Mammary-like glands (MLG) are present in the skin of the anogenital region of women and men. Like normal breast tissue, they have the potential for degeneration and malignancy, and neoplasms have been described in this location, although very rarely. Due to their low incidence and anomalous distribution, these neoplasms pose a diagnostic challenge and are usually an incidental finding, whose management is not widely defined or standardized.
We present the case of a 64-year-old woman, active smoker, with no other history of interest. During a routine examination, a perianal lesion was observed that had been progressing for 30 years, which was removed under local anesthesia. The pathological study reported microinvasive ductal carcinoma (<1 mm) of the mammary type located on the mammary-like anogenital gland, with focal extension to the resection margin. Sieve-like formations and foci of comedo necrosis were described, as well as pagetoid extension (Fig. 1). The immunohistochemical study reflected positivity of the intraepidermal cells for cytokeratin 7, CEA, and GATA3. The tumor cells expressed GATA 3, GCDFR-15, E-Cadherin and, in a focal manner, estrogen and progesterone receptors. Likewise, positivity was shown for cytokeratin 19, and the Neu-Her 2 study was negative. Mucoproduction was not observed.
Images from the pathological study: A) Ductal carcinoma in situ associated with epidermis with sieve-like formation and comedo necrosis (hematoxylin-eosin [H-E] ×2); B) Ductal carcinoma in situ with presence of pagetoid extension (H-E, ×20); C) Positive immunostaining for CK20 (×10); D) Positive immunostaining for CK7 (×4); E) Positive immunostaining for estrogen receptor (×10); F) Positive immunostaining for progesterone receptor (×20).
Subsequently, the resection margins were expanded, and the pathological study results were negative.
In addition, a complete physical examination of the patient was conducted, finding no lesions in either breast or inguinal lymphadenopathies. Lastly, the study was completed with PET, mammography and breast MRI, as well as a tumor marker analysis. All the extension studies were negative, which ruled out lymphadenectomy.
We presented the case to the multidisciplinary tumor committee, at which time it was decided to complete follow-up tests with tumor markers CEA, CA 15.3, as well as pelvic magnetic resonance imaging.
Mammary-like glands are present in the skin of the anogenital region of women and men. For many years, they had been considered ectopic breast tissue, derived from the embryological remains of the involution of the mammary ridge or crest.1 MLD are distributed through the anus and perianal region, interlabial sulci and around the clitoris in females, and the ventral side of the penis in males.
Recently, the distinction between both structures, ectopic breast tissue and MLG, has been clearly established, as the location of the latter is more medial and close to the vulvar labia minora, finding a smaller number of glands and presenting a simpler configuration.2 In addition, its ultrastructure differs from sweat glands in showing positivity for estrogens and progesterone.3
These MLG glands are subject to the degenerative and dysplastic changes present in the normal mammary parenchyma, so that the lesions that derive from them, whether benign or malignant, have a surprising similarity to their mammary counterparts,4 and evolution to malignant disease is extremely rare.5
MLG tumors are exceptionally rare entities. The fact that, in the literature, many of these neoplasms have been erroneously described as, originating from ectopic breast tissue also generates a lack of a standardized definition, categorization. Given their low prevalence, there is no consensus on the diagnosis, treatment, or follow-up protocols for these patients. However, since histology confirms a behavior similar to that of primary breast neoplasms, many authors advocate management similar to these tumors6 although this point remains controversial. Other studies defend individualization, recommend management similar to that of primary lesions for perineal, vulvar locations, including resection, lymphadenectomy, if appropriate.7
Correct classification of these neoplasms, greater agreement in the diagnostic process, and therapeutic alternatives could provide significant advantages for patients affected by this type of tumors which, although uncommon, are diagnosed as advanced disease due to the lack of suspicion.






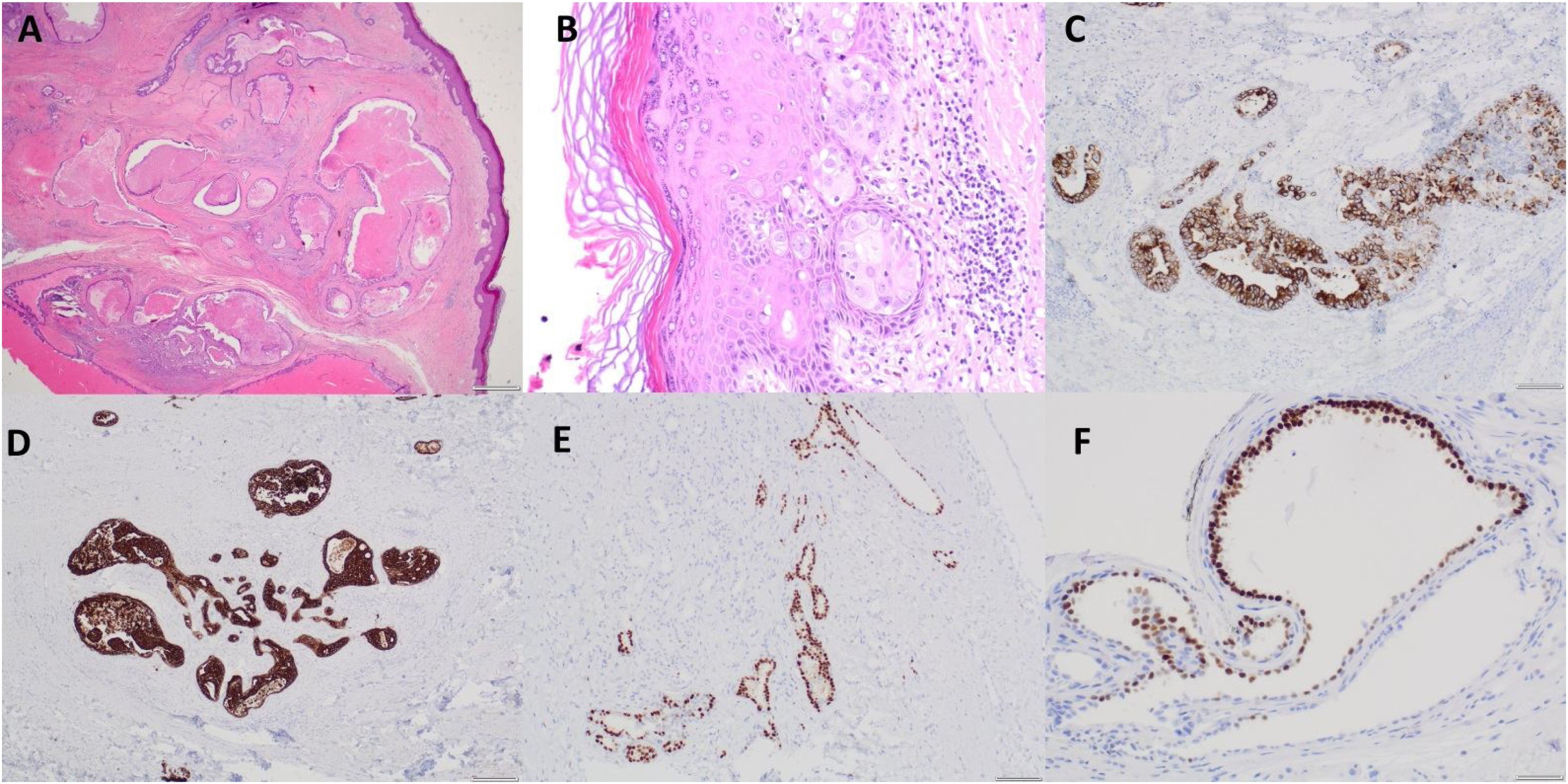
![Images from the pathological study: A) Ductal carcinoma in situ associated with epidermis with sieve-like formation and comedo necrosis (hematoxylin-eosin [H-E] ×2); B) Ductal carcinoma in situ with presence of pagetoid extension (H-E, ×20); C) Positive immunostaining for CK20 (×10); D) Positive immunostaining for CK7 (×4); E) Positive immunostaining for estrogen receptor (×10); F) Positive immunostaining for progesterone receptor (×20). Images from the pathological study: A) Ductal carcinoma in situ associated with epidermis with sieve-like formation and comedo necrosis (hematoxylin-eosin [H-E] ×2); B) Ductal carcinoma in situ with presence of pagetoid extension (H-E, ×20); C) Positive immunostaining for CK20 (×10); D) Positive immunostaining for CK7 (×4); E) Positive immunostaining for estrogen receptor (×10); F) Positive immunostaining for progesterone receptor (×20).](https://static.elsevier.es/multimedia/21735077/0000010100000001/v1_202301110859/S2173507722002307/v1_202301110859/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
