To assess the magnitude of the different causes of anxiety in patients and families, facing surgery.
MethodsCross-sectional multicenter national survey recruiting 1260 participants between patients and companions, analyzing the impact of 14 areas selected based on scientific publications aimed at the general public, concerning patients and/or companions, focused on concern about surgery. Patient sex, age, type of surgery (minor/major) and expected inpatient or ambulatory surgery were analysed. For the companions sex and age, and relationship to patient were analysed. In both cases it was assessed based on a unidimensional scale of 0–10, with 0 being be minimal cause for concern and 10, maximum.
ResultsThe most prominent have been the fear of the unknown, possible complications, the impact on quality of life, the accuracy of diagnosis and possible malignancy of the disease, as well as anaesthesia and pain control. There are significant differences in the involvement of patients and companions; and are also differences by sex and age of the patient; type of surgery (minor/major) and expected hospital admission or not.
ConclusionsThe patient faces surgery with a number of fears that can be reduced with increased information.
Valorar la magnitud de las diferentes causas de inquietud en pacientes y familiares, de cara a la intervención quirúrgica.
MétodosEstudio transversal mediante encuesta multicéntrica nacional, que reclutó a 1.260 participantes entre pacientes y acompañantes y analiza el impacto de 14 aspectos seleccionados a partir de publicaciones científicas y dirigidas al público general, referidas a pacientes o acompañantes, como causa de esta inquietud ante las intervenciones quirúrgicas. Del paciente se indicaba sexo, edad, tipo de cirugía (menor/mayor) e ingreso previsto o no. Del acompañante, sexo y edad, así como parentesco con el paciente. En ambos casos se valoró a partir de una escala unidimensional del 0 al 10, en la que el 0 corresponda a ser mínima causa de inquietud y 10, máxima.
ResultadosLas más destacadas han sido el miedo a lo desconocido, a las posibles complicaciones, a la afectación de la calidad de vida, la veracidad del diagnóstico y posible malignidad de la enfermedad, así como a la anestesia y control del dolor. Hay diferencias significativas en la afectación de pacientes y acompañantes, así como también se aprecian según el sexo y edad del paciente, tipo de cirugía (menor/mayor) e ingreso previsto o no.
ConclusionesEl paciente se enfrenta a la cirugía con una serie de temores que pueden reducirse con una mayor información.
The emotions of fear and anxiety are inherent in human beings. They are generally expressed when patients are going to be subjected to surgery. Although they are controlled, surgical operations are still a form of attack that is accompanied by discomfort and may give rise to complications, which is the chief fear of patients and their families. There may be multiple fears (fear of the unknown, fear of never waking up or of waking up half-way through the operation, fear of technical errors during surgery and fear of pain, etc.). These fears may cause psychological stress that affects the result of the operation itself.
More than four and a half million operations of different degrees of importance are carried out in Spain every year,1 so that many citizens are either operated on in a year or were beforehand, or have a family member who received surgical treatment. In this situation worries emerges which do not always correspond to reality. Nevertheless, they always merit full attention.
We have to offer quality of care at an optimum professional level that is in line with available resources and which aims to ensure the satisfaction of users (patients) and professionals (surgeons).2,3
Due to this the Spanish Association of Surgeons (AEC) and the Quality Management department of the AEC planned to implement this project, with the following objectives:
- •
To evaluate the magnitude of the different causes of concern for patients and their families in connection with general surgical operations.
- •
To compare the different viewpoints of patients and those accompanying them.
- •
To characterise the degree of patient worry according to operation type and their profile.
- •
To involve patients, those accompanying them and surgeons in the quality of care in general surgery.
- •
To identify areas for improvement so that the AEC is able to establish and publish a suitable action plan.
This project commenced in November 2013 with a systematic bibliographical search using Google Scholar of scientific and other sufficiently trustworthy publications aimed at the general public for articles describing the main causes of concern for patients and those accompanying them. After this, the scientific committee selected 14 (10 general articles and 4 articles specifically about anaesthesia) from all of the preselected ones. All of these articles have a degree of scientific evidence of III or IV according to the criteria of the National Health and Medical Research Council (NHMRC).
The minimum calculated sample size was 385 for each case, patients and those accompanying them, adjusted to a general size of 4500000 based on the annual number of surgical operations in Spain,1 from minor to major, with or without admission, with a level of confidence for the sample of 95%, a 5% margin of error and an estimated level of heterogeneity of 50%.
In January 2014, the AEC invited all resident tutors and heads of General and Digestive Surgery departments to designate residents or staff to take part in the study. The notification was then published in the bulletin that was also sent out to all members.
Each participant joined the study through a dedicated e-mail address, filling out a document transferring the results and data, according to Organic Law 15/1999, of 13 December, on Personal Data Protection (LOPD).
The national multicentre survey took place from February to April 2014.
Data was gathered by the doctor or other helpers in the surgery department from 10 randomly selected patients, in the order in which they were seen, who were soon to be operated on (once the date of the operation was known) for any reason. Their 10 corresponding accompanying individuals were also questioned for the paired survey, separately and without knowing the answers of the patient, using a specially designed leaflet. They both had to be over the age of 18 and to agree voluntarily to the survey. They were not identified.
Patient data recorded were sex, age, type of surgery (minor/major) and planned admission or not. Data corresponding to the individual accompanying them were their sex and age, as well as their relationship with the patient (spouse/partner, parent, other family member, friend or other relationship). In both cases they evaluated the following aspects on a single scale from 0 to 10, in which 0 corresponded to a minimum cause of worry and 10 a maximum cause:
- •
Fear of the unknown: the operating theatre, the hospital atmosphere, etc.4–6
- •
Complications: infections, bleeding, seromas, chronic pain, etc.5,7,8
- •
Nutrition: quality, quantity, forced fasting, weakness, etc.9,10
- •
Technical aspects: the doctor's level of training, distrust in medicine, etc.11–14
- •
Quality of life: the risk of sequelae, dysfunctionality, discomfort, etc.5,14
- •
The appearance of the scar.15,16
- •
Affect on work: time off work, company stability, etc.5
- •
The correctness of the diagnosis, possible disease malignity, etc.6,17
- •
Modesty about nakedness, being outside their usual environment, being washed by other people, etc.18–20
- •
The confidentiality of personal information (department/hospital database).20,21
- •
Anaesthesia and pain control during or after the operation, etc.4,5,22–24
Those causes which scored higher than 5 on the scale were considered important.The following questions were asked in connection with anaesthesia.4,5,22–24
- •
Worrying aspects such as noticing something during the operation, waking up or talking while asleep, etc.
- •
Whether they considered themselves to have been suitably informed about the type of anaesthesia (general/local).
- •
About whether they prefer to be awake or not during the operation.
Once the technical secretary had received the leaflets in reply, by fax, traditional or electronic mail, a “double entry” procedure was established using two different workers, to ensure the exactitude of the data entered. A descriptive analysis was carried out of patient and companion segmentation data (autonomous community, sex, age, type of surgery, and planned admission, as well as their relationship). These data were crossed with the scores of the 14 aspects selected using Microsoft Excel 2012 statistical tools to calculate the sample average, standard deviation (SD) and to determine the significance of differences in the comparisons using the P<.05 value by applying the Student t-test for independent samples, with equal estimated variance and considering both distribution tails.
The minimum recommended sample was widely surpassed, and the proportion of patients per autonomous community and population over the age of 18 in Spain25 is similar. One third of the patients awaiting an operation were over the age of 65 years old. This is not surprising, given that life expectancy in Spain stands at 82.4 years.26
The total number of surgical procedures was taken to be the sum of operations carried out with admission, as well as those involving planned and emergency major and minor out-patient surgery undertaken in hospital operating theatres.27
Results83 doctors who were interested in this subject joined the study, and finally 69 (83.13%) took part, from 17 autonomous communities (Appendix A).
A total of 1260 questionnaires were received, from 630 pairs of patients and the individual accompanying them. However, 11 patients had to be excluded (10 because they were under the age of 18 years old and one because their age was not given), as well as 8 accompanying individuals (3 under age and 5 who did not give their age). There were therefore 1241 valid questionnaires, 619 from patients and 622 from those accompanying them.
The relationship between patients and those accompanying them consisted of spouse/partner in 48.11% of cases; a parent in 16.47%; 28.34% another family member; 3.29% a friend, and another type of relationship in 3.79% of cases.
The average age of patients was 54.59 years old (SD 18.45), and 26.33% were aged from 18 to 40 years old, 41.52% from 41 to 65; and 32.15% were older than 65. The average age of those accompanying patients was 51.60 years old (SD 1438); 23.95% were aged from 18 to 40 years old, 59.81% from 41 to 65; and 16.24% were older than 65.
49.43% of the patients were men and 50.24% were women; the corresponding figures for those accompanying them are 36.82 and 62.70%, respectively.
Surgery was minor in 29.98% of cases and major in 70.02%, while 66.07% planned to be admitted.
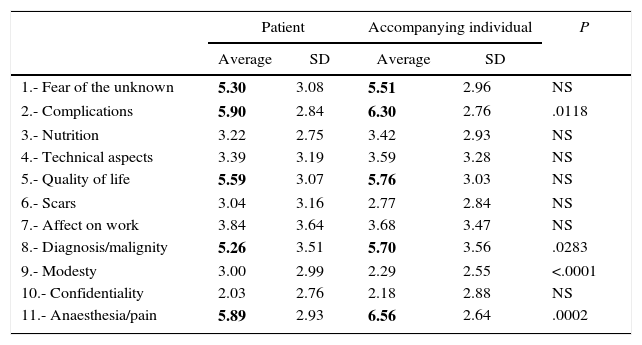
The different causes of worry were evaluated on a scale of from 0 to 10 by the patients and those accompanying them, as shown in Table 1.
Patient-Accompanying Individual Statistics.
| Patient | Accompanying individual | P | |||
|---|---|---|---|---|---|
| Average | SD | Average | SD | ||
| 1.- Fear of the unknown | 5.30 | 3.08 | 5.51 | 2.96 | NS |
| 2.- Complications | 5.90 | 2.84 | 6.30 | 2.76 | .0118 |
| 3.- Nutrition | 3.22 | 2.75 | 3.42 | 2.93 | NS |
| 4.- Technical aspects | 3.39 | 3.19 | 3.59 | 3.28 | NS |
| 5.- Quality of life | 5.59 | 3.07 | 5.76 | 3.03 | NS |
| 6.- Scars | 3.04 | 3.16 | 2.77 | 2.84 | NS |
| 7.- Affect on work | 3.84 | 3.64 | 3.68 | 3.47 | NS |
| 8.- Diagnosis/malignity | 5.26 | 3.51 | 5.70 | 3.56 | .0283 |
| 9.- Modesty | 3.00 | 2.99 | 2.29 | 2.55 | <.0001 |
| 10.- Confidentiality | 2.03 | 2.76 | 2.18 | 2.88 | NS |
| 11.- Anaesthesia/pain | 5.89 | 2.93 | 6.56 | 2.64 | .0002 |
SD: standard deviation; NS: non-significant difference (P>.05).
The values that are above the average on the 0–10 scale are in bold type.
62.14% of the patients were concerned about aspects such as noticing something during the operation, waking up and talking while unconscious, etc. 81.85% of the patients believed that they had been properly informed about the type of anaesthesia (general/local); and while 27.30% of the patients preferred to remain conscious during the operation, 72.70% preferred not to be.
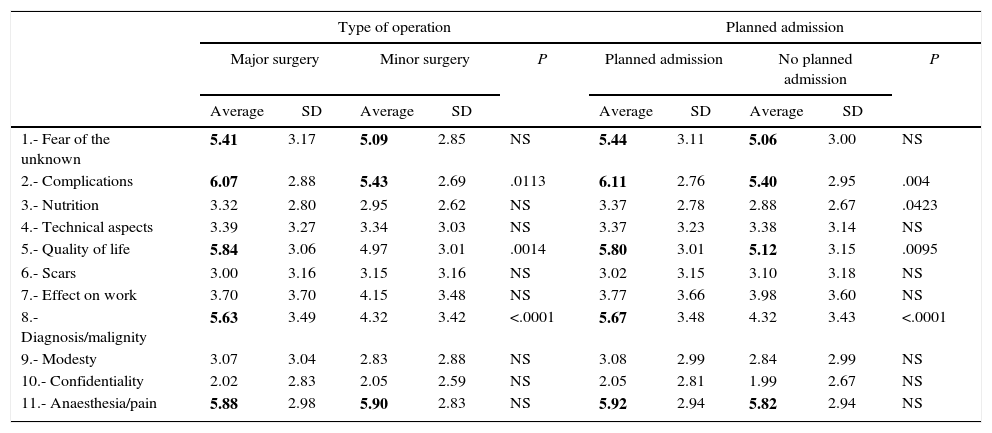
The results of evaluating the different causes of patient worry about the operation (type of operation and planned admission) are shown in Table 2.
Patient Statistics on Type of Operation and Planned Admission.
| Type of operation | Planned admission | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Major surgery | Minor surgery | P | Planned admission | No planned admission | P | |||||
| Average | SD | Average | SD | Average | SD | Average | SD | |||
| 1.- Fear of the unknown | 5.41 | 3.17 | 5.09 | 2.85 | NS | 5.44 | 3.11 | 5.06 | 3.00 | NS |
| 2.- Complications | 6.07 | 2.88 | 5.43 | 2.69 | .0113 | 6.11 | 2.76 | 5.40 | 2.95 | .004 |
| 3.- Nutrition | 3.32 | 2.80 | 2.95 | 2.62 | NS | 3.37 | 2.78 | 2.88 | 2.67 | .0423 |
| 4.- Technical aspects | 3.39 | 3.27 | 3.34 | 3.03 | NS | 3.37 | 3.23 | 3.38 | 3.14 | NS |
| 5.- Quality of life | 5.84 | 3.06 | 4.97 | 3.01 | .0014 | 5.80 | 3.01 | 5.12 | 3.15 | .0095 |
| 6.- Scars | 3.00 | 3.16 | 3.15 | 3.16 | NS | 3.02 | 3.15 | 3.10 | 3.18 | NS |
| 7.- Effect on work | 3.70 | 3.70 | 4.15 | 3.48 | NS | 3.77 | 3.66 | 3.98 | 3.60 | NS |
| 8.- Diagnosis/malignity | 5.63 | 3.49 | 4.32 | 3.42 | <.0001 | 5.67 | 3.48 | 4.32 | 3.43 | <.0001 |
| 9.- Modesty | 3.07 | 3.04 | 2.83 | 2.88 | NS | 3.08 | 2.99 | 2.84 | 2.99 | NS |
| 10.- Confidentiality | 2.02 | 2.83 | 2.05 | 2.59 | NS | 2.05 | 2.81 | 1.99 | 2.67 | NS |
| 11.- Anaesthesia/pain | 5.88 | 2.98 | 5.90 | 2.83 | NS | 5.92 | 2.94 | 5.82 | 2.94 | NS |
SD: standard deviation; NS: non-significant difference (P>.05).
The values that are above the average on the 0–10 scale are in bold type.
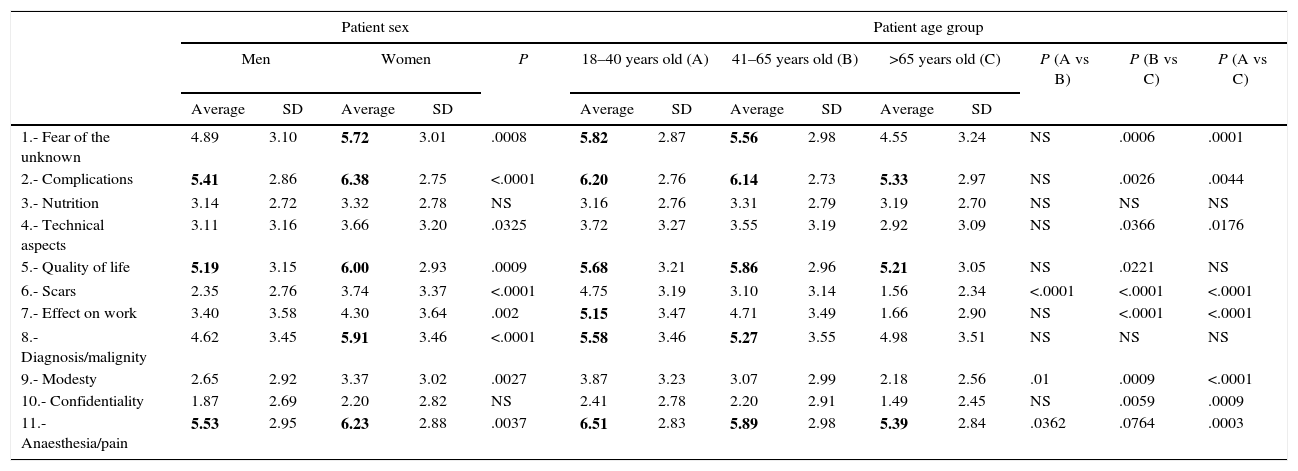
Table 3 shows the relationship between the causes of patient worry and their sex and age.
Patient Statistics for Sex and Age.
| Patient sex | Patient age group | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | P | 18–40 years old (A) | 41–65 years old (B) | >65 years old (C) | P (A vs B) | P (B vs C) | P (A vs C) | ||||||
| Average | SD | Average | SD | Average | SD | Average | SD | Average | SD | |||||
| 1.- Fear of the unknown | 4.89 | 3.10 | 5.72 | 3.01 | .0008 | 5.82 | 2.87 | 5.56 | 2.98 | 4.55 | 3.24 | NS | .0006 | .0001 |
| 2.- Complications | 5.41 | 2.86 | 6.38 | 2.75 | <.0001 | 6.20 | 2.76 | 6.14 | 2.73 | 5.33 | 2.97 | NS | .0026 | .0044 |
| 3.- Nutrition | 3.14 | 2.72 | 3.32 | 2.78 | NS | 3.16 | 2.76 | 3.31 | 2.79 | 3.19 | 2.70 | NS | NS | NS |
| 4.- Technical aspects | 3.11 | 3.16 | 3.66 | 3.20 | .0325 | 3.72 | 3.27 | 3.55 | 3.19 | 2.92 | 3.09 | NS | .0366 | .0176 |
| 5.- Quality of life | 5.19 | 3.15 | 6.00 | 2.93 | .0009 | 5.68 | 3.21 | 5.86 | 2.96 | 5.21 | 3.05 | NS | .0221 | NS |
| 6.- Scars | 2.35 | 2.76 | 3.74 | 3.37 | <.0001 | 4.75 | 3.19 | 3.10 | 3.14 | 1.56 | 2.34 | <.0001 | <.0001 | <.0001 |
| 7.- Effect on work | 3.40 | 3.58 | 4.30 | 3.64 | .002 | 5.15 | 3.47 | 4.71 | 3.49 | 1.66 | 2.90 | NS | <.0001 | <.0001 |
| 8.- Diagnosis/malignity | 4.62 | 3.45 | 5.91 | 3.46 | <.0001 | 5.58 | 3.46 | 5.27 | 3.55 | 4.98 | 3.51 | NS | NS | NS |
| 9.- Modesty | 2.65 | 2.92 | 3.37 | 3.02 | .0027 | 3.87 | 3.23 | 3.07 | 2.99 | 2.18 | 2.56 | .01 | .0009 | <.0001 |
| 10.- Confidentiality | 1.87 | 2.69 | 2.20 | 2.82 | NS | 2.41 | 2.78 | 2.20 | 2.91 | 1.49 | 2.45 | NS | .0059 | .0009 |
| 11.- Anaesthesia/pain | 5.53 | 2.95 | 6.23 | 2.88 | .0037 | 6.51 | 2.83 | 5.89 | 2.98 | 5.39 | 2.84 | .0362 | .0764 | .0003 |
SD: standard deviation; NS: non-significant difference (P>.05).
The values that are above the average on the 0–10 scale are in bold type.
A surgical operation may create certain fears in patients as well as for their family, regardless of their sex or age. Patient fears involve different factors such as the loss of privacy and having to abandon their usual environment and roles. Fears also arise due to the operation itself, such as the lack of certainty about the results of surgery and other fears about anaesthesia, running from whether it will be excessive or will lead to patients revealing personal information due to its effects, up to whether they will be aware of the pain of surgery. For some patients surgery even arouses a fear of death. These fears may lead to high levels of anxiety that will have a negative effect on the surgery.28
In this study we found that the most important causes of worry for the patient are fear of the unknown, possible complications, effects on their quality of life and the disease and diagnosis itself, together with the anaesthesia and pain control. Therefore and as a whole, the 3 main worries are complications, followed by pain control and loss of quality of life. In a Canadian study29 the main worries were connected with the possibility of brain damage in 19% of cases, waking up during surgery in 17% or the fear of dying in 12% of cases. Nevertheless, a few patients (9%) expressed fears about postoperative pain, although this question was not raised in our study.
Those who accompanied patients were found to share similar worries. Complications stand out for them, followed by quality of life and the disease/diagnosis itself. When we compared the opinion of patients with those of their companions, complications, the accuracy of the diagnosis and disease malignity are more important for the latter. However, anaesthesia and pain control are significantly more important for patients. Modesty too is more important for patients than it is for those who accompany them, although in this case the average score is no higher than 3 out of 10.
Differences were detected in patient attitudes depending on the type of operation. Thus, in general patients were less worried about minor surgery than they were about major surgery. There were statistically significant differences regarding complications, loss of quality of life and the disease itself/diagnosis of malignity, which always scored higher in cases of major surgery. There were no differences respecting pain control and fear of the unknown, which stood out in both cases. Only when they were asked about how it would affect their work were the patients awaiting minor surgery more worried, although differences were not significant. These data agree with those of other studies.30
When we compare the fears of patients who required admission with those who were going to be operated as outpatients, the latter and those accompanying them were logically less fearful. The only exception to this concerned the cosmetic harm of scars, although differences here were not significant. Fear of complications, loss of quality of life and aspects of the disease/a diagnosis of malignity were all significantly greater. Worry about nutrition was also higher, although it scored less than 4 out of 10. As in the previous case, fear of the unknown and anaesthesia as pain control were equally important as causes of concern. When other authors31 compared patient stress by measuring the physiological constants of admitted and outpatient surgical patients, they found no significant differences between both groups. However, surveys of family members31 show them to be more worried when surgery will take place on an outpatient basis than when patients are admitted. This is probably due to their worry that they may not be able to deal with any possible problems that arise once they return home.
When the scores awarded by men and women were compared, the latter were generally found to be more affected in terms of the number of causes and degree of worry. There were significant differences between men and women respecting fear of the unknown, possible complications, technical aspects of the operation, quality of life after surgery, scars, effect on work, the possible diagnosis of malignity, modesty and the pain that may be associated with anaesthesia. This fact was also observed in other studies,32–34 in which a significant difference was found in the level of anxiety between men and women faced with major surgery.
Lastly, age too influenced patient fears about surgery. In general, fear falls as patients¿ age. Thus the younger ones (18–40 years old) are the most worried, above all about pain, possible complications, fear of the unknown and losing quality of life. As was the case in other studies35 of heart surgery patients, those older than 65 years old felt a lower level of fear and worry. Some aspects such as the diagnosis of malignant disease were equally important as causes of worry in all of the age groups, with no significant differences between them.
As a limitation of this study, we wish to point out that other studies of patient fears and anxiety before surgery are very heterogeneous. The questions or questionnaires which they use vary widely, hindering comparison of their results. Moreover, the level of scientific evidence of the bibliographical references on this subject in the field of surgery is rather low, corresponding to observational studies and expert opinions (levels of evidence III and IV, respectively, according to the NHMRC criterion).
In spite of the advances in medicine and surgical techniques, there can be no doubt that surgery is an event which worries patients. This stress affects the physiological response of patients and their sensitivity to pain.29 The stress associated with an operation may be reduced by offering patients suitable information, improving results and patient perceptions beforehand. This work depends on the surgeon and may help surgery to be better tolerated and accepted.
These results should form the basis for the creation of an action plan and the implementation of improvements in our hospitals, as well as for surgeons, with the aim of minimising the negative impact of these fears, and increasing patient perceptions of quality prior to a surgical operation.
FinancingThis project was financed by a grant from Abbott España.
Conflict of InterestsThe authors declare that they have no conflict of interests.
The Spanish Association of Surgeons would like to thank the Quality Management Department for its involvement in and leadership of this project. We would also like to thank the Spanish Anaesthesiology, Resuscitation and Pain Therapy Society for helping with the preparation and analysis of the survey, as well as the scientific agency Bate Scientia Salus S.L. for its work as the technical secretary of the project. With especial thanks to the surgeons who took part in this study.
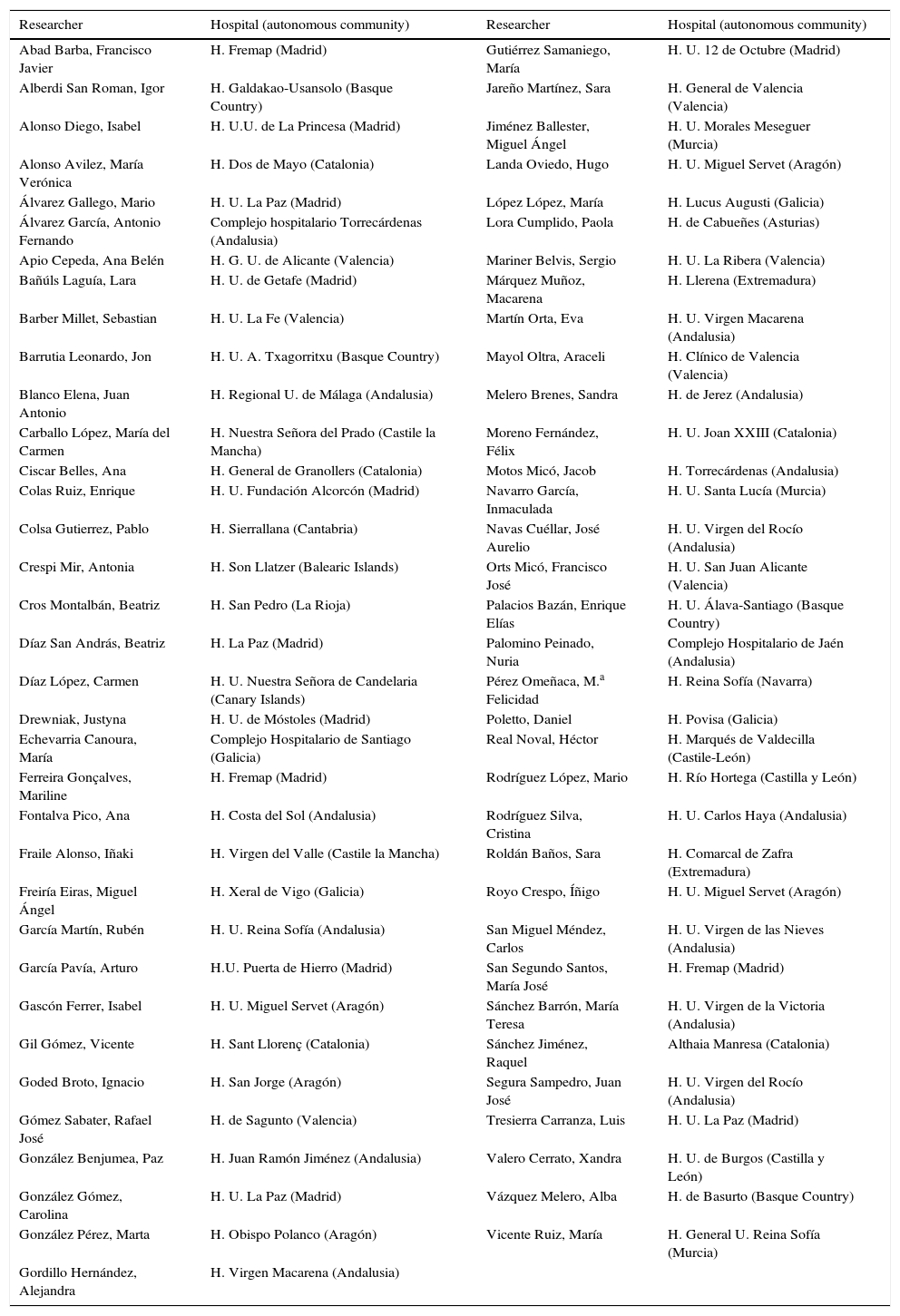
The list of collaborators in the Workgroup of the Spanish Association of Surgeons (AEC)
| Researcher | Hospital (autonomous community) | Researcher | Hospital (autonomous community) |
|---|---|---|---|
| Abad Barba, Francisco Javier | H. Fremap (Madrid) | Gutiérrez Samaniego, María | H. U. 12 de Octubre (Madrid) |
| Alberdi San Roman, Igor | H. Galdakao-Usansolo (Basque Country) | Jareño Martínez, Sara | H. General de Valencia (Valencia) |
| Alonso Diego, Isabel | H. U.U. de La Princesa (Madrid) | Jiménez Ballester, Miguel Ángel | H. U. Morales Meseguer (Murcia) |
| Alonso Avilez, María Verónica | H. Dos de Mayo (Catalonia) | Landa Oviedo, Hugo | H. U. Miguel Servet (Aragón) |
| Álvarez Gallego, Mario | H. U. La Paz (Madrid) | López López, María | H. Lucus Augusti (Galicia) |
| Álvarez García, Antonio Fernando | Complejo hospitalario Torrecárdenas (Andalusia) | Lora Cumplido, Paola | H. de Cabueñes (Asturias) |
| Apio Cepeda, Ana Belén | H. G. U. de Alicante (Valencia) | Mariner Belvis, Sergio | H. U. La Ribera (Valencia) |
| Bañúls Laguía, Lara | H. U. de Getafe (Madrid) | Márquez Muñoz, Macarena | H. Llerena (Extremadura) |
| Barber Millet, Sebastian | H. U. La Fe (Valencia) | Martín Orta, Eva | H. U. Virgen Macarena (Andalusia) |
| Barrutia Leonardo, Jon | H. U. A. Txagorritxu (Basque Country) | Mayol Oltra, Araceli | H. Clínico de Valencia (Valencia) |
| Blanco Elena, Juan Antonio | H. Regional U. de Málaga (Andalusia) | Melero Brenes, Sandra | H. de Jerez (Andalusia) |
| Carballo López, María del Carmen | H. Nuestra Señora del Prado (Castile la Mancha) | Moreno Fernández, Félix | H. U. Joan XXIII (Catalonia) |
| Ciscar Belles, Ana | H. General de Granollers (Catalonia) | Motos Micó, Jacob | H. Torrecárdenas (Andalusia) |
| Colas Ruiz, Enrique | H. U. Fundación Alcorcón (Madrid) | Navarro García, Inmaculada | H. U. Santa Lucía (Murcia) |
| Colsa Gutierrez, Pablo | H. Sierrallana (Cantabria) | Navas Cuéllar, José Aurelio | H. U. Virgen del Rocío (Andalusia) |
| Crespi Mir, Antonia | H. Son Llatzer (Balearic Islands) | Orts Micó, Francisco José | H. U. San Juan Alicante (Valencia) |
| Cros Montalbán, Beatriz | H. San Pedro (La Rioja) | Palacios Bazán, Enrique Elías | H. U. Álava-Santiago (Basque Country) |
| Díaz San András, Beatriz | H. La Paz (Madrid) | Palomino Peinado, Nuria | Complejo Hospitalario de Jaén (Andalusia) |
| Díaz López, Carmen | H. U. Nuestra Señora de Candelaria (Canary Islands) | Pérez Omeñaca, M.a Felicidad | H. Reina Sofía (Navarra) |
| Drewniak, Justyna | H. U. de Móstoles (Madrid) | Poletto, Daniel | H. Povisa (Galicia) |
| Echevarria Canoura, María | Complejo Hospitalario de Santiago (Galicia) | Real Noval, Héctor | H. Marqués de Valdecilla (Castile-León) |
| Ferreira Gonçalves, Mariline | H. Fremap (Madrid) | Rodríguez López, Mario | H. Río Hortega (Castilla y León) |
| Fontalva Pico, Ana | H. Costa del Sol (Andalusia) | Rodríguez Silva, Cristina | H. U. Carlos Haya (Andalusia) |
| Fraile Alonso, Iñaki | H. Virgen del Valle (Castile la Mancha) | Roldán Baños, Sara | H. Comarcal de Zafra (Extremadura) |
| Freiría Eiras, Miguel Ángel | H. Xeral de Vigo (Galicia) | Royo Crespo, Íñigo | H. U. Miguel Servet (Aragón) |
| García Martín, Rubén | H. U. Reina Sofía (Andalusia) | San Miguel Méndez, Carlos | H. U. Virgen de las Nieves (Andalusia) |
| García Pavía, Arturo | H.U. Puerta de Hierro (Madrid) | San Segundo Santos, María José | H. Fremap (Madrid) |
| Gascón Ferrer, Isabel | H. U. Miguel Servet (Aragón) | Sánchez Barrón, María Teresa | H. U. Virgen de la Victoria (Andalusia) |
| Gil Gómez, Vicente | H. Sant Llorenç (Catalonia) | Sánchez Jiménez, Raquel | Althaia Manresa (Catalonia) |
| Goded Broto, Ignacio | H. San Jorge (Aragón) | Segura Sampedro, Juan José | H. U. Virgen del Rocío (Andalusia) |
| Gómez Sabater, Rafael José | H. de Sagunto (Valencia) | Tresierra Carranza, Luis | H. U. La Paz (Madrid) |
| González Benjumea, Paz | H. Juan Ramón Jiménez (Andalusia) | Valero Cerrato, Xandra | H. U. de Burgos (Castilla y León) |
| González Gómez, Carolina | H. U. La Paz (Madrid) | Vázquez Melero, Alba | H. de Basurto (Basque Country) |
| González Pérez, Marta | H. Obispo Polanco (Aragón) | Vicente Ruiz, María | H. General U. Reina Sofía (Murcia) |
| Gordillo Hernández, Alejandra | H. Virgen Macarena (Andalusia) |
The list of co-workers may be found in Appendix A.
Please cite this article as: Fernandez Lobato RC, Soria-Aledo V, Jover Navalón JM, Calvo Vecino JM, Grupo de trabajo de la Asociación Española de Cirujanos (AEC). Encuesta nacional sobre los temores del paciente ante una intervención de cirugía general. Cir Esp. 2015;93:643–650.