The proportion of elderly patients is growing rapidly. Knowing the results of pancreatic surgery in this group of patients would help surgeons to make therapeutic decisions. The objective is to evaluate the surgical outcomes of pancreatic resections in patients over 70 years.
Method:Retrospective study including patients undergoing pancreatic resection during the period 2009–2014. The sample was divided into 2 groups. G1: Patients under 70 years and G2: Patients older than 70 years. Surgical results between the 2 groups were evaluated.
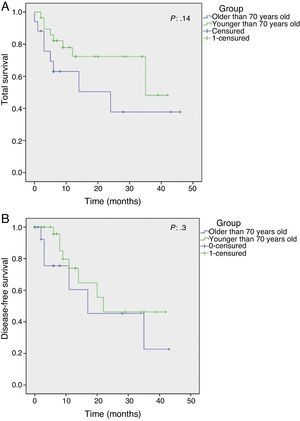
ResultsSeventy-three pancreatic resections were performed, 51 (70%) patients belonged to G1 and 22 (30%) to G2. There were no significant differences between G1 and G2 in terms of operative time and hospitalisation days. No significant difference was obtained in the incidence of delayed gastric emptying, pancreatic fistula or biliary fistula. The overall mortality in the series was 4.1% showing difference between both groups, with 2% in G1 and 13.6% in G2 (P=.04). When a sub-analysis in G2 was made, mortality in this group occurred only in patients with significant comorbidities with ASA≥3 (P=.004). Both groups with oncologic disease had similar overall survival and disease-free survival.
ConclusionsAge should not be a limiting factor for pancreatic resections. The elderly have similar results as younger patients and their increased perioperative mortality is due to the presence of important associated comorbidities rather than age as an independent risk factor.
La proporción de pacientes añosos está creciendo rápidamente. Conocer los verdaderos resultados de la cirugía pancreática en este grupo etario ayudaría para la toma de decisiones terapéuticas. El objetivo es evaluar los resultados quirúrgicos de resecciones pancreáticas en pacientes mayores de 70 años.
Métodos:Estudio retrospectivo que incluye a pacientes tratados mediante resección pancreática en el período 2009-2014. Se dividió la muestra en 2 grupos. G1: pacientes menores de 70 años y G2: pacientes mayores de 70 años. Se compararon los resultados quirúrgicos en ambos grupos.
ResultadosSe realizaron 73 resecciones pancreáticas; 51 (70%) pacientes pertenecieron al G1 y 22 (30%) al G2. No hubo diferencias significativas entre G1 y G2 en cuanto al tiempo operatorio ni a los días de internación. Tampoco se obtuvo diferencia significativa en incidencia de retardo del vaciamiento gástrico, fístula pancreática ni fístula biliar. La mortalidad global de la serie fue del 4,1%: del 2% en G1 y del 13,6% en G2 (p: 0,04). Al realizar un subanálisis en G2, la mortalidad en este grupo ocurrió únicamente en pacientes con comorbilidades significativas con ASA ≥ 3 (p: 0,004). Ambos grupos con enfermedad maligna presentaron similar sobrevida global y libre de enfermedad.
ConclusionesLa edad no debería ser un factor limitante para realizar resecciones pancreáticas. Los pacientes añosos presentan similares resultados quirúrgicos, y su mortalidad perioperatoria aumentada se debería a la presencia de comorbilidades importantes asociadas, y no a la edad como variable independiente.
Cancer of the pancreas is the fourth cause of mortality associated with cancer in the United States, with survival at 5 years of approx. 5%, showing the aggressive nature of this disease.1 In spite of the advances in oncological therapies and the use of neoadjuvant and adjuvant treatments, complete resection (R0) is the sole possibility of cure in these patients. Unfortunately, the majority of patients are considered to be unsuitable for this at the moment of diagnosis, due to the presence of remote metastasis or locally advanced disease.2
Pancreatic surgery has historically been associated with a high rate of perioperative morbimortality.3 With the advances in surgical technique and postoperative care in recent decades, the results of surgery have substantially improved, attaining perioperative mortality levels lower than 2% in high volume hospitals. Nevertheless, operational morbidity in pancreatic surgery remains high: 30%–40% in the majority of cases.4
Due to demographic changes in recent decades the proportion of elderly people in the population has risen considerably. In 2025, 20% of the American population are expected to be older than 65 years old, compared with 12% now.5 Given that the incidence of oncological diseases increases with age, the number of elderly patients diagnosed with pancreatic cancer will increase in coming years.
The rising number of elderly patients with pancreatic disease will create a dilemma for many specialists, as they may have doubts about the treatment of these patients in comparison with younger ones because of their functional state, associated comorbidities and the natural history of the disease itself.
Several studies have described the results of pancreatic surgery in elderly patients, although their conclusions vary and are inconsistent. The majority of these studies report a significant difference in morbidity that is negative for the elderly population.6–8 When mortality is analysed, some studies show no differences,9 while others state that mortality is higher in elderly patients.10
The aim of this study is to analyse the results of pancreatic surgery in an elderly population, to determine whether surgical treatment of these patients is effective.
MethodsA retrospective analysis was carried out using a prospective database that included a consecutive series of patients treated by pancreatic resection over a 5-year period (2009–2014) in a referral hospital.
The sample was divided into 2 groups, depending on whether patients were younger or older than 70 years old (G1: younger than 70 and G2: older than 70). Demographic, clinical presentation, type of surgery, surgical results and pathological variables were compared in both groups. A sub-analysis was also undertaken for those patients with adenocarcinoma, comparing the oncological outcomes in both groups.
The preoperative morbidity of patients was categorised according to the American Society of Anaesthesiologists (ASA) score: I healthy patient, II slight systemic disease, III serious systemic disease, IV serious and incapacitating systemic disease, and V terminal patient.
In all cases surgery was performed by the specialists of the Hepatobiliopancreatic Surgery Department, and surgical specimens were analysed by the same pathologist, who determined the surgical margins and pathological stage.
Preoperative mortality was defined as that occurring during admission or in the 30 days following the operation. Specific complications included in the study were: pancreatic fistula, delayed gastric emptying and biliary fistula. The guidelines of the International Study Group on Pancreatic Surgery (ISGPS) were used to diagnose and classify the pancreatic fistula as well as delayed emptying.
Statistical AnalysisStatistical analysis was carried out using the Statistical Package for the Social Sciences software (SPSS v 22). Categorical variables were compared using the chi2 test (Fisher's exact test) while continuous variables were compared using Student's t-test. Survival curves were developed using the Kaplan–Meier method, and differences in survival over the long term in both groups were compared using the log-rank test. Results where P<.05 were considered significant.
Results73 pancreatic resections were performed in the study period. 51 (70%) patients were in G1 of those aged under 70 years old, and 22 (30%) were in G2 of those older than 70 years old. The average age in G1 was 57.2 (22–69) years old, while in G2 it was 76.6 (70–91) years old (P<.001). There were no significant differences in clinical presentation, previous biopsy or the need for preoperative biliary drainage. The patients in G2 presented a higher number of comorbidities, as shown by a higher ASA score, in comparison with those in G1 (ASA III/IV 32 vs 10%, respectively) (P:.01) (Table 1).
There were no significant differences between the surgical procedures used in G1 and G2: cephalic duodenopancreatectomy (CDP) 65% vs 55%, corporocaudal pancreatectomy 31% vs 40%, complete duodenopancreatectomy 2% vs 5%, and in G1 one enucleation was performed (2%). Nor were there significant differences in operating time between G1 and G2, which in CDP was (5.2h vs 4.7h) and in corporocaudal pancreatectomy (3.1h vs 3.8h) or in the use of intraoperational blood transfusions (1 vs 3 BCU) (Table 2).
Surgical Patient Variables.
| G1 | G2 | P | |
|---|---|---|---|
| CDP (%) | 36 (65) | 12 (55) | NS |
| CDP lap (%) | 1 (2) | 0 | NS |
| CCP (%) | 16 (31) | 9 (40) | NS |
| PPC lap (%) | 11 (21) | 3 (14) | NS |
| TDP (%) | 1 (2) | 1 (5) | NS |
| Enucleation (%) | 1 (2) | 0 (0) | NS |
| Time CDP op (h) | 5.2 (2.5–10) | 4.7 (3–6.5) | NS |
| Time CCP op (h) | 3.1 (2–4.5) | 3.8 (1.5–6.5) | NS |
| Transfusion op (BCU) | 1 | 3 | NS |
CDP: cephalic duodenopancreatectomy; TDP: total duodenopancreatectomy; CCP: corporocaudal pancreatectomy; BCU: blood cell units.
No significant differences between G1 and G2 were found when the times spent in the intensive care unit were compared (4.1 days vs 3.4 days) as well as the total length of hospitalisation (11.2 days vs 10.8 days) or in the incidence of postoperative complications. 27.4% presented a type B or C pancreatic fistula in G1, as did 18.1% in G2; 10% in G1 and 9% in G2 presented delayed gastric emptying; and biliary fistula was present in 6% of G1 patients and 4% of those in G2. There were differences between both groups in terms of perioperative mortality, as it stood at 2% in G1 and 13% in G2 (P:.04) (Table 3). Nevertheless, when the patients in G2 were subjected to a sub-analysis, all of the patients with mortality had major associated comorbidities (ASA III/IV) while no G2 patient with ASA I/II presented mortality (P:.004) (Table 4). I.e., that although in single variant analysis being older than 70 years old as well as an ASA score≥III are associated with perioperative mortality, when multivariant analysis is performed only the preoperative ASA is associated with this adverse outcome (Table 5).
Surgical Results of Patients.
| G1 | G2 | P | |
|---|---|---|---|
| Admission for therapy (d) | 4.1 (0–39) | 3.4 (0–17) | NS |
| Total admission (d) | 11.2 (3–44) | 10.8 (2–28) | NS |
| Pancreatic fistula (%) | 25 (49) | 9 (40) | NS |
| B/C type fistula (%) | 14 (27) | 4 (18) | NS |
| Delayed emptying (%) | 5 (10) | 2 (9) | NS |
| Biliary fistula (%) | 3 (6) | 1 (4) | NS |
| Perioperative mortality (%) | 1 (2) | 3 (13) | .04 |
With respect to histopathology, a larger number of cancers were found in G2 (77%) than in G1 (57%), although this difference was not statistically significant. The several variants of malignant neoplasias were homogeneous in both groups (Table 6). Tumour stages and surgical margins were also similar. Although fewer patients in G2 received adjuvant treatment, this difference was not significant (Table 7).
Malignant Histopathological Diagnoses in Both Groups.
| G1 n (%) | G2 n (%) | P | |
|---|---|---|---|
| Cancer | 29 (57) | 17 (77) | NS |
| Duct adenocarcinoma | 19 (65) | 11 (65) | NS |
| Neuroendocrine cancer | 4 (14) | 2 (12) | NS |
| Papillary cancer | 3 (10) | 1 (6) | NS |
| Mucinous cystoadenoca | 2 (8) | 2 (11) | NS |
| Anaplastic cancer | 1 (3) | 0 (0) | NS |
| Distal biliary duct cancer | 0 (0) | 1 (6) | NS |
Tumour Stages, Resection Margins and Adjuvant Therapy in Both Groups.
| G1 n (%) | G2 n (%) | P | |
|---|---|---|---|
| T 1 | 3 (10) | 5 (29) | NS |
| T 2 | 5 (17) | 3 (18) | NS |
| T 3 | 18 (63) | 8 (47) | NS |
| T 4 | 3 (10) | 1 (6) | NS |
| N+ | 16 (55) | 10 (59) | NS |
| R 0 | 22 (75) | 11(65) | NS |
| R 1 | 7 (25) | 5 (30) | NS |
| R 2 | 0 | 1(5) | NS |
| CMT | 23 (80) | 9 (52) | NS |
| RT | 2 (7) | 1 (5) | NS |
CMT: chemotherapy; RT: radiotherapy.
With an average follow-up of 14 months (6–46) in adenocarcinoma patients, the Kaplan–Meier curves reflect an overall survival of 30.4 months for G1 patients (95% CI: 23–36) compared with 23.3 months in G2 (95% CI 12–33) (P:.14) and an average disease-free survival in G1 of 26.8 months (95% CI 19–34) and 22.5 months in G″ (95% CI: 11–33) (P:.3) (Fig. 1A and B).
DiscussionThe high rate of surgical morbidity associated with pancreatic surgery and the known natural history of malignant pancreatic disease tend to create a dilemma for patients as well as surgeons regarding how to treat elderly patients. Several studies describe how many therapeutic decisions are based on patient age, so that many elderly patients receive less aggressive surgical treatment as well as less systemic adjuvant treatment; i.e., in many situations patient age is a decisive factor leading to a rejection of surgery even in cases when the disease is surgically resectable. This gives rise to worse oncological results in elderly patients.11–13
The elderly population will increase over time due to demographic changes, so that the number of elderly patients with pancreatic disease that can be treated surgically will also increase. In the USA the majority of pancreatic cancers are diagnosed in patients aged from 75 to 84 years old, while the average age at diagnosis is 71 years old.14 In fact, the proportion of elderly patients treated using pancreatic surgery has increased in the majority of referral hospitals over recent years. Sohn et al.10 in Johns Hopkins Hospital show an increase in the number of octogenarian patients treated using CDP. This stood at 2% in the decade after 1980 and reached 9% in 1996. We too noticed an increase in the number of elderly patients in our department over the years, and 30% of all pancreatic surgery patients were older than 70 years old in the period 2009–2014. This is why knowing the true surgical and oncological outcomes in these patients will aid therapeutic decision-making in an increasingly large group of patients.
Several studies have described worse surgical results in terms of morbimortality in elderly patients. Bathe et al.15 show higher perioperative mortality (within 30 days after the operation) in patients older than 75 years old, while Rial et al.16 describe age as an independent risk factor for higher morbimortality in pancreatic surgery. In our series, we observed no significant differences in the complications index between groups of patients, with similar incidences of pancreatic fistula, delayed emptying and biliary fistula. When perioperative mortality was analysed, we found that results were worse for patients over the age of 70 years old, at 13% in elderly patients vs 2% in younger ones (P:.03). However, when sub-analysis was performed on the group of older patients, it was found that all cases of mortality involved patients with important associated comorbidities, with a preoperational ASA score of III/IV. Thus no patient older than 70 years old and ASA I/II died, while 42% of patients with ASA III/IV did suffer this adverse outcome (P:.003). Therefore, age does not have an independent effect on the results of surgery, as these are affected more by the comorbidities associated with this age group.
When the pathologies of both groups are compared, we are able to determine a tendency towards more malignant disease in the older patients, which had an incidence of cancer of 77%, compared with malignant histology in 57% of the patients under the age of 70 years old. Although more advanced tumour stages could be expected to be found in elderly patients, due to delay in diagnosis or treatment, we did not detect this difference in our series, where both groups had similar stages and resection margins.
Several centres have also studied the oncological results in this group of patients. Jin He et al.17 compare the population of pancreatic adenocarcinoma in patients younger than 45 years old with others over the age of 75 years old, and they found a statistically significant difference in average survival time in favour of the younger patients (19 months vs 16 months). On the contrary, Riediger et al.18 showed that age is not an independent risk factor for mortality in connection with this cancer. In our series, although a longer survival time and disease-free survival were found in the younger group, this difference is not statistically significant. Additionally, we also found a tendency to use less adjuvant chemotherapy treatment in elderly patients, and this may partially explain the difference in the results.
To conclude, patient age should not be a restrictive factor in the surgical treatment of pancreatic disease. Elderly patients present similar surgical morbidity to that of younger patients, and their increased perioperative mortality is due to the presence of major associated comorbidities, and it is not associated with age as an independent variable. Moreover, the oncological results in elderly patients are acceptable, so that surgery should always be considered as a treatment in this age group.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Schlottmann F, Iovaldi ML, Capitanich P, McCormack L. Resultados de la cirugía pancreática en pacientes mayores de 70 años. Cir Esp. 2015;93:638–642.