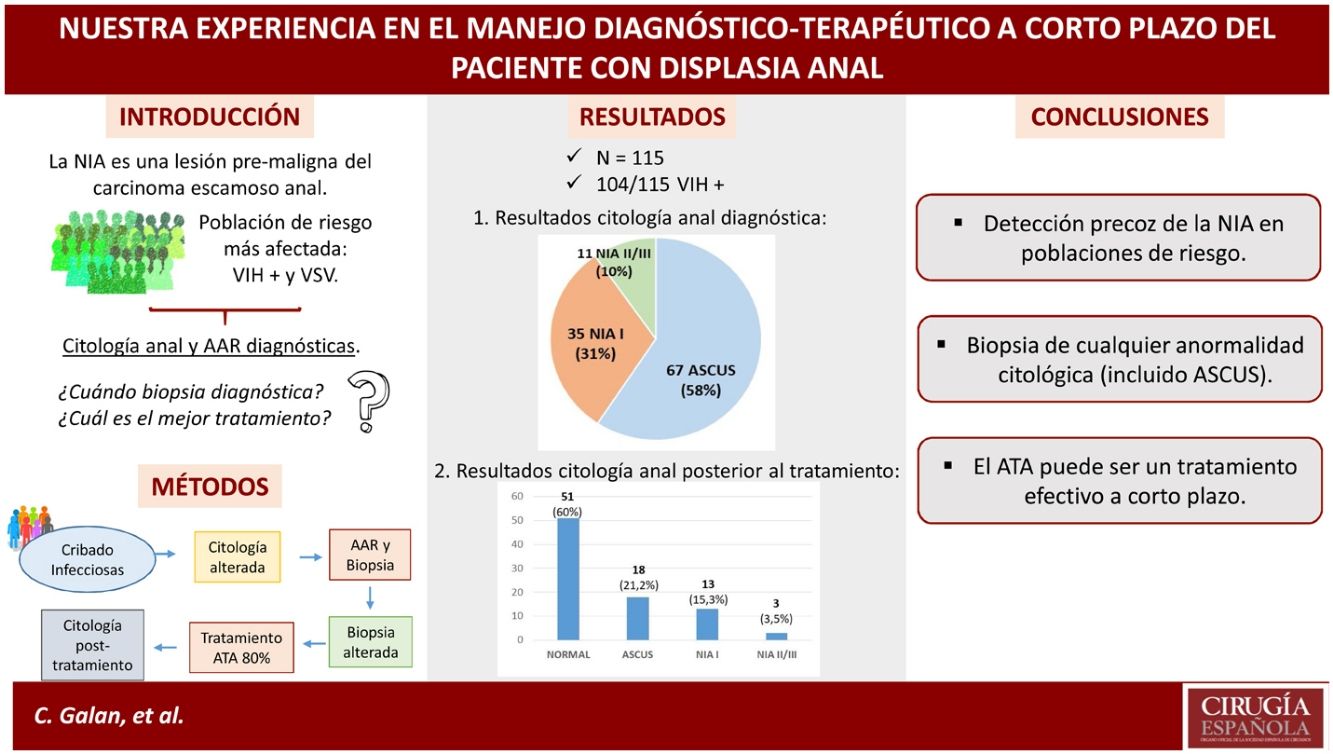
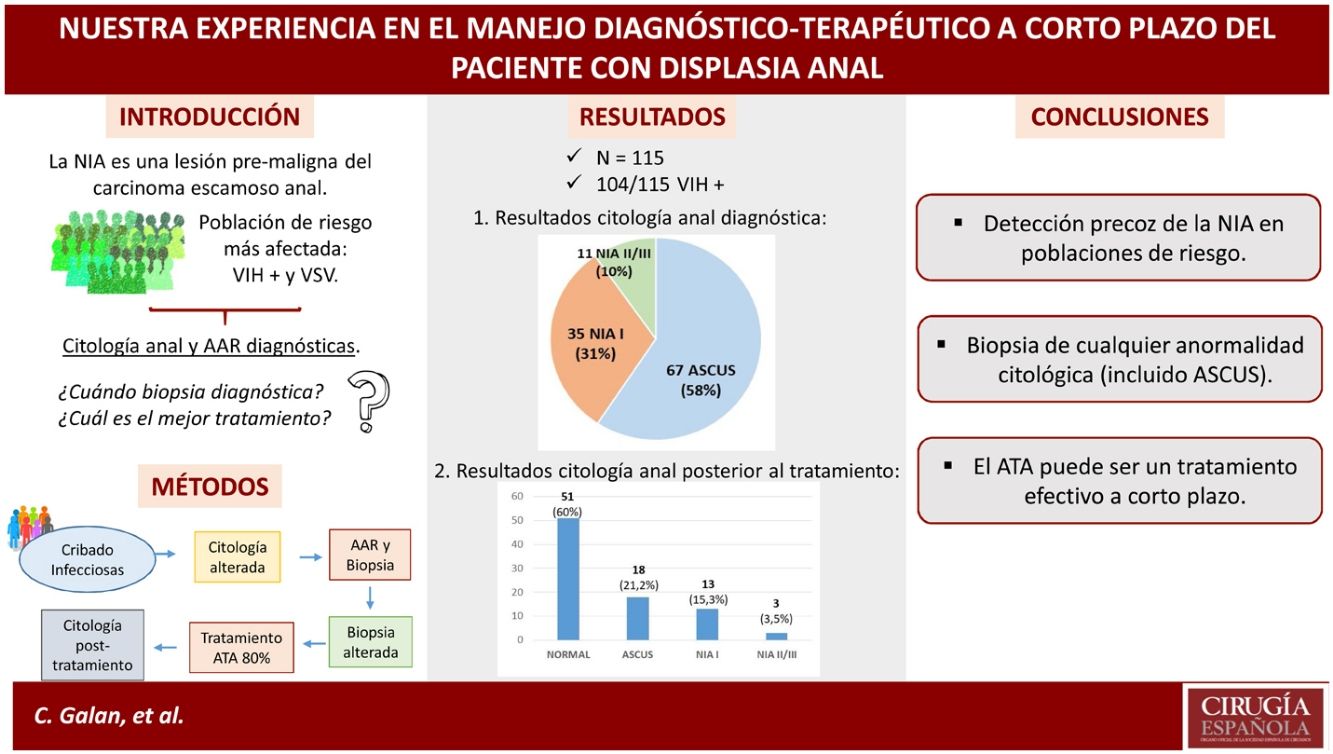
Anal intraepithelial neoplasia (AIN) is a premalignant lesion of anal squamous cell carcinoma. HIV-positive males who have sex with males, are the most affected at-risk population. Cytology and anuscopy are the best accepted methods for its diagnosis, although it is controversial which patients should complete it with a biopsy. Neither which patients should undergo treatment nor which is the best treatment is not well established. With this study, we would like to present our experience in the diagnostic-therapeutic management of AIN in the short term.
MethodsRetrospective observational study of patients at risk of AIN with altered anal cytology who underwent high-resolution anuscopy with biopsy. After histological confirmation of dysplasia, they started treatment with trichloroacetic acid. Its effectiveness was verified by subsequent cytology. The demographic variables of the sample and the results of both diagnostic and treatment tests were analyzed.
ResultsThe majority were HIV-positive males (104/115) and 50% had sexual relations with other men. We included 115 patients with altered anal cytology, of whom 92% had dysplasia on biopsy. 97% with atypia of uncertain significance on cytology had histological dysplasia. Cytology normalized after treatment in 60% of patients.
ConclusionEarly detection of AIN should be routinely considered in known at-risk populations. Any cytological abnormality should be biopsied. Tricholoroacetic acid can be an effective treatment achieving a high percentage of regression, although currently, the information we have is of low level of evidence.
La neoplasia intraepitelial anal (NIA) es una lesión premaligna del carcinoma escamoso anal. Los varones VIH que tienen sexo con varones, es la población de riesgo más afectada. La citología y anuscopia son los métodos mejor aceptados para su diagnóstico, aunque es controvertido qué pacientes deben completarlo con una biopsia. Tampoco está bien establecido qué pacientes deben someterse a tratamiento y cuál es el mejor. Con este estudio, queremos exponer nuestra experiencia en el manejo diagnóstico-terapéutico del NIA a corto plazo.
MétodosEstudio observacional retrospectivo de pacientes con riesgo de NIA con una citología anal alterada a los que se les realizó una anuscopia de alta resolución con biopsia. Tras la confirmación histológica de displasia iniciaron tratamiento con ácido tricloroacético. Se comprobó su efectividad con una citología posterior. Se analizaron las variables demográficas de la muestra y los resultados de las pruebas diagnósticas y de tratamiento.
ResultadosLa mayoría eran varones VIH positivos (104/115) y el 50% mantenían relaciones sexuales con otros varones. Se incluyeron 115 pacientes con citología anal alterada, de los cuales el 92% presentaron displasia en la biopsia. El 97% con atipia de significado incierto en la citología presentaron displasia histológicamente. El 60% de los pacientes normalizó la citología tras el tratamiento.
ConclusiónSe debe considerar de forma sistemática la detección precoz de la NIA en poblaciones de riesgo conocidas. Cualquier anormalidad citológica debe ser biopsiada. El ácido tricloroacético puede ser un tratamiento efectivo consiguiendo un alto porcentaje de regresión, aunque actualmente la información con la que contamos es de bajo nivel de evidencia.
Anal intraepithelial neoplasia (AIN) is a premalignant lesion that can develop into squamous carcinoma.1,2 In the last decade, its incidence has increased by approximately 2% per year,3 and in Spain it is estimated at 0.2 cases/100,000 inhabitants.4
The role of human papillomavirus (HPV) in the pathophysiology of anal squamous cell carcinoma has been demonstrated by the clinical and histopathological evolution it shares with cervical or vulvar intraepithelial neoplasia.2,5 The same virus is implicated in its pathogenesis, type 16 (85% of cases) and type 18.6 The risk of progression to invasive cancer from high-grade AIN within 5 years can be as high as 12%, rates similar to those of the cervix, vulva or vagina.5
Classically, the Bethesda nomenclature was used to describe AIN in three levels: AIN I, II and III. Since 2013, atypia of undetermined significance or ASCUS and AIN I have been standardised and defined as low-grade squamous intraepithelial lesions (L-SIL) and AIN II and AIN III as high-grade squamous intraepithelial lesions (HSIL).5,7
Risk factors associated with the presence of AIN are: men who have sex with men (MSM), immunocompromised patients (HIV, transplant recipients), previous history of ano-genital condylomas and women with cervico-vulvo-vaginal HPV.6
There is controversy about which techniques are the most accepted for the early detection of AIN (isolated anal cytology, oncogenic HPV detection, combination of both, anal biopsy, etc.), as well as treatment, with several therapeutic options currently accepted.
It has been shown that early detection of AIN can prevent its progression to neoplasia in the aforementioned at-risk populations, which justifies the growing interest in the study and treatment of this disease today.
The aim of our study was to evaluate our experience in the short-term diagnostic and therapeutic management of patients with AIN in our hospital.
MethodsStatistical analysisDescriptive observational study of a series of patients with AIN who were diagnosed and treated in our department.
Inclusion criteriaAll patients with an altered anal cytology presenting with a low-grade squamous lesion LSIL (ASCUS or AIN I) or high-grade HSIL (AIN II/III)2 were included.
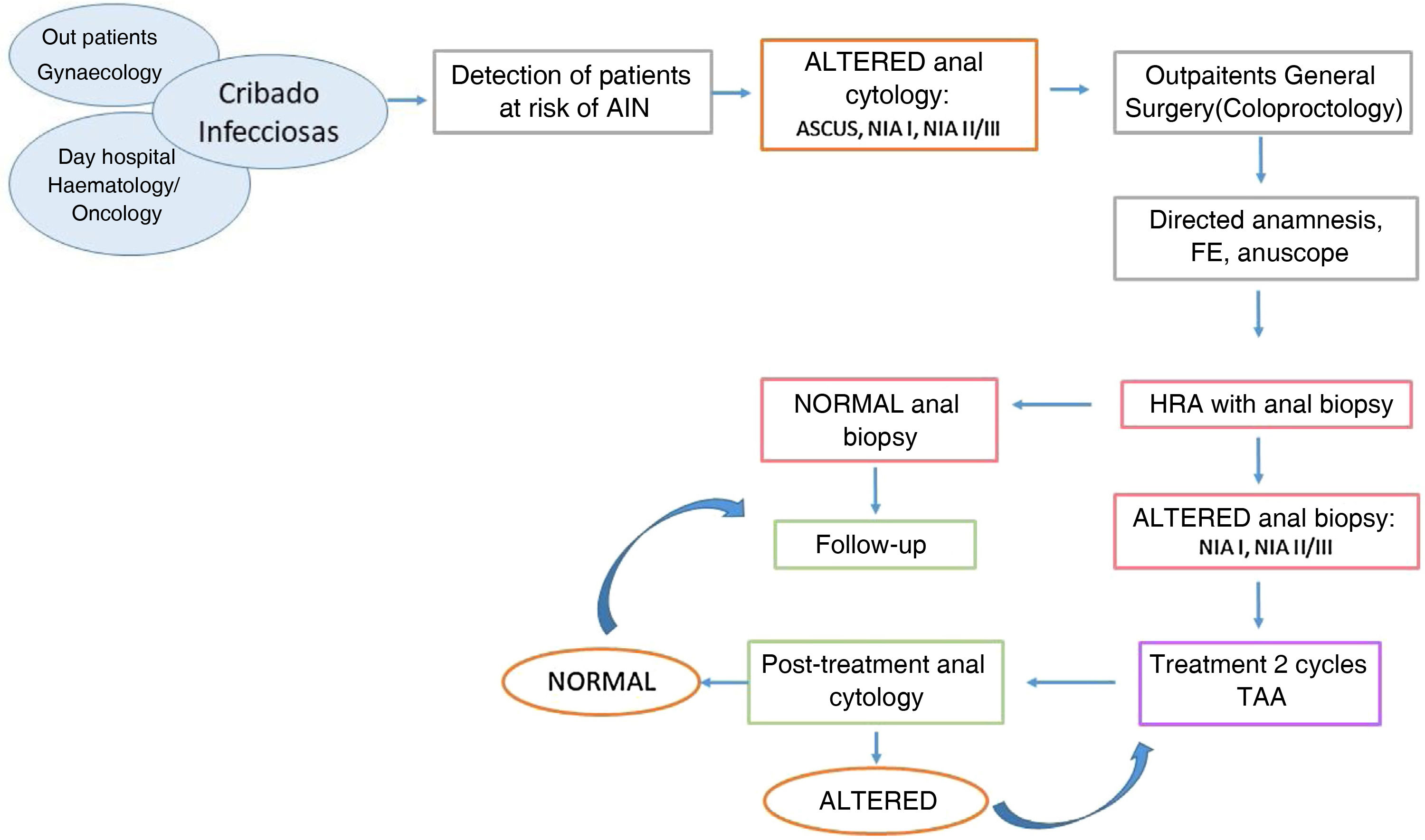
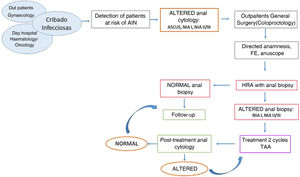
Most of them were HIV-positive men who came from the screening programme of the infectious disease service, which consists of anal cytology every year. Women with difficult-to-screen cervico-vulvo-vaginal HPV had anal cytology performed by the gynaecology service and were referred if the anal cytology was altered. Patients with other immunosuppression (transplant recipients or with haematological diseases) were women with concomitant gynaecological HPV or with dysplasia in samples taken in colonoscopies performed for their underlying disease. Once referred to our unit, a standardised diagnostic-therapeutic protocol of the AIN was applied (Fig. 1).
A physical examination by digital rectal examination and high-resolution anuscopy (HRA) with biopsy was performed in our consultations, placing the patient in lateral decubitus for the procedure. During the HRA we performed a 5% acetic acid impregnation of the anal epithelium under direct visualisation. We then applied lugol to reveal those non-catching "acetowhite" lesions that are likely to be preneoplastic (Shiller test).8 These lesions were biopsied using rectal biopsy forceps, as well as any other lesion suggestive of malignancy.
At the discretion of the pathology department, HPV genotype was determined on cytology and biopsy in some patients, but not in a standardised manner.
Patients in whom histology confirmed anal dysplasia were proposed for treatment, which consisted of the topical application of two cycles of trichloroacetic acid (80% TAA) in two sessions separated by 30 days. A swab soaked in TAA was used to contact the entire circumference of the anal mucosa for 30 s after topical application of local anaesthetic.
The effectiveness of the treatment was assessed by anal cytology performed 30–60 days after the second course of treatment. Patients with complete regression after treatment were followed up by infectious disease service screening. If cytological alteration persisted after treatment, they underwent 2 more rounds of 80% TAA (Fig. 1).
ResultsDemographic analysisBetween January-2018 and February-2020, a series of 115 patients presenting with abnormal anal cytology were seen: 106 men and 9 women, with a mean age of 42.5 years (19–65).
The distribution according to associated risk factors was: 104 patients were HIV-positive, of whom 57 were MSM; 7 patients had other types of immunosuppression (solid organ transplantation or rheumatological/haematological diseases/ID) and 5 patients had no immunosuppression (4 men with homosexual risk contact and 1 woman with condylomas).
In the subgroup of women (9), 3 were HIV-positive, 3 were transplant recipients and one had NHL undergoing chemotherapy. Six of the women had concomitant cervical-vaginal HPV. Two of them were vaccinated against HPV (Table 1).
Summary of the demographic characteristics of the series.
| Number (n) | Percentagee (%) | |
|---|---|---|
| Total sample | 115 | 100 |
| Men | 106 | 92.2 |
| Women | 9 | 7.8 |
| HIV infection | 104 | 90.4 |
| MSM | 57 | 49.6 |
| Solid organ transplants | 3 | 2.6 |
| Other immunosuppressionsa | 4 | 3.5 |
| Women with concomitant gynaecological HPV | 6 | 5.2 |
| Immunocompetent | 5 | 4.4 |
HIV, Human Immunodeficiency Virus; IBD, Inflammatory bowel disease; MSM, Men who have sex with men.
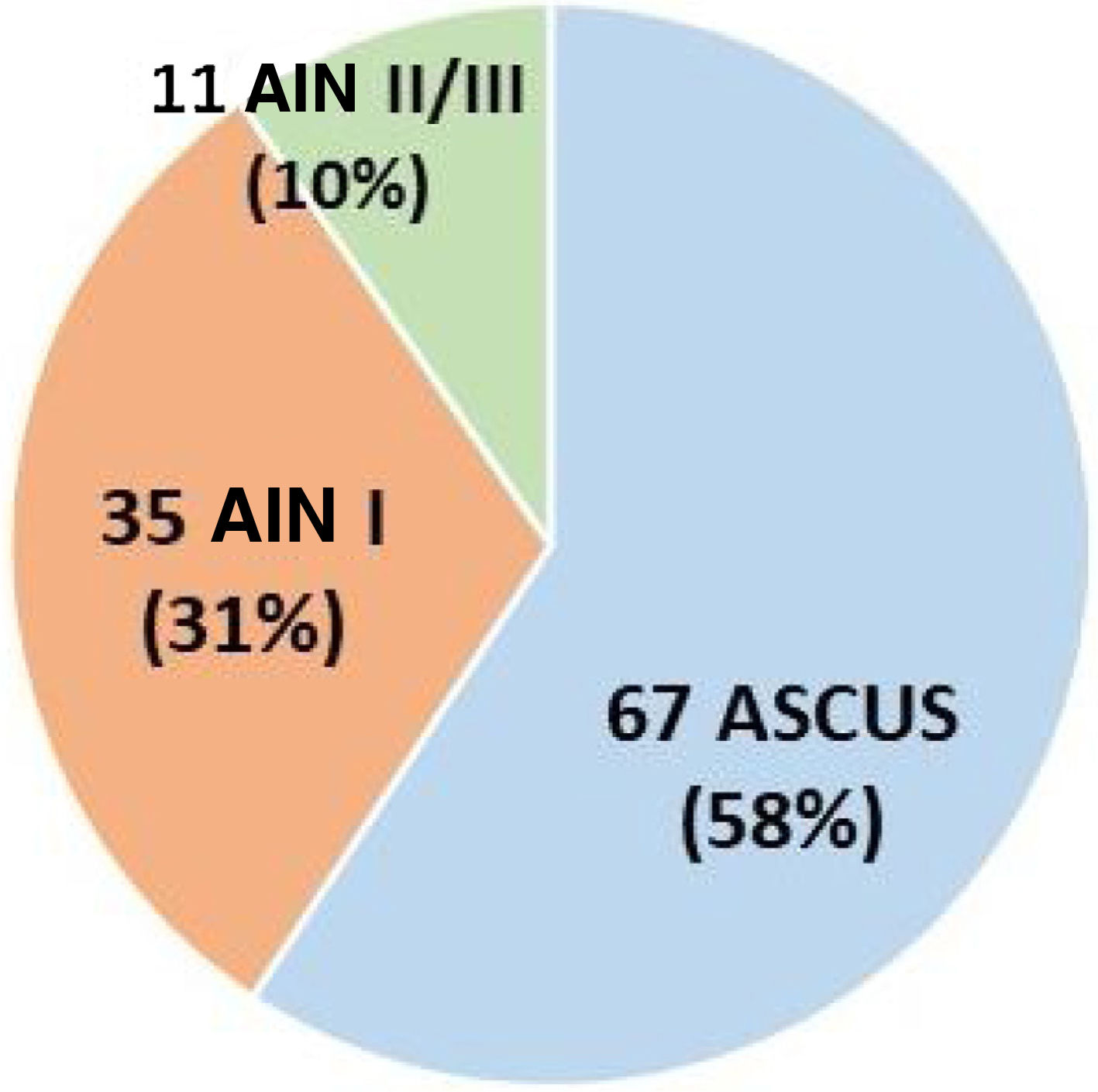
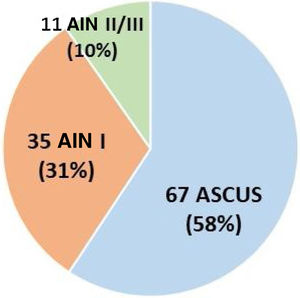
Of the 115 patients, 2 were diagnosed by biopsy with no previous cytology, and 113 presented with an altered anal cytology. Of these 67 presented with atypia of undetermined significance/ASCUS (58%), 35 AIN I (31%) and 11 AIN II/III (10%) (Fig. 2).
BiopsyOf the 115 patients, 112 patients were biopsied after an altered initial cytology, as 2 patients had biopsy without previous cytology and one patient started treatment directly after cytology without biopsy. Of the biopsied patients (112): 9 had a normal biopsy (8%), 55 (49%) had an AIN I result and 48 (43%) had an AIN II/III result.
Of the patients with altered initial cytology, 92% had biopsy-confirmed dysplasia (103/112). Notably, of 66 patients with ASCUS on cytology, 64 (97%) had dysplasia histologically.
Seven out of 9 patients with normal biopsy results had a previous cytological finding of AIN I. Patients with normal biopsy were not treated and continued to be followed up with regular annual cytology. Of 48 patients with severe dysplasia on biopsy, 9 had previous HSIL on cytology (Table 2).
Relationship between the cytology results and the diagnostic anal biopsy.
| Anal biopsy results | ||||
|---|---|---|---|---|
| Normal | AIN I | AIN II/III | Total | |
| Anal cytology results | ||||
| ASCUS | 2 | 32 | 32 | 66 |
| AIN I | 7 | 21 | 7 | 35 |
| AIN II/III | 0 | 2 | 9 | 11 |
| Total | 9 | 55 | 48 | 112 |
Of the 115 patients in the total sample: 112 had cytology and anal biopsy (2 patients had biopsy without cytology and one patient had cytology without biopsy).
HPV 16 genotype was tested on initial cytology in 93 patients, being positive in 31 (33%) and on biopsy in 45 patients, being positive in 6 (13%). Five of these 6 had ASCUS on cytology.
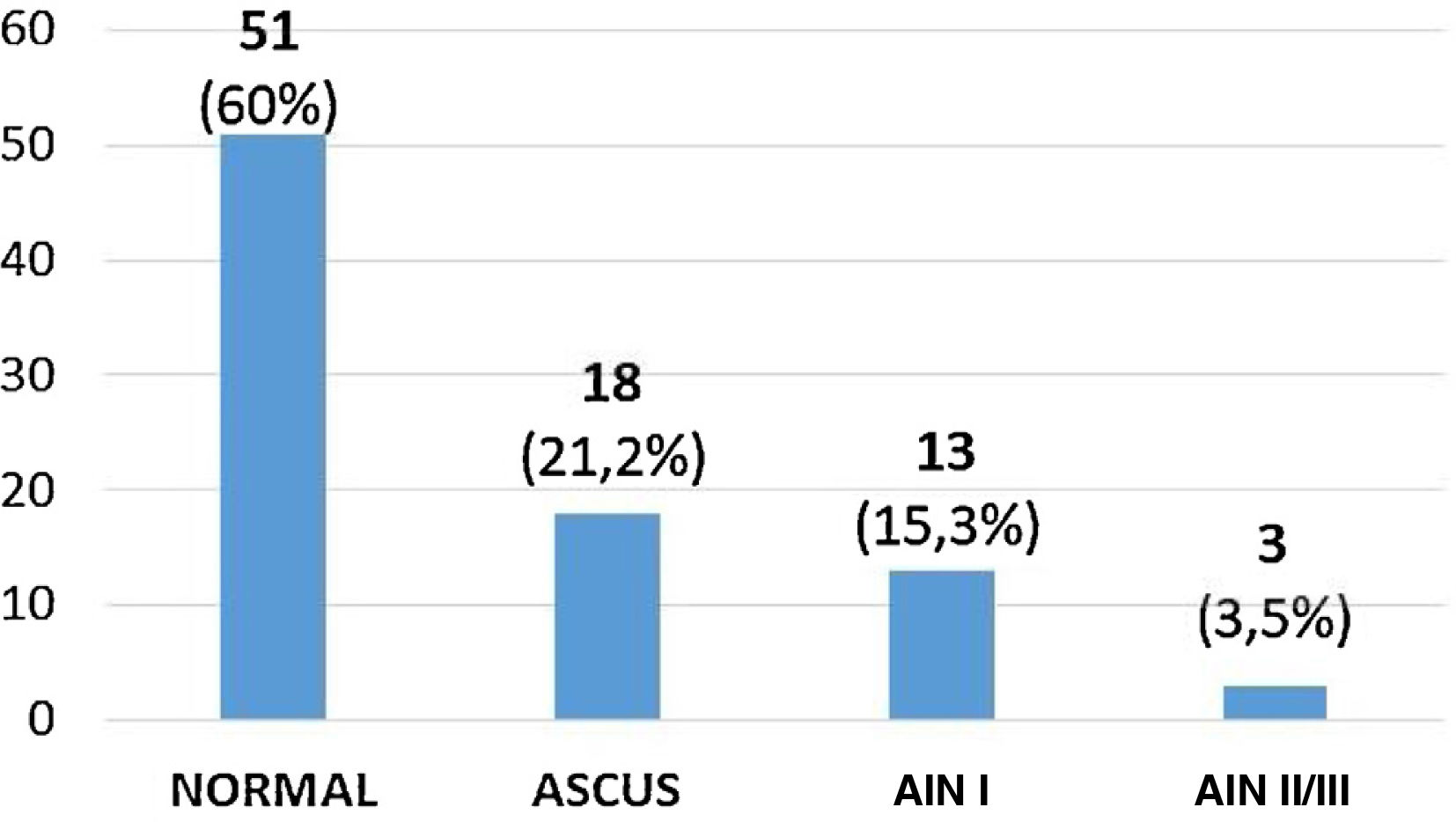
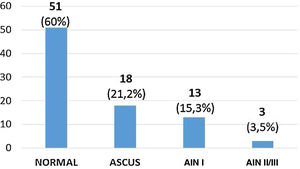
Treatment analysisNinety-eight patients completed 2 cycles of TAA at the time of the study. Of these we have control in 85 patients with cytology, which normalised in 51 patients (60%), 18 (21.2%) had ASCUS, 13 (15.3%) AIN I and 3 (3.5%) AIN II/III (Fig. 3). According to these results, treatment was effective in 60% of cases (Table 3).
Those patients with persistent cytological alteration post-treatment (34) underwent 2 more rounds of 80% TAA, followed by a further control cytology. We do not currently have the results of the latter cytology because the procedure times are very long, so we cannot show the results of the follow-up of this group of patients in this study.
Of the 51 patients with normal cytology after treatment, 27 patients underwent a repeat cytology after one year by the infectious diseases service as part of their regular screening. Of these 27 patients: 18 had persistently normal cytology and 9 had ASCUS. In conclusion, 18/27 (66%) of patients with complete regression after treatment and who continued to be followed up, have had no recurrence of dysplasia to date.
DiscussionThere has been an increase in the incidence of anal squamous cell carcinoma in recent decades in certain at-risk populations such as HIV-positive patients.9,10 AIN is now considered to be a pre-neoplastic lesion that may progress to anal cancer, so interest in early detection has increased, with surveillance systems being stepped up in known at-risk populations and being considered in other populations with risk factors that are not yet well defined. In our series, most of the patients (104/115) had HIV, and at the time of the study 57 of them were known to be HIV-positive (49% of the total), although the type of sexual behaviour of the entire sample had not been asked, so this percentage is probably higher, as described in the literature.
Our study also included patients who had received a transplant or corticosteroid/chemotherapy treatment. The prevalence of AIN in a transplant patient can be as high as 40%.5 Larsen et al. evaluated the prevalence of anal HSIL in renal transplant recipients compared to immunocompetent patients, finding a higher risk of HSIL and anal cancer in the latter, and detecting the presence of genital condylomas and homosexual practices as risk factors.11 The three transplant recipients in our series had anal HPV that was difficult to control, requiring several lines of treatment.
In women, coexisting cervical HPV infection increases the risk of AIN, regardless of whether they also have HIV.5,12 Wohlmuth et al. recently established that women over 40 years of age with gynaecological HPV have high rates of AIN, and that advanced age and smoking are considered significant risk factors for developing anal cytology abnormalities.13 In our sample, 6 women had concomitant cervico-vaginal HPV.
The demographic analysis of our population suggests the need to include other populations considered at risk in the early detection of AIN in a more accurate and standardised manner.
Regarding the diagnosis of anal dysplasia, there is insufficient evidence that has demonstrated which is the best screening method at present, but physical examination with anuscopy and cytology are considered the "gold standard". Combining several diagnostic methods can reduce the false negative and false positive rate and bring us closer to a more accurate diagnosis.
Cytology is a non-invasive method in the diagnosis of AIN. It has a higher sensitivity (70%–95%) than specificity (40%–50%), so a significant proportion of specimens diagnosed with LSIL will subsequently present with AIN II/III on histological diagnosis. According to these data, any cytological abnormality should be completed with an HRA and biopsy.2,5
In our study, 92% of patients with altered cytology had dysplasia on diagnostic biopsy, and 97% of patients with atypia of uncertain significance/ASCUS on cytology had histologically confirmed dysplasia (half of these, high-grade dysplasia). These data support the need to complete the diagnosis of any abnormal cytology with a biopsy, given that the rate of dysplasia per biopsy in patients with ASCUS on cytology is not negligible in our series (64/66). Currently, there is disagreement about what to do with a cytological result of ASCUS, with follow-up only in many centres. In our opinion, patients with an altered anal cytology including ASCUS require a biopsy and more exhaustive follow-up.
HPV genotyping has recently been established as a more sensitive and specific diagnostic method than cytology for the diagnosis of anal dysplasia. This is demonstrated by a retrospective cohort study of 84 patients with risk factors for AIN (half HIV-positive), in whom genotyping identified 17 cases (22%) of severe dysplasia that had been under-diagnosed on cytology, concluding that HPV screening can complement cytology and help identify patients at higher risk of developing high-grade anal dysplasia.10 It is in cervical cancer that there is most experience with the usefulness of virus genotyping. Four European randomised trials demonstrated that HPV screening can provide up to 60–70% greater protection against invasive cervical carcinoma in women compared to cytology.5
In our study, 33% of patients with altered cytology were positive for HPV 16, most with an ASCUS result. Given that almost half of the patients with ASCUS had high-grade dysplasia on subsequent biopsy, we believe that HPV genotyping is a cost-effective tool in the initial diagnosis of AIN, and can help us identify which patients should be biopsied if they have high-risk genotypes.
HRA with biopsy is still considered an essential diagnostic procedure, either alone or in association with cytology and/or HPV genotyping, as it allows histological confirmation of dysplasia.14. The main disadvantage is that not all centres have it, and it requires expert staff to perform it.
Currently, the treatment of AIN is highly controversial for several reasons: (a) there is no consensus on which patients should be monitored without treatment; (b) what is the ideal treatment; and (c) which treatment option has demonstrated the highest complete regression rates. Multiple treatments have been used, ranging from ablative techniques such as CO2 laser, electrocautery, infrared, cryotherapy to application of topical agents such as trichloroacetic acid, 5-fluorouracil or imiquimod. All are associated with variable morbidity due to mild side effects such as pain, bleeding, itching or more significant effects such as stenosis or faecal incontinence.2
A recent systematic review (2020) analysing current treatment modalities identified several treatments capable of inducing AIN regression, however, recurrence rates were high and assessment of long-term efficacy was limited by short follow-up periods.15 The results of studies comparing ablative therapies and topical agents are highly variable.
Regarding trichloroacetic acid, Singh et al. (2009) conducted a retrospective study in 35 HIV-positive and 19 HIV-negative MSM who underwent treatment with 85% TAA. Of 28 patients with high-grade dysplasia, 32% regressed completely and 29% regressed to low-grade dysplasia. Low-grade lesions were completely eliminated in 73% of cases;15 Cranston et al. (2014) evaluated the efficacy of 80% TAA treatment in HIV-positive men with high-grade AIN with a 72% complete response rate, 11% partial response and 15% recurrence at 3–6 months.16
TAA is a corrosive agent with mild side effects and low cost. Its application is entirely hospital-based, so it offers greater reliability in terms of patient compliance with treatment. In our centre, we used 2 cycles of TAA, which was effective in more than half of the patients who underwent treatment, given that 60% had normalised cytology after treatment. Of the patients who experienced complete regression (51), 24 had high-grade dysplasia on previous biopsy (47%) and 27 had low-grade dysplasia (53%).
Comparing our results with the aforementioned studies, our sample showed a higher percentage of regression after treatment in patients with high-grade dysplasia than the Sing et al. series (47 vs. 32%), but lower than Cranston et al. However, our regression rate in patients with low-grade dysplasia was lower than the Sing et al. series (53 vs. 73%). TAA is our treatment of choice, although the results in the literature regarding its effectiveness are variable and there is insufficient evidence on its long-term preventive effects.
In our study, we are aware of the results of subsequent follow-up of patients with normalisation of cytology after treatment in a very small number of patients (27), so the percentage of persistent regression one year after treatment (66%) should be interpreted with caution. The limitations of our analysis are those of a retrospective descriptive study, with a small population and a short follow-up of patients.
From our experience we would like to conclude: (a) the need to standardise those high-risk populations that would benefit from anal dysplasia screening; (b) the importance of biopsying any abnormality in anal cytology, and (c) to consider TAA as an effective treatment that achieves high rates of regression in the short term. However, studies with larger sample sizes and longer follow-ups are needed to agree on the correct diagnostic-therapeutic management in patients at high risk of AIN and to demonstrate that inducing AIN regression can reduce the risk of developing anal squamous cell carcinoma.
Conflict of interestsThe authors have no conflict of interests to declare.