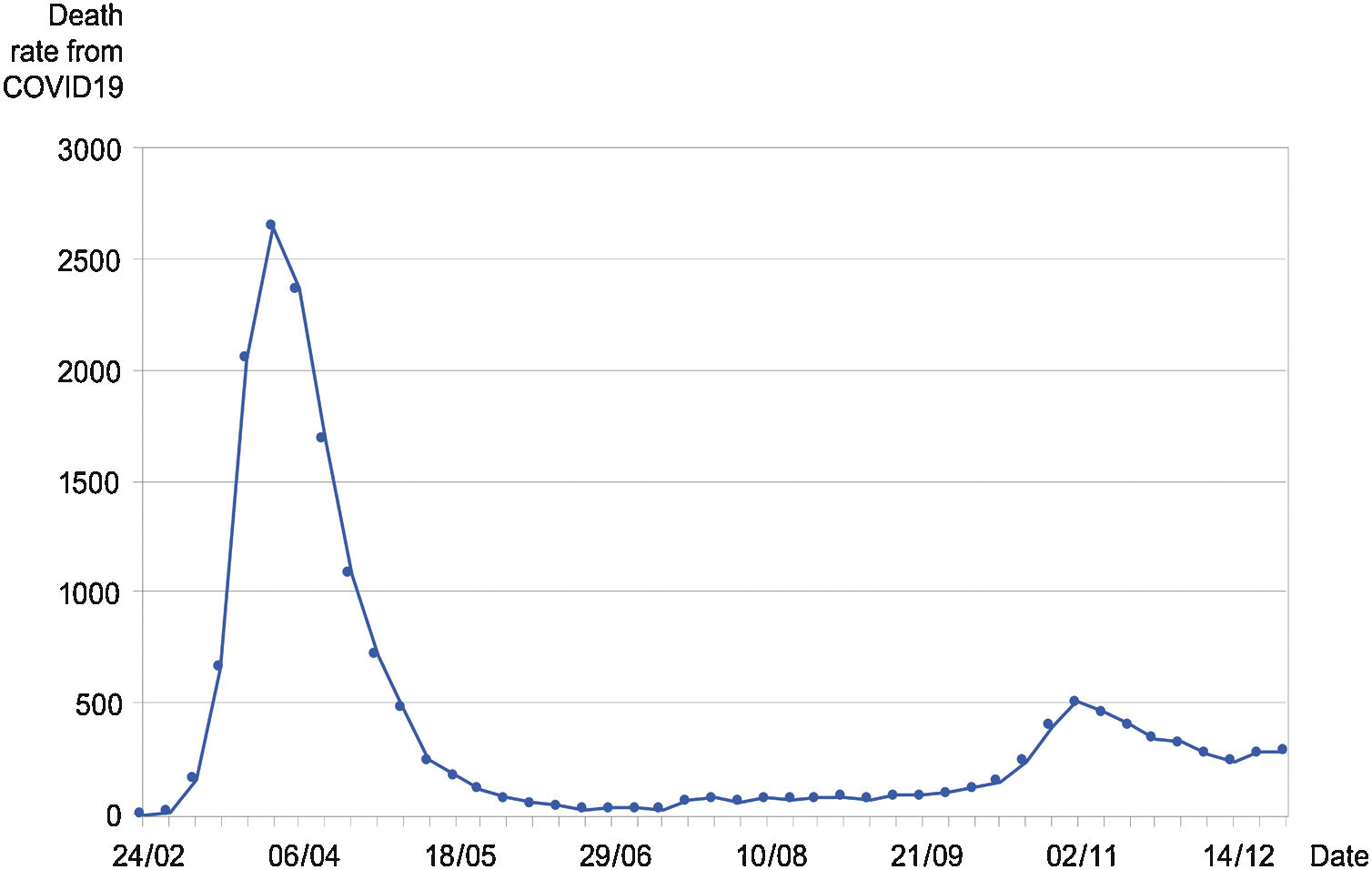
The pillars of Breast cancer (BC) care in Catalonia are a well established population screening programme (PSP), as well as an optimal performance of the Breast Units that harmonize the relative contribution from the involved departments. As of mid March 2020, covid pandemic was hitting hard on the catalan population (7.7 million), and a complete lockdown was decreed by the spanish government on March 14 (Fig. 1).1 At this stage, most public hospitals and primary care centres were being strongly devoted to covid-19 patient care in the region, while a great deal of the usual non-covid health assistance was being put on hold.2 Thus, our PSP was halted from March 16,2020 to May 18, 2020. In the present investigation we aimed to ascertain the actual impact of such a deprived time on the care of patients with a new or recent diagnosis of BC, especially focusing on the initial diagnostic procedures, and surgery.
This study was restricted to two public university hospitals of Terrassa (Barcelona). The overall population in the joined catchment area exceeds 400.000 inhabitants.The shared local PSP was established in 2000, and had been operating uneventfully until March 2020. During the previous five years, there had been a stable rate of newly diagnosed cases BC emerging from the same demographic base, at a mean rate of 350 new cases per year.
Patient culling was achieved by screening the breast committee reports, as well as the pathology database for core-biopsy results positive for BC. From March 15, 2020 until September 30, 2020 (study period), subjects were registered in this study following one of these criteria: first outpatient visit with a new BC diagnosis, primary surgical procedure for BC, post-neoadjuvant surgical procedure for BC, or had been put on a neoadjuvant chemotherapy regime. We excluded patients with a BC diagnosis or treatment outside the study period, as well as elderly patients unfit for conventional treatment, and patients with stage IV disease at onset.
The study period was selected in order to accommodate the first covid-19 outbreak and short of the second outbreak, occurring in October 2020, such that any significant change in this patient series, as compared with the control series one year previously, would reflect the short term effects of the first outbreak on BC care.
Variable results from the study were compared with the corresponding results from a control group of patients, from March 15, 2019 until September 30, 2019.
Overall, 104 patients were registered into the 2020 study group. This compares with 171 patients in the 2019 control group, for a decrease of 39,2% in BC care activity. The corresponding figures for new BC cases were 73 and 127 patients respectively, for a decrease of 41.7%. The 2019 count of BC cases in the control period was not a far cry from the expected half-year count. The rate of decrease in the 2020 BC care activity was most dramatic during the first eight weeks, then leveling off by the 28th week, although no clear recovery was evident by that time yet.
The Table1 shows a comparative analysis of the relevant variables between the study and control subjects.
Comparative analysis of the relevant variables between the study and control breast cancer patients group.
| Control group-2019 | Study group-2020 | P value | |
|---|---|---|---|
| N = 171 | N = 104 | ||
| Patient Age – mean ± SD | 58 ± 13 | 60 ± 14 | .486 |
| First degree family history of BC: yes/no | 30/85 | 81/73 | .001 |
| Study entry: First visit | 127 | 73 | .343 |
| Surgery | 15 | 11 | |
| Post-chemotherapy surgery | 23 | 16 | |
| Primary chemotherapy | 5 | 4 | |
| Diagnosis: BC clinical | 124 | 78 | .380 |
| Screening programme | 47 | 26 | |
| Biopsy diagnosis | .022 | ||
| DCIS | 27 | 7 | |
| Invasive carcinoma | 144 | 95 | |
| T Stage: T1 | 74 | 43 | .384 |
| T2 | 67 | 41 | |
| T3 | 10 | 10 | |
| Preoperative nodal stage | 0.217 | ||
| Negative | 86 | 59 | |
| Positive | 67 | 36 | |
| Clinical stage: 0 | 26 | 7 | .842 |
| I | 58 | 35 | |
| IIA | 48 | 30 | |
| IIB | 23 | 15 | |
| III | 10 | 14 | |
| Phenotype: Luminal A | 64 | 25 | .061 |
| Luminal B | 64 | 41 | |
| Her2 + | 13 | 15 | |
| Triple negative | 19 | 15 | |
| Surgical procedure | 0.416 | ||
| Mastectomy | 43 | 21 | |
| Conservative | 128 | 70 |
BC, Breast cancer.
The ominous covid-19 pandemic is bound to have profound effects on many aspects of Health Care worldwide. Due to its high prevalence in the western world, BC is of much concern under the present circumstances.3 Early BC diagnosis together with the improved women’s awareness of the disease has led to a marked improvement of prognosis, with a present survival rate of 84% at 5 years.4 In order to meet these goals, a well-built armamentarium has been deployed, including PSP, and an enhanced use of ultrasound scans (US), Magnetic Resonance Imaging (MRI), Core-needle biopsy, ever more conservative surgical procedures, improved radiation therapy, and updated systemic therapy. Much of such mindset and deployed resources seem at jeopardy during an initial covid-19 outbreak. Potential BC patients may refrain from consultation in the first place under the belief that hospitals are a source of infection.5 The results from our investigation points to a drop of about 39% in overall BC care activity and about 42% in newly diagnosed cases. In general, the lack of significant differences between the study and control groups suggests that patients attending our hospitals during and shortly after the first outbreak did not have a more advanced disease stage, as perhaps one might have expected. A significant decrease of DCIS rate during the study period seems clearly related to the halting of our PSP for several weeks. More difficult to explain is the higher rate of a family history of BC among study patients. Having first degree relatives with BC may have prompted them to seek medical care. Regarding BC patients actually being cared for, there seems not to have been any significant delay in diagnosis or treatment in the short term. However, more intriguing and perhaps worrying is the lack of information concerning those patients that went missing during the initial outbreak, lasting until late May (Fig. 1), who had not shown-up significantly by the end of September 2020, just prior to the second outbreak.