Although the unique comparison standard of primary inguinal hernia repair is the Lichtenstein technique (LICH), totally extra-peritoneal (TEP) laparoscopic inguinal hernioplasty shows, although not systematically demonstrated, clear advantages as regards, perceived pain, analgesic use, and recovery of daily life activities.
ObjectiveTo demonstrate the differences in perceived pain, analgesic use, and recovery of daily life activities between Lichtenstein hernioplasty and TEP laparoscopy.
Material and methodsA prospective, non-randomised observational study was conducted on 169 consecutive patients subjected to LICH vs TEP. The LICH was performed using local anaesthesia and sedation, and the TEP with general anaesthesia, both being performed as ambulatory surgery. The points of analysis included: analgesic use, level of perceived pain, and recovery of daily life activities.
ResultsAnalgesic use was less in the TEP group for post-operative day 4 and 5, similar to the perceived pain. As regards recovery of daily life activities, the significantly minimum differences were achieved on post-operative day 7 in favour of TEP.
ConclusionsOur study shows a significant difference as regards perceived pain and analgesic use, as well as in the level of recovery of daily life activities, when comparing both groups. TEP hernioplasty should also be considered in the non-complicated primary unilateral inguinal hernia.
: Aunque el patro¿n de comparacio¿n de la reparacio¿n de la hernia inguinal primaria es la te¿cnica de Lichtenstein (LICH), la Hernioplastia inguinal laparosco¿pica totalmente extraperitoneal (TEP) muestra claras ventajas no sistema¿ticamente demostradas en cuanto a dolor percibido, consumo de analge¿sicos y recuperacio¿n de las actividades de la vida diaria.
ObjetivoDemostrar la existencia de diferencias en dolor percibido, consumo de analge¿sicos y recuperacio¿n de las actividades de la vida diaria entre la hernioplastia Lichtenstein versus la laparoscopia TEP.
Material y me¿todosEstudio prospectivo, observacional no aleatorizado de 169 pacientes consecutivos sometidos a LICH vs. TEP. El LICH se realizo¿ mediante anestesia local y sedacio¿n y el TEP con anestesia general, siendo ambos practicados en forma ambulatoria. Los puntos de ana¿ lisis incluyeron: consumo de analge¿sicos, grado de dolor percibido y grado de recuperacio¿n de las actividades de la vida diaria.
ResultadosEl consumo de analge¿sicos fue menor en el grupo TEP para los dı¿as 4 y 5 postoperatorio, al igual que el dolor percibido. En referencia a la recuperacio¿n de las actividades de la vida diaria se alcanzaron mı¿nimas diferencias significativas en el 7.0 dı¿a postoperatorio a favor del TEP.
ConclusionesNuestro estudio muestra una diferencia significativa en cuanto a dolor percibido y consumo de analge¿sicos, ası¿ como en el grado de recuperacio¿n de las actividades de la vida diaria al comparar ambos grupos. La hernioplastia tipo TEP debe ser tambie¿n considerada en la hernia inguinal unilateral primaria no complicada.
The current gold standard technique for inguinal hernia repair is without doubt the prosthetic type Lichtenstein (LICH) repair, with or without the use of the Rutkow–Robbins type plug. The optimisation of maximum efficacy and efficiency for this technique is performed under local anaesthesia and sedation, controlled by the anesthesiologist, in an outpatient regimen. No one disputes the reproducibility of the procedure and its obvious advantages in terms of learning and cost.
However, the laparoscopy alternative, total extraperitoneal prosthetic (TEP) repair, which is similar to the Rene Stoppa open preperitoneal technique, has additional benefits not achieved by the anterior prosthetic approach. These include more rapid physical and functional recovery, less post-operative pain, less analgesia, reduced loco-regional disease, and lower rates of chronic inguinodynia. The recurrence rate is similar, although it seems to be higher in some studies.
The biggest obstacle for the spreading of the laparoscopic procedure is its learning curve. However, it might be worth reconsidering the learning curve of the standard inguinal hernia repair, which is not usually considered when comparing both techniques, and even the learning curve of the above mentioned equivalent (Nyhus hernia repair).
The aim of this study was to find out if there were any differences between the two types of hernia repair in the degree of perceived postoperative pain, analgesic consumption and recovery of activities of daily living (ADL) for those operated on as outpatients.
Patients and MethodsThis was a non-randomised, observational prospective study of 215 consecutive male patients over a period of 18 months, undergoing elective surgery for a primary unilateral inguinal hernia.
Patients with a primary unilateral inguinal hernia and scrotal component in a clinical examination performed in the supine position were excluded. Only patients with an inguinal hernia with a protrusion of the inguinal content in an external orifice were included, or where the hernia was interstitial, as in the previous study.1
The choice of surgical technique depended on the availability of a surgeon with experience in laparoscopic TEP hernia repair, and all patients were operated upon by the same surgeon (MPR). The only contraindications to laparoscopic TEP inguinal hernia surgery were prior inframesocolic surgery or a prior appendectomy with pararectal access or extensive McBurney incisions in the right inguinal hernias.
The Lichtenstein hernioplasty was performed using local anaesthesia and anaesthetist-controlled sedation. A blind ilio-inguinal block was performed by the surgeon using 0.50% bupivacaine associated with 2% mepivacaine and ketoprofen and anaesthesia of a single plane (under the oblique fascia or fascia of Scarpa) in the inguinal area, while routinely assessing the likelihood of accidental infiltration of the femoral nerve and the development of subsequent transient femoral nerve palsy.2 Resection of the sac was performed with plication of the transversalis fascia at the discretion of the surgeon, and the Lichtenstein procedure with a polypropylene mesh (6×11, normal weight) fixed with PDS 3/0 sutures according to the usual technique. The surgeons responsible for the LICH group were experts in hernioplasty (having performed over 200 hernias), and the intervention was performed on an outpatient basis, with discharge between 3 and 7h after surgery.
The laparoscopic TEP hernioplasty was performed under general anaesthesia using a balloon dissector to expand the preperitoneal space and 0.50% bupivacaine as a preventive block for trocar wounds, without infiltration of the preperitoneal space at the end of the procedure. The sac was reduced in direct hernias without any further operation on it. The sac was reduced in indirect hernias. Associated lipomas were also treated and reduced.
The “anatomical” mesh fixation technique was communicated beforehand.3 The mesh was maintained by anatomical elements in the inguinal area, after positioning one sheet of the mesh between the vas deferens underneath and vascular elements of the cord above. The upper sheet of the mesh covered the entire area of Hesselbach's triangle (direct hernias) and went behind the epigastric vessels through a retroepigastric tunnel previously created by blunt dissection just above the deep inguinal ring. Here they were loosely attached to the anterior abdominal wall by an easily dissected piece of cellulo-adipose tissue. This arrangement meant that the two sheets were overlapped in the lateral area of the inguinal space, thus “closing” the deep inguinal ring due to lateral intersection. A 14×10cm (normal weight) polypropylene anatomical mesh was used. The operations were performed on an outpatient basis with discharge times similar to LICH.
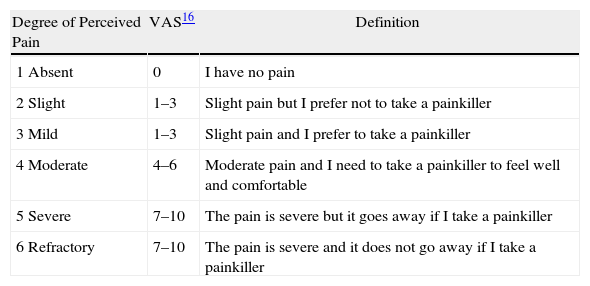
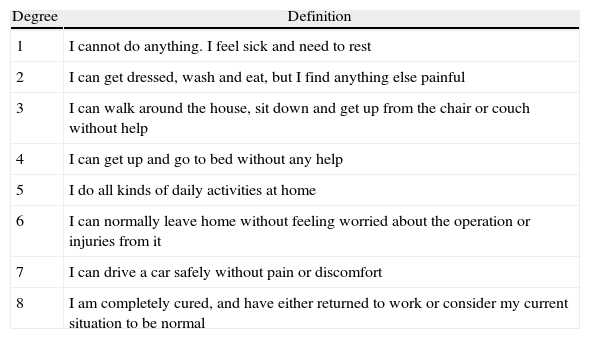
When discharged from hospital, patients were given a questionnaire about pain (at rest), analgesic consumption and recovery of activities of daily living (Tables 1 and 2). These were earlier published by our group when analysing the same parameters in outpatient laparoscopic cholecystectomy.4 Appropriate instructions to fill in the forms were provided on a daily basis until the 20th postoperative day.
Classification of the Degree of Perceived Pain, With its Description and Equivalent in the Visual Analogue Pain Scale.
| Degree of Perceived Pain | VAS16 | Definition |
| 1 Absent | 0 | I have no pain |
| 2 Slight | 1–3 | Slight pain but I prefer not to take a painkiller |
| 3 Mild | 1–3 | Slight pain and I prefer to take a painkiller |
| 4 Moderate | 4–6 | Moderate pain and I need to take a painkiller to feel well and comfortable |
| 5 Severe | 7–10 | The pain is severe but it goes away if I take a painkiller |
| 6 Refractory | 7–10 | The pain is severe and it does not go away if I take a painkiller |
Activities of Daily Living Classification.
| Degree | Definition |
| 1 | I cannot do anything. I feel sick and need to rest |
| 2 | I can get dressed, wash and eat, but I find anything else painful |
| 3 | I can walk around the house, sit down and get up from the chair or couch without help |
| 4 | I can get up and go to bed without any help |
| 5 | I do all kinds of daily activities at home |
| 6 | I can normally leave home without feeling worried about the operation or injuries from it |
| 7 | I can drive a car safely without pain or discomfort |
| 8 | I am completely cured, and have either returned to work or consider my current situation to be normal |
Magnesium metamizol in 3 daily oral doses in ampoules was recommended as post-operative analgesia. Patients were told to start taking the painkillers at the first sign of discomfort. Once the pain is established, it is difficult to control with analgesia. They were therefore advised to start treatment as soon as possible, but they were also told not to take the analgesia on a regular basis (according to a particular timetable), but only if the patient felt pain or preferred to take it as a precaution.
Patients were instructed to carry out all types of physical activities (at home or at work, practising sports or driving) that did not involve strenuous physical activity or lifting heavy weights (>30kg), with each patient evaluating their tolerance to such activity on an individual basis.
Patients, who developed local postoperative complications which could increase the pain, analgesic consumption or delayed the recovery of ADL, were excluded from the analysis (there were 7 cases of transient oedematous orchitis and 2 wound haematomas in the Lichtenstein group). Also excluded were those whose questionnaires were not properly completed (25 cases in the LICH group and 12 in the TEP group).
The data were transferred to a DbaseV database and processed using SPSS 15.0 software. Continuous data were expressed as mean and standard deviation, and were analysed by Student's t-test. Categorical variables were compared using the chi-squared test and expressed as the number of cases and percentage. A significance level of P<.05 was set.
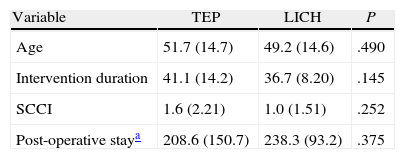
ResultsThe total number of patients studied was 169, with 53 undergoing TEP and 116 LICH procedures. All were operated on an outpatient basis.
Table 3 shows the comparison features for the 2 groups, with both groups being homogeneous in terms of comparison conditions.
Demographic and Series Homogeneity Variables.
| Variable | TEP | LICH | P |
| Age | 51.7 (14.7) | 49.2 (14.6) | .490 |
| Intervention duration | 41.1 (14.2) | 36.7 (8.20) | .145 |
| SCCI | 1.6 (2.21) | 1.0 (1.51) | .252 |
| Post-operative staya | 208.6 (150.7) | 238.3 (93.2) | .375 |
SCCI, surgical complexity classification index.
Outcome variables analysed included: daily analgesic consumption, perceived pain and recovery of ADL. The results were analysed by comparing the percentages for the defined variables (chi-squared test).
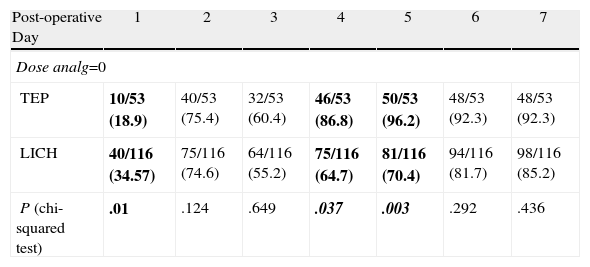
Table 4 shows the results for the consumption of analgesics. In the first 24h after surgery, the percentage of patients with lower analgesic consumption was the LICH group with 34.5% vs 18.9% for the TEP group (P=.010).
Consumption of Analgesics. Percentage by Groups of Patients Requiring no Medication by Post-operative Day.
| Post-operative Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Dose analg=0 | |||||||
| TEP | 10/53 (18.9) | 40/53 (75.4) | 32/53 (60.4) | 46/53 (86.8) | 50/53 (96.2) | 48/53 (92.3) | 48/53 (92.3) |
| LICH | 40/116 (34.57) | 75/116 (74.6) | 64/116 (55.2) | 75/116 (64.7) | 81/116 (70.4) | 94/116 (81.7) | 98/116 (85.2) |
| P (chi-squared test) | .01 | .124 | .649 | .037 | .003 | .292 | .436 |
Dose analg=0: percentage of patients who did not require any consumption of analgesics.
The percentage of patients requiring no analgesia on the 4th and 5th postoperative day, respectively, was 86.8 and 96.2 for the TEP group vs 64.7 and 70.4 in the LICH group (P=.037 and P=.003, respectively). This difference was more than 20% between the two groups and was therefore clinically relevant.
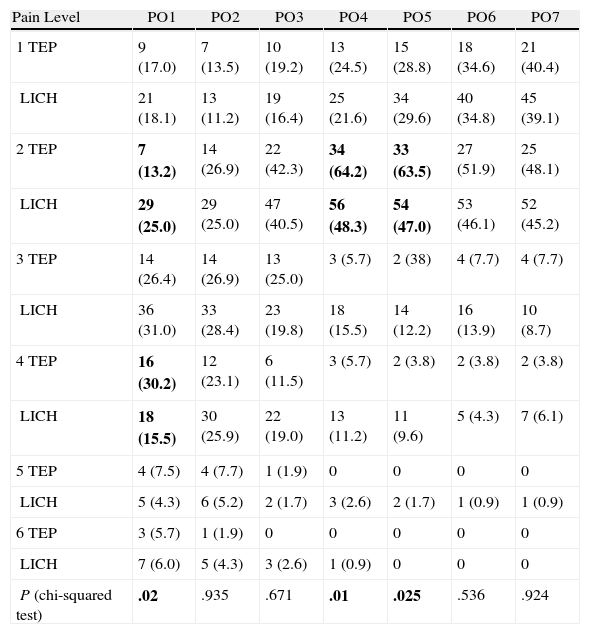
Table 5 shows the degree of perceived pain according to the scale used by our group. At 24h, there was a percentage of patients in the LICH group with less perceived pain than the TEP group (25.0 vs 13.0, P=.020). This was consistent with the analgesic consumption results in Table 4, and is due to the different anaesthetic regimens used for the ilio-inguinal block performed under local anaesthesia in the LICH group.
Perceived Pain. Percentage by Groups.
| Pain Level | PO1 | PO2 | PO3 | PO4 | PO5 | PO6 | PO7 |
| 1 TEP | 9 (17.0) | 7 (13.5) | 10 (19.2) | 13 (24.5) | 15 (28.8) | 18 (34.6) | 21 (40.4) |
| LICH | 21 (18.1) | 13 (11.2) | 19 (16.4) | 25 (21.6) | 34 (29.6) | 40 (34.8) | 45 (39.1) |
| 2 TEP | 7 (13.2) | 14 (26.9) | 22 (42.3) | 34 (64.2) | 33 (63.5) | 27 (51.9) | 25 (48.1) |
| LICH | 29 (25.0) | 29 (25.0) | 47 (40.5) | 56 (48.3) | 54 (47.0) | 53 (46.1) | 52 (45.2) |
| 3 TEP | 14 (26.4) | 14 (26.9) | 13 (25.0) | 3 (5.7) | 2 (38) | 4 (7.7) | 4 (7.7) |
| LICH | 36 (31.0) | 33 (28.4) | 23 (19.8) | 18 (15.5) | 14 (12.2) | 16 (13.9) | 10 (8.7) |
| 4 TEP | 16 (30.2) | 12 (23.1) | 6 (11.5) | 3 (5.7) | 2 (3.8) | 2 (3.8) | 2 (3.8) |
| LICH | 18 (15.5) | 30 (25.9) | 22 (19.0) | 13 (11.2) | 11 (9.6) | 5 (4.3) | 7 (6.1) |
| 5 TEP | 4 (7.5) | 4 (7.7) | 1 (1.9) | 0 | 0 | 0 | 0 |
| LICH | 5 (4.3) | 6 (5.2) | 2 (1.7) | 3 (2.6) | 2 (1.7) | 1 (0.9) | 1 (0.9) |
| 6 TEP | 3 (5.7) | 1 (1.9) | 0 | 0 | 0 | 0 | 0 |
| LICH | 7 (6.0) | 5 (4.3) | 3 (2.6) | 1 (0.9) | 0 | 0 | 0 |
| P (chi-squared test) | .02 | .935 | .671 | .01 | .025 | .536 | .924 |
No. (%); P, Chi-squared test; PO, post-operative day.
The results outside the influence of the anaesthetic block performed with bupivacaine were favourable for the TEP group on days 4 and 5. Thus, the percentage of patients who considered themselves pain-free or suffering mild pain (pain level ≤2) and not requiring analgesia as a qualitative analysis variable were 88.7 vs 60.9 on postoperative day 4 and 92.3 vs 76.6 on day 5 in the TEP and Lichtenstein groups, respectively (P=.010 and P=.025, respectively). This was statistically significant regardless of the anaesthetic regimen used.
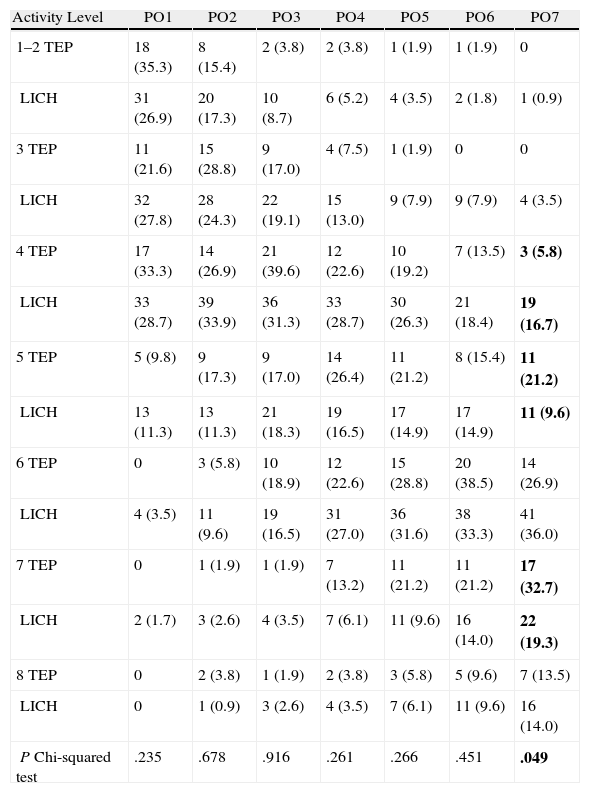
Table 6 shows the degree of recovery of ADL in the first 7 postoperative days. Both techniques showed similar results with minimal statistical significant difference on the 7th postoperative day (P=.049), which must therefore be interpreted with caution. By this time, 21.2% of patients in the TEP group performed home ADL (level 5) without restrictions, compared with only 9.6% in the LICH group.
Recovery of Activities of Daily Living.
| Activity Level | PO1 | PO2 | PO3 | PO4 | PO5 | PO6 | PO7 |
| 1–2 TEP | 18 (35.3) | 8 (15.4) | 2 (3.8) | 2 (3.8) | 1 (1.9) | 1 (1.9) | 0 |
| LICH | 31 (26.9) | 20 (17.3) | 10 (8.7) | 6 (5.2) | 4 (3.5) | 2 (1.8) | 1 (0.9) |
| 3 TEP | 11 (21.6) | 15 (28.8) | 9 (17.0) | 4 (7.5) | 1 (1.9) | 0 | 0 |
| LICH | 32 (27.8) | 28 (24.3) | 22 (19.1) | 15 (13.0) | 9 (7.9) | 9 (7.9) | 4 (3.5) |
| 4 TEP | 17 (33.3) | 14 (26.9) | 21 (39.6) | 12 (22.6) | 10 (19.2) | 7 (13.5) | 3 (5.8) |
| LICH | 33 (28.7) | 39 (33.9) | 36 (31.3) | 33 (28.7) | 30 (26.3) | 21 (18.4) | 19 (16.7) |
| 5 TEP | 5 (9.8) | 9 (17.3) | 9 (17.0) | 14 (26.4) | 11 (21.2) | 8 (15.4) | 11 (21.2) |
| LICH | 13 (11.3) | 13 (11.3) | 21 (18.3) | 19 (16.5) | 17 (14.9) | 17 (14.9) | 11 (9.6) |
| 6 TEP | 0 | 3 (5.8) | 10 (18.9) | 12 (22.6) | 15 (28.8) | 20 (38.5) | 14 (26.9) |
| LICH | 4 (3.5) | 11 (9.6) | 19 (16.5) | 31 (27.0) | 36 (31.6) | 38 (33.3) | 41 (36.0) |
| 7 TEP | 0 | 1 (1.9) | 1 (1.9) | 7 (13.2) | 11 (21.2) | 11 (21.2) | 17 (32.7) |
| LICH | 2 (1.7) | 3 (2.6) | 4 (3.5) | 7 (6.1) | 11 (9.6) | 16 (14.0) | 22 (19.3) |
| 8 TEP | 0 | 2 (3.8) | 1 (1.9) | 2 (3.8) | 3 (5.8) | 5 (9.6) | 7 (13.5) |
| LICH | 0 | 1 (0.9) | 3 (2.6) | 4 (3.5) | 7 (6.1) | 11 (9.6) | 16 (14.0) |
| P Chi-squared test | .235 | .678 | .916 | .261 | .266 | .451 | .049 |
P, Chi-squared test; PO, post-operative day.
However, intermediate ADL was managed by 26.9% of the TEP group and 36.0% of the LICH group which, while not being statistically significant, is a difference to be considered.
Finally, “complete” recovery, as considered by the patient, was perceived on the 7th day after surgery in 13.5% and 14.0% of patients regardless of the technique used, which is therefore similar in both groups.
DiscussionPerceived pain, analgesic consumption and the recovery of ADL are difficult to assess in patients who have undergone surgery.
Many factors affect the perception of pain, including the type of operation, age (with more pain felt by younger people5,6), complications, tolerance to pain itself, as well as many cultural and social factors which are difficult to evaluate, consider and analyse.7 Therefore, increasing the sample size in the prospective analysis of such subjective variables from different procedures is very important, regardless of a greater proportion of patients in one of the groups.4
Using local anaesthesia in the pre-incisional (preventive) and post-incisional modes clearly changed the intensity of perceived pain for different types of surgery.8,9 Similarly, better results for perceived pain and analgesic consumption were obtained in open inguinal repair using ilio-inguinal block and preventive infiltration, compared with other anaesthetic regimens, such as using general and locoregional anaesthesia. These latter have been questioned as anaesthetic techniques for hernia repair in favour of local anaesthesia and controlled sedation by the anesthesiologist.9 In our group, the pain-free interval after surgery with block was between 6 and 10h, which explains why the percentage of patients with no consumption of analgesics in the first 24h was lower in the LICH group than in the TEP group.
Postoperative pain after TEP is lower in some published studies,10–13 especially in the first postoperative week.11,14 However, the pain measurement techniques and anaesthetic modalities were variable and are therefore difficult to compare.
Verbal scales (mild, moderate, severe),10–14 simple scoring systems (1–10) or visual analogue scales (VAS), from 1 to 100mm, were used.
The use of VAS for assessing the hernia treatment is widespread.11,15 It is the preferred system, and has proved reliable in linearly quantifying pain in serial measurements, showing clinically relevant absolute values of VAS.
Most authors16 agree that a VAS score from 0 to 3 corresponds to nil or mild pain, for which patients do not need or want analgesia. Scores from 4 to 6 relate descriptively with moderate pain, and 7 to 10 correspond to severe pain. Therefore, the descriptive and quantitative equivalence with VAS is an accepted system of measurement.
Our scale of measurement combined all possible descriptive varieties of pain intensity perception and associated them to the treatment chosen by the patient depending on said intensity, while incorporating the treatment outcome. This makes it possible for the pain level expressed by patients to be more consistent, regardless cultural conditioning. Furthermore, this scale is easily transferred to other systems or numerically or quantitatively transformed even to the VAS system (Table 1).
Our results show clinically relevant percentage differences (over 20% of patients) between the two techniques for perceived pain and analgesic consumption. These results show the superiority of TEP on post-operative days 4 and 5 only in terms of perceived pain and analgesic consumption.
The ADL recovery results are even more difficult to evaluate for a comparative analysis of different techniques, because the common measurement scales, and that used by our group, are probably not sensitive enough to detect functional changes in each technique. Our study found only slight differences between the two groups at the 7th postoperative day, with a slight advantage for TEP. There also appears to be a greater tolerance to TEP as the home ADL without restrictions is greater. Patients who underwent laparoscopic surgery returned to work and were driving before those who underwent conventional surgery, although some studies do not report this.7
The speed of recovery of ADL may be conditioned by the development of local complications (e.g., orchitis or haematoma). TEP has a local complication rate much lower than conventional Lichtenstein hernioplasty (9.8% vs 20.4%),17 and this is confirmed in many studies. Similarly, the long-term evaluation of postherniorrhaphy inguinodynia (not chronic inguinodynia, but residual to the hernia procedure, which is of variable duration after the intervention) is favourable towards TEP (3.3% vs 9.7% for LICH).17 These results have been further corroborated by new studies showing that postoperative recovery, perceived pain (VAS) and analgesic consumption rates are better in the TEP group. This further demonstrates that the sick leave period was dependent on the degree of surgical trauma (and therefore higher in the LICH group).18
In the Lau study,19 the pain score at rest was significantly lower in the TEP group on postoperative days 0, 1, 4, 5, and 6. The patients returned to work 6 days earlier, and the incidence of inguinodynia was significantly lower in the TEP group (9.9% vs 21.7%), which points to the superiority of TEP over LICH.
Although the recurrence rate was low, it was higher for TEP, possibly due to poor surgical technique in not recognising associated hernias, and therefore, not treating them. This is generally associated with the procedure learning curve, which should be reviewed.20
Laparoscopic hernioplasty has been heavily criticised for its technical difficulty, cost and steep learning curve, which is currently estimated at 40–50 procedures.21 However, it might be considered whether the learning curve for the anterior preperitoneal inguinal hernia repair is not as complex as that of TEP, as is the case for the Stoppa preperitoneal technique and even that of a common inguinal hernia repair.
A cost-effectiveness review by McCormack et al.22 showed that the expected benefits of TEP include rapid recovery of ADL and a lower percentage of inguinal inguinodynia and dysesthesias. The cost of TEP is higher by £350, but the cost-effectiveness difference between open and laparoscopic surgery is eliminated when considering productivity costs. In relation to primary unilateral inguinal hernia, the lowest cost option is the open approach, but it has a lower QALY (hernia-free period, adjusted for quality of life) than TEP, and this latter is much better than the trans-abdominal pre-peritoneal (TAPP) option. For bilateral inguinal hernia, the most cost effective of all options is TEP. Recent randomised studies identify TEP as a factor for recurrence, although the learning curve was not estimated as a dispersion variable for many of them.
In Spain, the classic study by Feliu X strongly affirms the economic superiority of TEP (TEP-TAPP) over LICH.23
The procedure is scarcely implemented and is not widespread in Spain, with a minimum number of surgeons involved in the laparoscopic approach to inguinal hernia, despite the studies published about it since 1997.24–30 This is probably due to its steep learning curve which presents as difficult and unappealing to surgeons used to the standard procedure.
There are a number of weaknesses in our study. The first is the different anaesthetic regimens used. In the LICH group, the ilio-inguinal block with bupivacaine eliminated postoperative pain for up to 8h or more in a large proportion of patients. Therefore, the consumption of analgesics and perceived pain in the first 24h is not subject to comparison, but this does not apply for the rest of the period analysed. Nevertheless, neither general anaesthesia, which is not currently adjusted should be chosen to avoid this bias, except in patients with ischaemic heart disease9 in the LICH group nor should TEP be performed in LR anaesthesia procedures.
Second, the larger sample size may either increase or decrease the benefits received by the TEP group. For a larger sample size, the subjective assessment of pain may decrease with a more homogeneous sample of patients. This led us to include all patients in the LICH group despite the difference in sample size.
Finally, the evaluation of the ADL recovery parameters does not discriminate between one technique and the other, as it does not measure the inguinocrural functional recovery of patients. This is very evident in the physical activity follow-up in the outpatient clinic (sit on the bed, get down from the bed, get dressed) where activities are not performed equally by patients who underwent LICH and those who had TEP. This can be obviated by evaluating inguinal abdominal musculature, as done previously by Liem and Paine.31,32 This study highlights the major advantage of PET over LICH, by improving isolated and insufficient assessment for the recovery of ADL.
This is also demonstrated by the views of patients who have previously undergone surgery for hernia repair, who recall their previous experiences and opt for the laparoscopic procedure.
In conclusion, our study demonstrates the superiority of TEP over LICH hernia repair in terms of perceived postoperative pain and analgesic consumption in the first week, particularly on the 4th and 5th post-operative days for the more than 20% of cases. Recovery of ADL in the first post-operative week is slightly better in the TEP group, although this is shown only as an evident improvement on the 7th postoperative day.
Current indications in our group for TEP include primary inguinal hernia, especially if the patient is of working age, and the classical indication for bilateral inguinal hernia, with it being indicated for individually analysed recurrence.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Planells Roig M, et al. Dolor percibido, consumo de analgésicos y recuperación de las actividades de la vida diaria en pacientes sometidos a hernioplastia inguinal ambulatoria laparoscópica tipo TEP versus hernioplastia Lichtenstein en régimen ambulatorio. Cir Esp. 2011;89:524-31.