is 4.53 per unit, and the median is 3. The average impact factor per publication is 1.88. Fifty-five units (80%) have a prospective database.
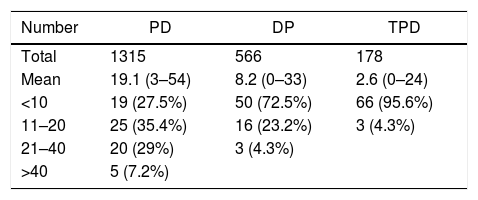
The number of pancreatectomies performed during 2017 in the hospitals surveyed is described in Table 3. Regarding technical questions, the most frequent approach is the so-called ‘classic’ in 44 units (64%), artery first in 9, and both in 16. The usual pancreatojejunal anastomosis performed is pancreatojejunostomy in 54 units (78%), pancreaticogastrostomy (PG) in 10 units and both without preference in 5 units. A single loop is used in 39 units (56%), 2 loops in 28 units and both techniques in 2. The usual gastrojejunal anastomosis is antecolic in 51 (74%) and retrocolic in 18 units. Three units do not place any drains, 15 units a single drain and 2 drain tubes in 51 units.
Number of Pancreatectomies in 2017.
| Number | PD | DP | TPD |
|---|---|---|---|
| Total | 1315 | 566 | 178 |
| Mean | 19.1 (3–54) | 8.2 (0–33) | 2.6 (0–24) |
| <10 | 19 (27.5%) | 50 (72.5%) | 66 (95.6%) |
| 11–20 | 25 (35.4%) | 16 (23.2%) | 3 (4.3%) |
| 21–40 | 20 (29%) | 3 (4.3%) | |
| >40 | 5 (7.2%) |
PD: pancreaticoduodenectomy; TPD: total pancreaticoduodenectomy; DP: distal pancreatectomy.
There is no multimodal rehabilitation protocol in 45 units (64.2%), and 24 do have protocols. Only 7 units perform pancreaticoduodenectomy (PD) by laparoscopy, and 62 units (89.9%) do not perform it. Thirteen units do not perform distal pancreatectomy (DP) by the laparoscopic approach, and 56 do (81.2%). The immediate postoperative period of PD is in the ICU in 53 hospitals, and in 16 post-op is in the post-anesthesia care unit.
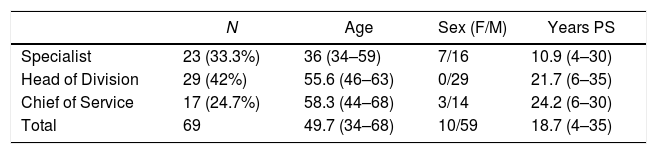
The characteristics of the surgeons who completed the surveys (age, sex, position and experience in pancreatic surgery) are included in Table 4.
Characteristics of the Surgeon Completing the Survey.
| N | Age | Sex (F/M) | Years PS | |
|---|---|---|---|---|
| Specialist | 23 (33.3%) | 36 (34–59) | 7/16 | 10.9 (4–30) |
| Head of Division | 29 (42%) | 55.6 (46–63) | 0/29 | 21.7 (6–35) |
| Chief of Service | 17 (24.7%) | 58.3 (44–68) | 3/14 | 24.2 (6–30) |
| Total | 69 | 49.7 (34–68) | 10/59 | 18.7 (4–35) |
PS: pancreatic surgery; M: male; F: female.
This is the first survey about the care and scientific activity of a large percentage of surgery units that perform pancreatic surgery in Spain.
The characteristics of these units are as follows. 53.7% of the hospitals where these pancreatic surgery units are located are medium or large in size (500–1000 beds), but 36% are in hospitals with less than 500 beds. Most units (77%) treat patients requiring hepatic, biliary and pancreatic surgery. The average number of surgeons is 4.5, with a wide variability ranging from one to 11 surgeons, which logically affects the pancreatectomies/surgeon rate per year. 80% of the hospitals lack specific anesthesiologists for pancreatic surgery, which is a very important datum since Uppal et al. demonstrated in their 2018 study that the existence of a group of anesthetists specialized in this type of surgery improves the results obtained; therefore, this should be an objective in large hospitals with a large number of anesthesiologists.2 Almost 80% of patients spend the immediate postoperative period in the ICU.
As for scientific production, we believe that the actual data are lower than those obtained, since there are national multicenter studies included, meaning that some articles are duplicated in the final article count. On December 31, 2018 we conducted a search in Pubmed 2015–2017 (with the words pancreas AND surgery AND Spain) and we only obtained 32 results.
In the 1990s, very controversial articles were published about the benefits of regionalization of procedures. They described a direct relationship between the volume of patients who undergo surgery for a certain complex pathology and the results obtained, especially in terms of postoperative complications, mortality, average stay and failure to rescue when there are complications.3,4 There are also contradictory publications about the correlation between volume of cases and costs.3,4
Different cut-off values have been used to define hospitals with a low, medium or high volume of pancreatic surgery.3,5 The Dutch study by Van der Geest et al. defined high-volume units as those who perform more than 40 PD, noting that mortality rates are lower and survival rates are higher at these hospitals, probably because they resect more lymph nodes, achieve a higher rate of R0 and administer more postoperative chemotherapy.5 These better results are especially striking in senior patients.6 In Spain, only 5 hospitals perform more than 40PD/year, which is 7.2% of the total number of PD performed. Likewise, only 5 hospitals in the Netherlands perform more than 40PD/year, but they represent 36% of the total number of PD performed, which implies a regionalization of procedures far superior to that of our country. The average number of PD in the Netherlands per hospital is 23, which is slightly higher than the 19 PD obtained in our survey. The information on DP and total pancreaticoduodenectomy (TPD) in relation to the annual volume is very limited in the literature. Only 3 hospitals in Spain carry out more than 20PD/year, and we want to highlight the wide variability in the use of TPD by hospitals that probably have different indications for this intervention, such as TPD in cases of high risk of anastomotic failure not accepted by all pancreatic surgeons.7
In 2002, Figueras et al. proposed that, in order to be a reference hospital, at least 24PD/year should be performed; we have not found data in other countries on this point.1 Another very debated issue is the minimum number of pancreatectomies per year that each center and each surgeon must perform, and there is currently no consensus on which cut-off number is appropriate.5
If we want to define the most frequent PD performed in Spain, we could say that it is performed by laparotomy using a classic approach, with a pancreatojejunal anastomosis using one loop, antecolic gastrojejunostomy and intra-abdominal drain tubes. We will briefly delve into these aspects, verifying that using the most recently published meta-analyses, in most of the technical options there are many uncertainties to be resolved since the superiority of one option over another is not usually evident, and surgeons tend to use the technique that they believe best or with which they are familiar.
The artery first approach has recently become popular in pancreatic surgery, since it theoretically allows the resectability of the pancreatic tumor to be checked and greater R0 resections to be obtained. The meta-analysis by Ironside et al. demonstrates that this approach is accompanied by less intraoperative blood loss, less intraoperative transfusion, lower morbidity, lower incidence of grade B/C fistula, higher rate of R0 resections, better survival and mortality similar to the traditional technique.8 Despite being a fairly recent technical modification, one-third of units already practice it systematically or in combination with the classic approach.
Fistula of the pancreatodigestive anastomosis fistula is the most serious complication after PD. Many alternative techniques have been performed trying to improve the classic duct-to-mucosa pancreatojejunal anastomosis. Among the alternative options is PG.9 In the randomized study conducted in Spain by Figueras et al. comparing pancreatojejunal anastomosis and PG, the authors demonstrated that the rate and severity of pancreatic fistulae was lower with PG.9 The meta-analysis by Menahem et al. confirmed these results.10 Despite these excellent data, PG is not a widely used technique in Spain: 80% of units use pancreatojejunal anastomosis and 20% use PG alone or both techniques. There are no international data to compare these figures with those obtained in Spain.
The position of the gastrojejunal anastomosis after PD can be antecolic or retrocolic. Those who advocate the antecolic position argue that if it is placed in this position it is removed from the pancreatojejunal anastomosis, and if a pancreatic fistula occurs, the gastrojejunal anastomosis is not compromised, providing maintained oral-digestive transit. In the meta-analysis by Joliat et al. antecolic gastrojejunostomy does not improve the results when compared with the retrocolic.11 In Spain, antecolic gastrojejunostomy is mostly used. Regarding the use of one or 2 loops, the meta-analysis by Deng et al. concludes that both techniques obtain similar results in terms of postoperative complications12; and, at the national level, the one-loop technique is used slightly more often than 2 loops.
The use of drains in pancreatic surgery is a controversial issue. A randomized study comparing no drainage vs PD drainage was suspended after observing that the group without drainage had a higher mortality rate (3% vs 12%).13 Huan et al. have subsequently published a meta-analysis, which concluded that the rate of postoperative pancreatic fistula is lower in the group without drainage than in the group with routine drainage, placing drain tubes increases morbidity after PD, and not using drain tubes in DP reduces mortality but the clinically relevant fistula rate is higher.14 The conclusion of the meta-analysis is that drainage should not be used in DP, and not routinely in PD.14 The policy of no drainage is not extended in Spain, and only 3 units practice it; most units use 2 abdominal drain tubes.
Laparoscopic pancreatic surgery has experienced slow diffusion within Pancreatic Surgery Units, especially for PD because it is technically very demanding.15,16 In an international survey about laparoscopic pancreatic surgery answered by pancreatic surgeons, 79% of them performed laparoscopic DP and 29% laparoscopic PD. Also, 70% thought that laparoscopic DP is superior to open DP, but only 10% when referring to laparoscopic PD. Despite these data, laparoscopic DP is probably not as widespread as it seems. In 2015, the Dutch Cancer Study Group published that from 2005 to 2013, only 10% of DP in the Netherlands had been performed laparoscopically. Afterwards, a national tutored training system was implemented, which has increased its use. In a recently published international study comparing laparoscopic PD and open PD, only 17% of patients had undergone laparoscopic, robotic or hybrid surgery.17 The data of our survey are superior to those previously mentioned, since 90% of the groups perform laparoscopic DP, although it has not been possible to determine the exact percentage of DP performed by laparoscopy, and only 10% of the groups perform laparoscopic PD. Only a national registry of all pancreatectomies performed in Spain would provide reliable information. The implementation of laparoscopic PD will probably still be a very slow process.
Enhanced recovery after surgery protocols have been shown to reduce hospital stays and costs without increasing morbidity and mortality; almost one-third of units apply these postoperative protocols after pancreatectomy. Although these protocols have different levels of complexity depending on the number of actions performed, we believe that it is a very relevant rate considering that pancreatectomies, due to their low frequency and complexity, are not usually the group where the use of multimodal rehabilitation is initiated.18
One of the limitations of this survey is that it does not include all units, the data are not prospective and it has not been audited externally. The strength of the study is that the sum of the hospital areas and reference areas covers 95% of the national territory, with the participation of hospitals from 16 autonomous communities. Furthermore, we have included not only publicly owned centers, but also 3 private hospitals.
In conclusion, we believe that this survey provides updated information on the care and scientific contributions of a large percentage of units where pancreatic surgery is performed in Spain. This study could also be a starting point for prospective multicenter studies. We believe that, as in other countries such as the Netherlands, or in other pathologies like gastric cancer, future prospective registries that include all pancreatectomies performed can offer accurate information on surgical and oncological results in a particularly complex pathology like surgery of the pancreas.
Conflict of InterestsThe authors have no conflict of interests to declare.
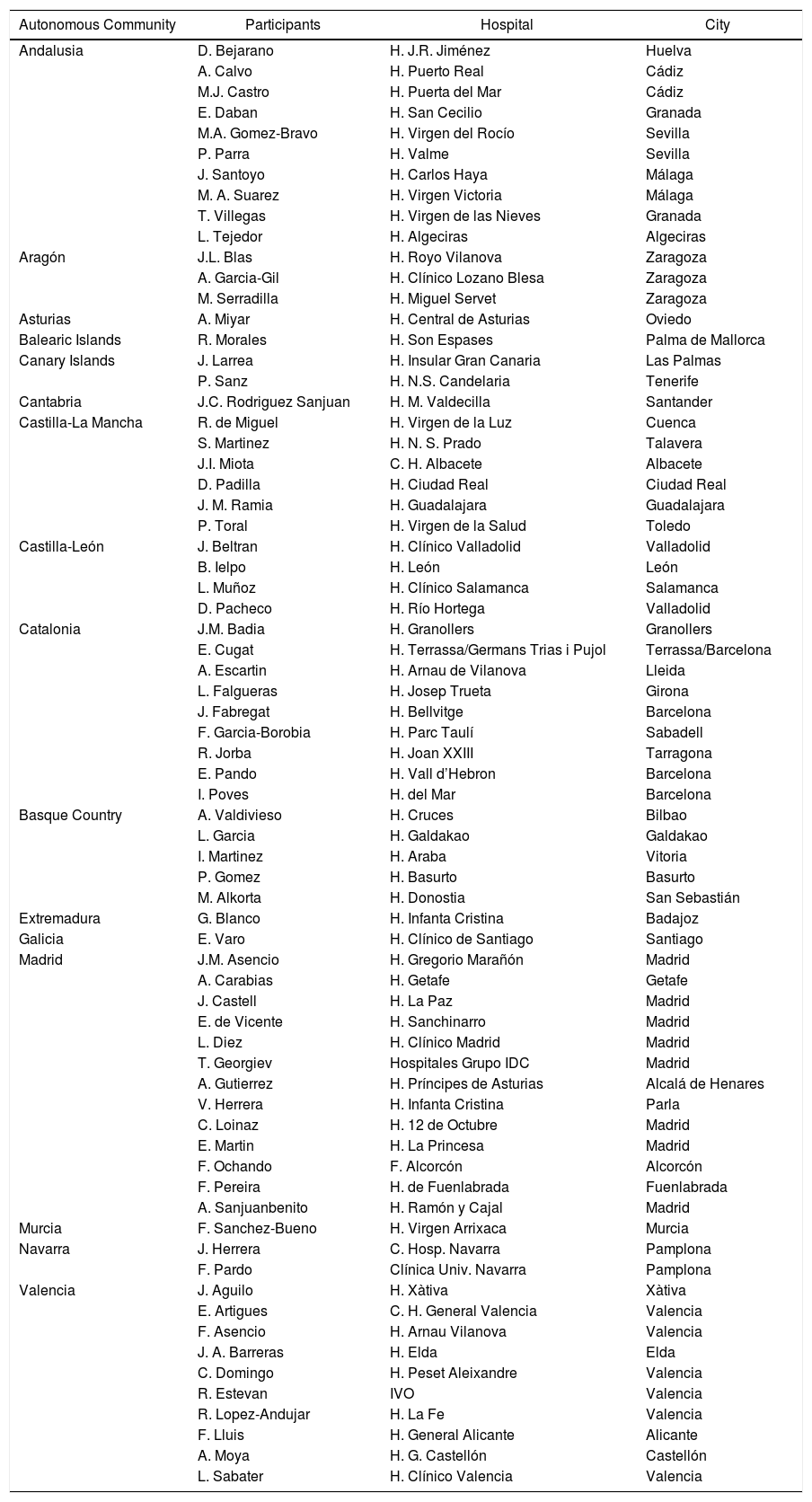
Group members are presented alphabetically (‘autonomous community’ and surgeon).
| Autonomous Community | Participants | Hospital | City |
|---|---|---|---|
| Andalusia | D. Bejarano | H. J.R. Jiménez | Huelva |
| A. Calvo | H. Puerto Real | Cádiz | |
| M.J. Castro | H. Puerta del Mar | Cádiz | |
| E. Daban | H. San Cecilio | Granada | |
| M.A. Gomez-Bravo | H. Virgen del Rocío | Sevilla | |
| P. Parra | H. Valme | Sevilla | |
| J. Santoyo | H. Carlos Haya | Málaga | |
| M. A. Suarez | H. Virgen Victoria | Málaga | |
| T. Villegas | H. Virgen de las Nieves | Granada | |
| L. Tejedor | H. Algeciras | Algeciras | |
| Aragón | J.L. Blas | H. Royo Vilanova | Zaragoza |
| A. Garcia-Gil | H. Clínico Lozano Blesa | Zaragoza | |
| M. Serradilla | H. Miguel Servet | Zaragoza | |
| Asturias | A. Miyar | H. Central de Asturias | Oviedo |
| Balearic Islands | R. Morales | H. Son Espases | Palma de Mallorca |
| Canary Islands | J. Larrea | H. Insular Gran Canaria | Las Palmas |
| P. Sanz | H. N.S. Candelaria | Tenerife | |
| Cantabria | J.C. Rodriguez Sanjuan | H. M. Valdecilla | Santander |
| Castilla-La Mancha | R. de Miguel | H. Virgen de la Luz | Cuenca |
| S. Martinez | H. N. S. Prado | Talavera | |
| J.I. Miota | C. H. Albacete | Albacete | |
| D. Padilla | H. Ciudad Real | Ciudad Real | |
| J. M. Ramia | H. Guadalajara | Guadalajara | |
| P. Toral | H. Virgen de la Salud | Toledo | |
| Castilla-León | J. Beltran | H. Clínico Valladolid | Valladolid |
| B. Ielpo | H. León | León | |
| L. Muñoz | H. Clínico Salamanca | Salamanca | |
| D. Pacheco | H. Río Hortega | Valladolid | |
| Catalonia | J.M. Badia | H. Granollers | Granollers |
| E. Cugat | H. Terrassa/Germans Trias i Pujol | Terrassa/Barcelona | |
| A. Escartin | H. Arnau de Vilanova | Lleida | |
| L. Falgueras | H. Josep Trueta | Girona | |
| J. Fabregat | H. Bellvitge | Barcelona | |
| F. Garcia-Borobia | H. Parc Taulí | Sabadell | |
| R. Jorba | H. Joan XXIII | Tarragona | |
| E. Pando | H. Vall d’Hebron | Barcelona | |
| I. Poves | H. del Mar | Barcelona | |
| Basque Country | A. Valdivieso | H. Cruces | Bilbao |
| L. Garcia | H. Galdakao | Galdakao | |
| I. Martinez | H. Araba | Vitoria | |
| P. Gomez | H. Basurto | Basurto | |
| M. Alkorta | H. Donostia | San Sebastián | |
| Extremadura | G. Blanco | H. Infanta Cristina | Badajoz |
| Galicia | E. Varo | H. Clínico de Santiago | Santiago |
| Madrid | J.M. Asencio | H. Gregorio Marañón | Madrid |
| A. Carabias | H. Getafe | Getafe | |
| J. Castell | H. La Paz | Madrid | |
| E. de Vicente | H. Sanchinarro | Madrid | |
| L. Diez | H. Clínico Madrid | Madrid | |
| T. Georgiev | Hospitales Grupo IDC | Madrid | |
| A. Gutierrez | H. Príncipes de Asturias | Alcalá de Henares | |
| V. Herrera | H. Infanta Cristina | Parla | |
| C. Loinaz | H. 12 de Octubre | Madrid | |
| E. Martin | H. La Princesa | Madrid | |
| F. Ochando | F. Alcorcón | Alcorcón | |
| F. Pereira | H. de Fuenlabrada | Fuenlabrada | |
| A. Sanjuanbenito | H. Ramón y Cajal | Madrid | |
| Murcia | F. Sanchez-Bueno | H. Virgen Arrixaca | Murcia |
| Navarra | J. Herrera | C. Hosp. Navarra | Pamplona |
| F. Pardo | Clínica Univ. Navarra | Pamplona | |
| Valencia | J. Aguilo | H. Xàtiva | Xàtiva |
| E. Artigues | C. H. General Valencia | Valencia | |
| F. Asencio | H. Arnau Vilanova | Valencia | |
| J. A. Barreras | H. Elda | Elda | |
| C. Domingo | H. Peset Aleixandre | Valencia | |
| R. Estevan | IVO | Valencia | |
| R. Lopez-Andujar | H. La Fe | Valencia | |
| F. Lluis | H. General Alicante | Alicante | |
| A. Moya | H. G. Castellón | Castellón | |
| L. Sabater | H. Clínico Valencia | Valencia |
Please cite this article as: Ramia JM, Serrablo A, Gomez Bravo MA y Grupo Español de Cirugía Pancreática (AEC/CE-IHPBA). Encuesta nacional sobre las Unidades de Cirugía Pancreática. Cir Esp. 2019;97:254–260.
The names of the members of the Spanish Group of Pancreátic Surgery (AEC/CE-IHPBA) are listed in Appendix A.