“Patients with anemia should not undergo scheduled surgical procedures without having been previously studied and appropriate treatment attempted.”
The Spanish Ministry of Health, Social Services and Equality (Ministerio de Sanidad, Servicios Sociales e Igualdad, MSSSI) has published the Enhanced Recovery after Abdominal Surgery (ERAS) guidelines1 under the auspices of several Spanish scientific societies. The ERAS guidelines explain that “the surgical Multimodal Rehabilitation (MMR) protocols have reviewed traditional perioperative practices, assessing key points specific to each type of surgery, and have analyzed the related scientific evidence.” One of these points is preoperative anemia.
In recent years, a new multimodal, multidisciplinary and individualized concept has been implemented worldwide for the integral management of surgical patients at risk for receiving blood transfusion, hemorrhaging or developing anemia2: Patient Blood Management (PBM).3,4 PBM was promoted by the WHO Global Forum Assembly (June 201) as the “appropriate multidisciplinary integral management of patients at risk for receiving a transfusion”.4 Its ultimate objective is to “reduce or eliminate the need for transfusion and improve clinical results”.5 This multimodal management is based on 3 pillars: the stimulation of erythropoiesis or treatment of perioperative anemia; the reduction of the risk for hemorrhage and active treatment of bleeding; and the tolerance to perioperative anemia, based on the acceptance of normovolemic anemia, application of “restrictive” criteria for transfusion, use of autologous blood and improved cardiopulmonary reserve.2,4 Its scope covers preoperative, intraoperative and postoperative activities.2,4,5 The recommendations include “Do not perform elective surgery in patients with anemia”.2,4
In December 2013, the MSSI presented the project Commitment to Quality of the Spanish Scientific Societies, supported methodologically by healthcare guidelines (such as ERAS).6 The recommendations include: “Do not schedule elective surgery with risk for bleeding in patients with anemia until completing adequate diagnostic studies and treatment.”6
Thus, the ERAS, MSSSI, PBM and WHO concur in emphasizing the importance of preoperative anemia and hemoglobin (Hb) levels as an important independent factor for the increased risk of perioperative morbidity and mortality.3,4 The accumulated evidence shows the relationship between a low level of Hb with the increased infection associated with treatment, prolongation of hospitalization, higher risk of re-hospitalization, thrombosis, tumor recurrence and even mortality. Anemia is one of the few risk factors that are modifiable preoperatively. Although transfusion increases Hb levels rapidly and effectively, it involves its own risks, complications and costs. Transfusion is only a temporary solution, and if the cause of the anemia is not corrected, it will re-appear.7
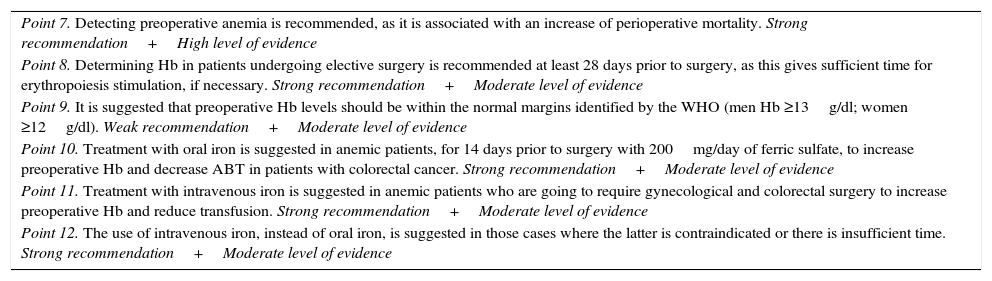
The ERAS guidelines include recommendations based on the evidence available at the time of its elaboration, and 6 are directed at the management of anemia (Table 1). For this purpose, the PRISMA protocol was used and different strategies employed to search and catalog scientific evidence, aimed at issuing recommendations, and the GRADE methodology was chosen. Nevertheless, we want to briefly review some of them with the current evidence and propose certain updates (Table 2).
ERAS Recommendations About Perioperative Anemia (Modified).
| Point 7. Detecting preoperative anemia is recommended, as it is associated with an increase of perioperative mortality. Strong recommendation+High level of evidence |
| Point 8. Determining Hb in patients undergoing elective surgery is recommended at least 28 days prior to surgery, as this gives sufficient time for erythropoiesis stimulation, if necessary. Strong recommendation+Moderate level of evidence |
| Point 9. It is suggested that preoperative Hb levels should be within the normal margins identified by the WHO (men Hb ≥13g/dl; women ≥12g/dl). Weak recommendation+Moderate level of evidence |
| Point 10. Treatment with oral iron is suggested in anemic patients, for 14 days prior to surgery with 200mg/day of ferric sulfate, to increase preoperative Hb and decrease ABT in patients with colorectal cancer. Strong recommendation+Moderate level of evidence |
| Point 11. Treatment with intravenous iron is suggested in anemic patients who are going to require gynecological and colorectal surgery to increase preoperative Hb and reduce transfusion. Strong recommendation+Moderate level of evidence |
| Point 12. The use of intravenous iron, instead of oral iron, is suggested in those cases where the latter is contraindicated or there is insufficient time. Strong recommendation+Moderate level of evidence |
Source: Clinical program for Enhanced Recovery after Abdominal Surgery (ERAS)1 Workgroup.
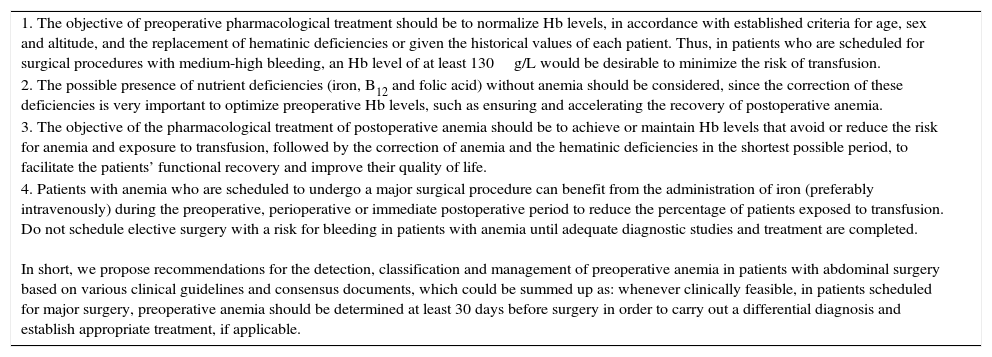
Proposals for Implementing PBM Principles in ERAS.
| 1. The objective of preoperative pharmacological treatment should be to normalize Hb levels, in accordance with established criteria for age, sex and altitude, and the replacement of hematinic deficiencies or given the historical values of each patient. Thus, in patients who are scheduled for surgical procedures with medium-high bleeding, an Hb level of at least 130g/L would be desirable to minimize the risk of transfusion. |
| 2. The possible presence of nutrient deficiencies (iron, B12 and folic acid) without anemia should be considered, since the correction of these deficiencies is very important to optimize preoperative Hb levels, such as ensuring and accelerating the recovery of postoperative anemia. |
| 3. The objective of the pharmacological treatment of postoperative anemia should be to achieve or maintain Hb levels that avoid or reduce the risk for anemia and exposure to transfusion, followed by the correction of anemia and the hematinic deficiencies in the shortest possible period, to facilitate the patients’ functional recovery and improve their quality of life. |
| 4. Patients with anemia who are scheduled to undergo a major surgical procedure can benefit from the administration of iron (preferably intravenously) during the preoperative, perioperative or immediate postoperative period to reduce the percentage of patients exposed to transfusion. Do not schedule elective surgery with a risk for bleeding in patients with anemia until adequate diagnostic studies and treatment are completed. In short, we propose recommendations for the detection, classification and management of preoperative anemia in patients with abdominal surgery based on various clinical guidelines and consensus documents, which could be summed up as: whenever clinically feasible, in patients scheduled for major surgery, preoperative anemia should be determined at least 30 days before surgery in order to carry out a differential diagnosis and establish appropriate treatment, if applicable. |
In the 8th recommendation, Hb determinations are recommended at least 28 days before surgery. We consider that the “iron metabolism studies” should be added in order to detect cases of absolute or functional iron deficiency, which are also risk factors for transfusion. Iron deficiency anemia is a risk factor for infection in abdominal surgery or hip fracture.8 In addition, the determination of vitamin B12 and folic acid should be included in patients over the age of 60.9
In the 9th point, 13g/dL (at sea level) should be considered the minimum Hb level in both men and women, to reduce risk and avoid transfusion. Women, with a smaller mass and erythrocyte volume, have a higher risk for transfusion in all types of surgery.
The 10th suggests treating anemia with oral iron during the 14 days prior to surgery. We consider that this period is insufficient to improve Hb levels and/or increase iron deposits using enteral administration. Oral iron has uncertain or inhibited absorption in the presence of inflammation.
Recommendation 12 restricts the use of intravenous (iv) iron. Other indications or situations are obviated, such as: contraindication, resistance or refractoriness to oral iron; little time before surgery; moderate to severe anemia (high need in a short time); concomitant use of erythropoiesis-stimulating agents; presence of iron deficiency associated with inflammation; or patient preference. We recommend using iv iron therapy in all cases where there is no contraindication. Intravenous iron should be the first choice in the case of preoperative anemia, reserving oral iron for those patients who cannot go to the hospital to receive parenteral treatment or with an expected long waiting list.
Supporting a recent editorial by main authors of the ERAS method,10 we believe that this is the moment to integrate PBM in MMR protocols. Now is the time for collaboration among all the specialties involved in the blood management and optimization of our patients, not only to reduce and even avoid transfusions, but also to obtain the best clinical results, less morbidity and mortality, better postoperative recovery, fewer re-hospitalizations, fewer re-operations, better quality and lower costs.
Conflict of InterestsDr. García Erce has given conferences with grants or funding from Vifor-España, Sandoz, Amgen, Alexion, Braun, GSK, Novartis and Sanofi.
The authors would like to thank Prof. Manuel Muñoz Gómez.
Please cite this article as: García Erce JA, Laso Morales MJ. «Patient blood management» en la vía clínica de recuperación intensificada en cirugía abdominal. Cir Esp. 2017;95:552–554.