Lemmel's syndrome is an uncommon pathology first described in 1934,1 defined as obstructive jaundice due to a periampullary duodenal diverticulum in the absence of choledocholithiasis or neoplasm. To date, there are few published cases, and the etiopathogenesis has not been completely established.
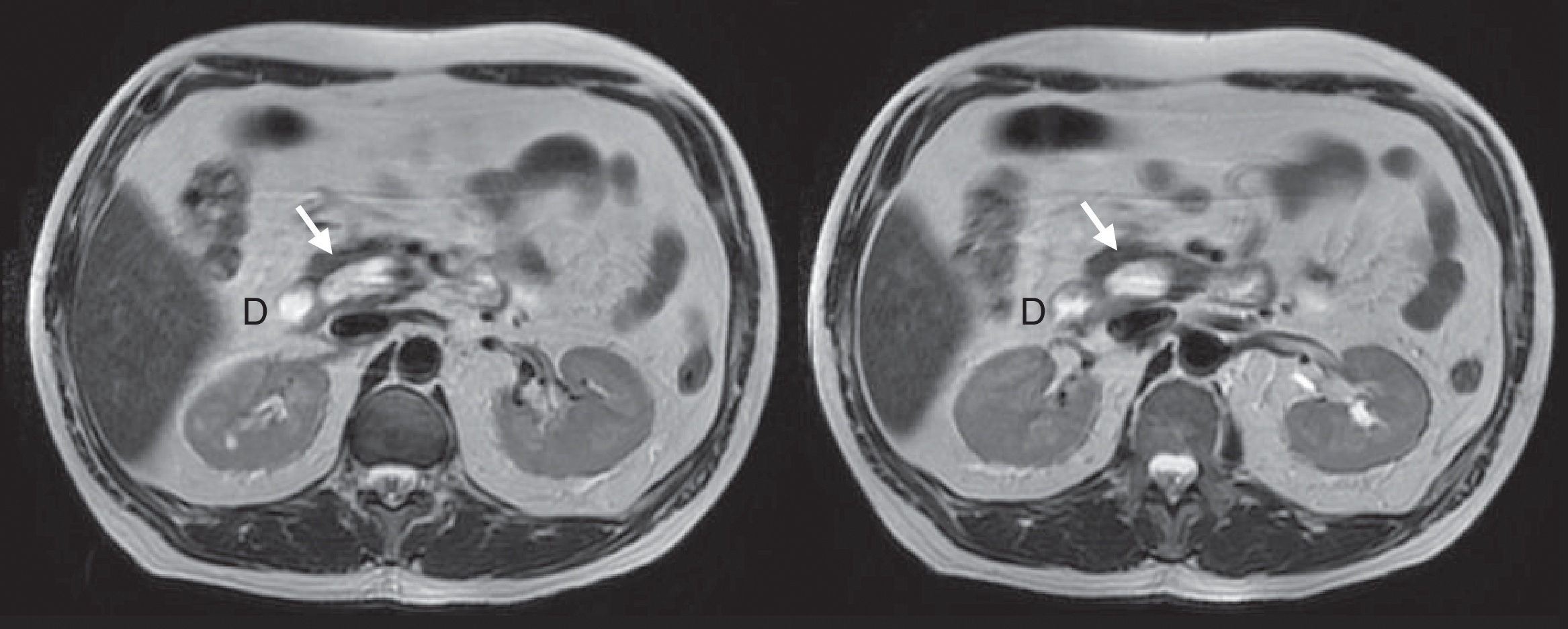
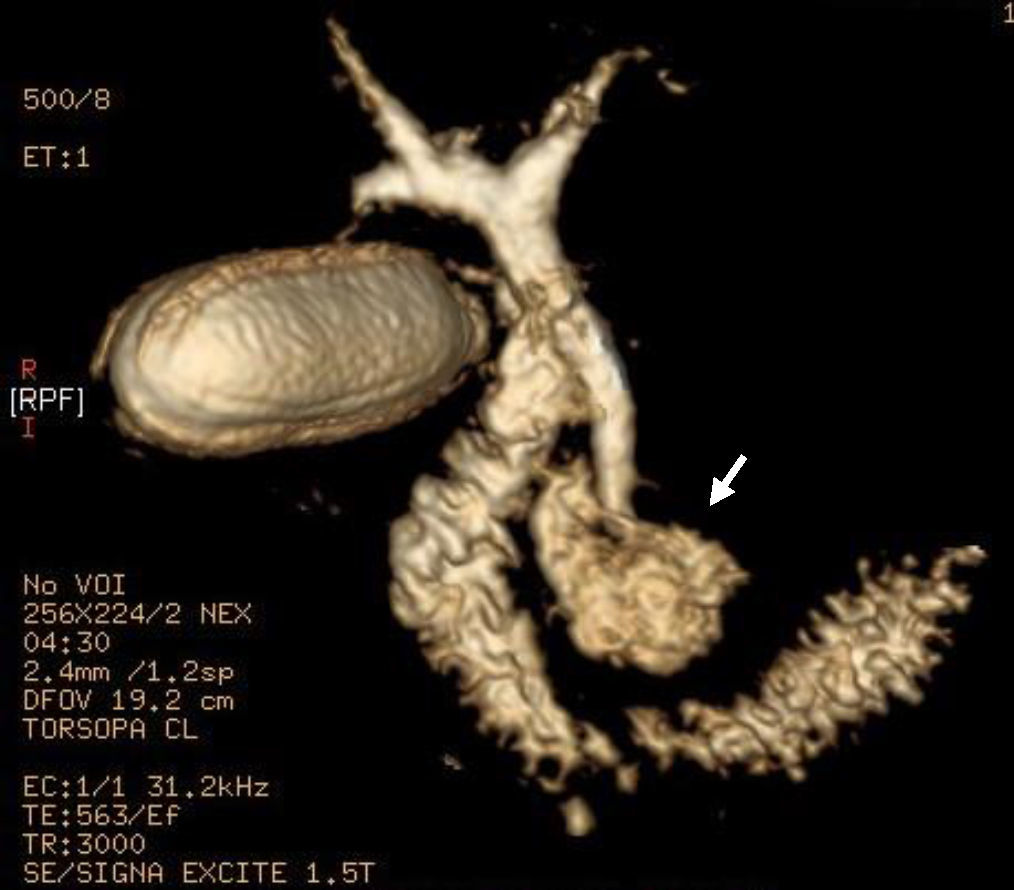
We present the case of a 54-year-old male with a history of hypertension and dyslipidemia. The patient was being studied by the gastroenterology department after having presented several self-limiting episodes of abdominal pain in the right hypochondrium and epigastrium, fever and jaundice with leukocytosis, as well as a cytolytic and cholestatic pattern seen in the lab work-up. Ultrasound showed a dilation of the proximal third of the common bile duct up to 1cm, although the distal two-thirds could not be visualized. Magnetic resonance cholangiopancreatography was performed, which revealed dilatation of the biliary tract as well as a large duodenal diverticulum with an air-fluid level in its interior that was displacing and compressing the main biliary tract, with no images suggestive of cholelithiasis or choledocholithiasis (Figs. 1 and 2). Since ERCP did not guarantee definitive treatment, the patient was referred to our surgical service.
During surgery, a 4cm diverticulum was found on the posteromedial side of the second duodenal portion of the juxtapapillary duodenum, which was compressing the distal bile duct and contained food debris. After conducting standard cholecystectomy, the common bile duct was released up to its end, along with the duodenal diverticulum, from the surrounding pancreatic tissue. Once the papilla was located with a Fogarty catheter through the cystic duct, the diverticulum was dissected at its neck; the common bile duct was dissected above the area being compressed by the diverticulum, confirming the discharge of clean bile; the bile duct was ligated distally and reconstructed using Roux-en-Y choledochojejunostomy. In the postoperative period, the patient had a subphrenic abscess that was drained surgically and a biliary fistula that was resolved with conservative management. The pathology study revealed no pathological alterations in the walls of the diverticulum. Currently, 24 months after surgery, the patient is asymptomatic and has not presented any new episodes of abdominal pain or obstructive jaundice.
The incidence of duodenal diverticula is around 17% and increases with age.2 Most are extraluminal and acquired. They are more frequently located in the second portion of the duodenum, close to the ampulla of Vater (juxtapapillary) due to the weakness of the wall in this area. Only 5% are symptomatic,3 and they are usually an incidental finding during the study of another disease or when performing an upper gastrointestinal endoscopy. The existence of a juxtapapillary diverticulum is associated with the elevated incidence of biliopancreatic disease due to, on the one hand, the extrinsic compression of the diverticulum itself on the bile duct (Lemmel's syndrome) and, on the other hand, it may favor bacterial overgrowth and consequently the production of biliary lithiasis due to beta-glucuronidase activity, in addition to inducing sphincter of Oddi dysfunction, leading to stasis and biliary reflux from the duodenum to the common bile duct.4 Other associated complications are intestinal obstruction, perforation and gastrointestinal bleeding.5
In asymptomatic cases, treatment is not justified since the risk of developing complications is very low. Endoscopic sphincterotomy is the treatment of choice in cases of biliary or pancreatic complications.6 The presence of a duodenal diverticulum does not contraindicate this procedure, although cannulation of the ampulla can be difficult if it is intradiverticular.7 Surgery is reserved for endoscopic failure.8 In our case, surgery was indicated in order to guarantee definitive treatment in a young patient with no significant comorbidities since, despite adequate endoscopic treatment, bile symptoms are recurrent and long periods of observation are required.9 There is currently no consensus on what surgical technique should be performed. Simple diverticulectomy is associated with high morbidity and mortality due to the risk of biliopancreatic duct injury, so it is mandatory to locate the ampulla of Vater using a duodenotomy or an antegrade approach through the cystic duct or choledochotomy. An associated choledochojejunostomy also decreases this risk of injury. Other authors advocate adding a gastrointestinal bypass, especially if there is local inflammation or risk of diverticular perforation.10 Other options have also been described, such as diverticular inversion, transduodenal sphincteroplasty or pancreaticoduodenectomy. No surgical option is free of the risk for complications; therefore, the treatment should be individualized according to the characteristics of the patient, the location of the diverticulum and the experience of the medical team.
Please cite this article as: Agúndez MC, Guerra DL, Pérez JF, Fernández GB. Síndrome de Lemmel: ictericia obstructiva secundaria a divertículo duodenal. Cir Esp. 2017;95:550–551.