Major chest wall defects that remain after resection of a tumor involving the sternum and/or ribs are associated with some morbidity and mortality and are, in many cases, a great challenge for the surgeon. Mansour et al. reported an overall mortality of 7%, with a pneumonia rate of 24% and a general hospital stay of 18±16 days following reconstruction of the chest wall with a mesh.1
Different prosthetic materials are described in the literature for chest wall reconstruction and thoracic surgeons’ decision about what materials to use and how to reconstruct chest wall and sternal defects must take into account the patient's age, extent of resection, defect size, and presence of infection or prior radiation.2 The main objective of every surgeon is to obtain a prosthesis or material that is malleable to suit the shape of the chest wall and flexible enough to allow breathing excursions, biologically inert, which allows internal tissue growth and is also esthetically acceptable.3 It is also important to consider that, regardless of the technique used to establish skeletal stability, ensuring total tissue coverage of the prosthesis is always necessary, especially in oncological surgery. This can be achieved by direct closure, skin grafts, local advancement flaps, pedunculated myocutaneous flaps, or free flaps.3
The invention of 3D printing techniques with the ability to produce exact titanium-based copies of virtually any bone has led to another era in reconstructive surgery.4
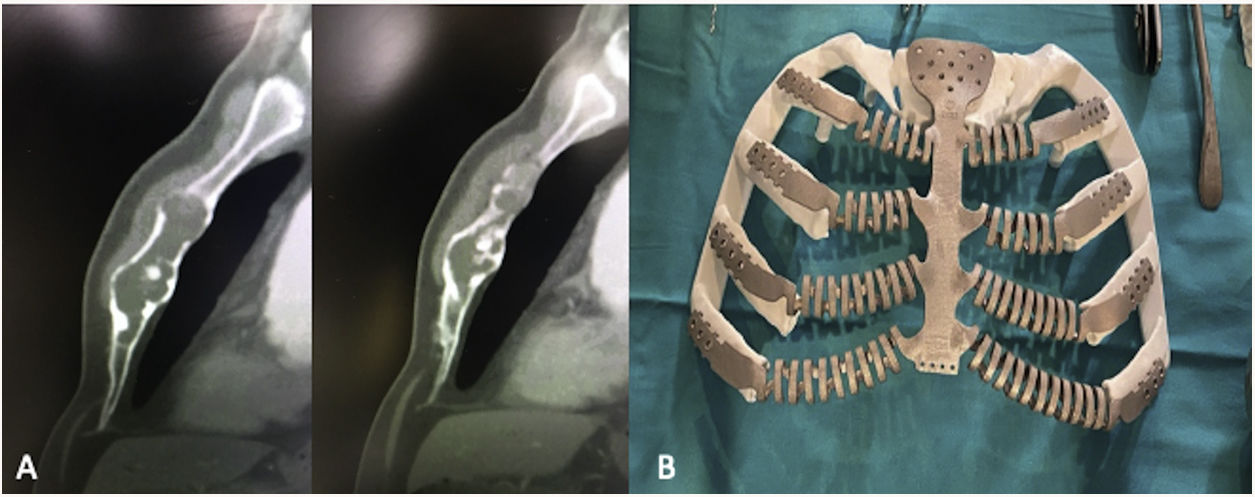
A 61-year-old male patient attended the consultation complaining of pain and a feeling of instability in the anterior chest wall associated with respiratory distress, which limited his active lifestyle. The patient was an athlete and a hard worker, a former smoker, and had no history of previous oncological disease. On physical examination, unevenness was palpable on the surface of the entire body of the sternum. A high resolution chest tomography showed an osteolytic lesion with sclerotic edges, small areas of cortical rupture, and no invasion of adjacent soft tissue parts, which generated insufflation of the sternal body (Fig. 1).
We decided to remove the sternal body and the corresponding costal cartilages, and to carry out the reconstruction with a titanium prosthesis. Raomed Co. (Cordoba, Argentina) designed and created a 3D printed titanium implant based on the patient's CT images, which consisted of a fixation base with screws in the sternal manubrium and flexible lateral spiral-shaped extensions simulating the costal cartilages which have a distal end with fitting holes that can adapt to the costal surfaces. The prosthesis was designed taking into consideration safe resection margins and perfect adaptability (Fig. 1).
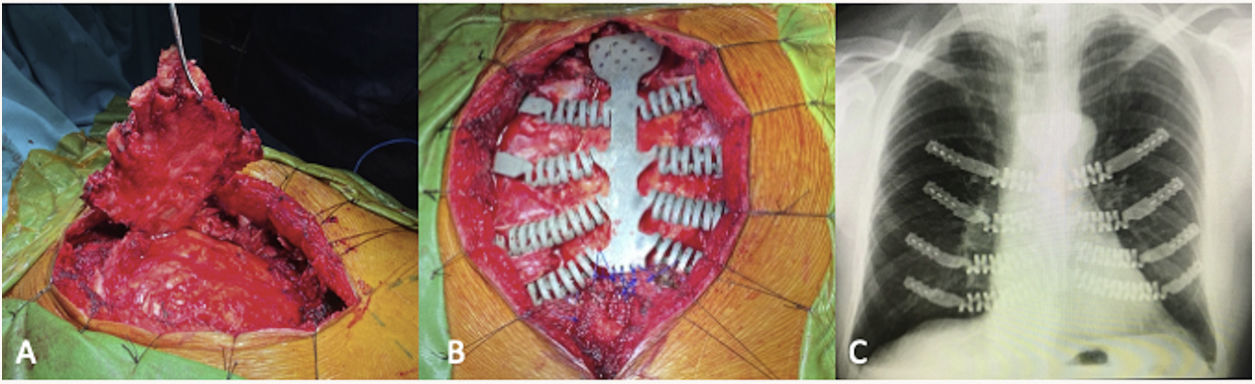
The surgery started with the mobilization of the pectoralis major and minor muscles, which were then used to cover the prosthesis. This was followed by identification of the limits of the osteocartilaginous lesion and lateral dissection until reaching healthy ribs for the implantation of the prosthesis. After that, the sternum was resected along with the costal cartilages, maintaining the perichondrium (Fig. 2).
The 3D-printed titanium sternal prosthesis was placed and fixed into position starting with the upper segment in the sternal manubrium. Then, the lateral extensions of the lateral ends were attached to the rib surfaces on both sides, fixing and blocking them with self-drilling screws in order to provide a firm fixation. The lower extremity was fixed by prolene suture to the xiphoid process and adjacent muscles. The previously mobilized pectoral flaps were then joined in the midline, ensuring total and vascular coverage of the implant (Fig. 2).
The postoperative period was uneventful and the patient was discharged on the 3rd. postoperative day. Histopathological examination confirmed the diagnosis of low-grade chondrosarcoma. The tumor extension was 115×90×25mm and the margins were free of lesions. The patient was monitored on an outpatient basis and no complications were detected after five months of follow-up.
There is a consensus that a total or subtotal resection of the sternum or of three or four ribs increases the likelihood of chest wall instability and, therefore, reconstruction and the use of synthetic materials is a formal indication. Materials such as Marlex® mesh, bone cement, Prolene® mesh, bone cement composed of Prolene® mesh, a complex sandwich, stainless steel mesh, titanium mesh and titanium plate have been widely adopted in the reconstruction of major chest wall defects. But titanium prostheses have several advantages: they are inert and resistant to corrosion and biochemical degradation, have the highest strength-to-weight ratio of any metal, the ability to integrate into nearby bone structures, are flexible, and do not interfere with imaging techniques. In addition, complications are rare, including infection, fragmentation, and/or fracture.2 However, 3D designs, as the one designed in this case, give the prosthesis greater flexibility and can even reduce the risk of fracture. Therefore, titanium prostheses appear to be ideal for use in adults with large defects.2 The optimal anterior chest wall reconstruction material should provide rigid structural support to protect the heart and other visceral structures and to prevent paradoxical chest wall movement with respiration, while allowing for flexible rib movement. 1,5 The advancement of technology in the manufacture of printed titanium prostheses in 3D has revolutionized modern surgical practice and, today, it is possible to create complex implants with great precision and efficiency, which are adaptable to the individual characteristics of the patient and type of defect, thus being an attractive option for the thoracic surgeon.5 The creation of a 3D model of bone structures extracted from CT image data also provides an adequate visualization of the defect in the preoperative surgical evaluation and in the careful planning of the repair. This offers the advantage that intraoperative errors can be rectified in the preoperative period without having to resolve them during surgery.
The prosthesis in our patient was fitted exactly and symmetrically to the patient's ribcage and no additional fixation maneuvers were necessary. It also matched the shape and contour of the patient's chest wall and provided a strong but flexible structural support, with excellent esthetic results, achieving a normal appearance and allowing maximum postoperative movement capacity. The patient tolerated the procedure well and his symptoms improved significantly in the immediate postoperative period.
In this way, the prosthesis used represents a novel design that safely protects the underlying organs, with an excellent esthetic result, which confirms the high standard and remarkable qualities of this type of prosthesis for complex reconstructions of the chest wall. According to Moradiellos et al., 6 the manufacturing cost is the main disadvantage in this type of surgery.
FundingThe author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interestThe author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.