Medullary thyroid carcinoma (MTC) is a rare disease that is silent and usually diagnosed in advanced stages, representing 2%–5% of all thyroid cancers. After years of study, we have been able to better understand its relationship with genetic factors and the presence of lymph node invasion. It can occur sporadically (70%–80%) or associated with a complex group of familial endocrinopathies (20%–30%).1 Mutations of the RET proto-oncogene located on chromosome 10q11.2 cause an alteration of the transmembrane receptor tyrosine kinase, resulting in clinical manifestations in the thyroid (in the sporadic type) and in different organs (when associated with familial syndromes).2 MTC affects parafollicular cells, increasing the secretion of calcitonin and making these levels a useful marker to evaluate the response to treatment and during follow-up. At the time of diagnosis, lymph node or distant involvement were detected in half of patients, which reduced the average survival in the latter to 3 years, with high rates of persistent disease and locoregional recurrence.3 We present a series of 12 cases that analyzes the characteristics related with the persistence and recurrence of the disease.
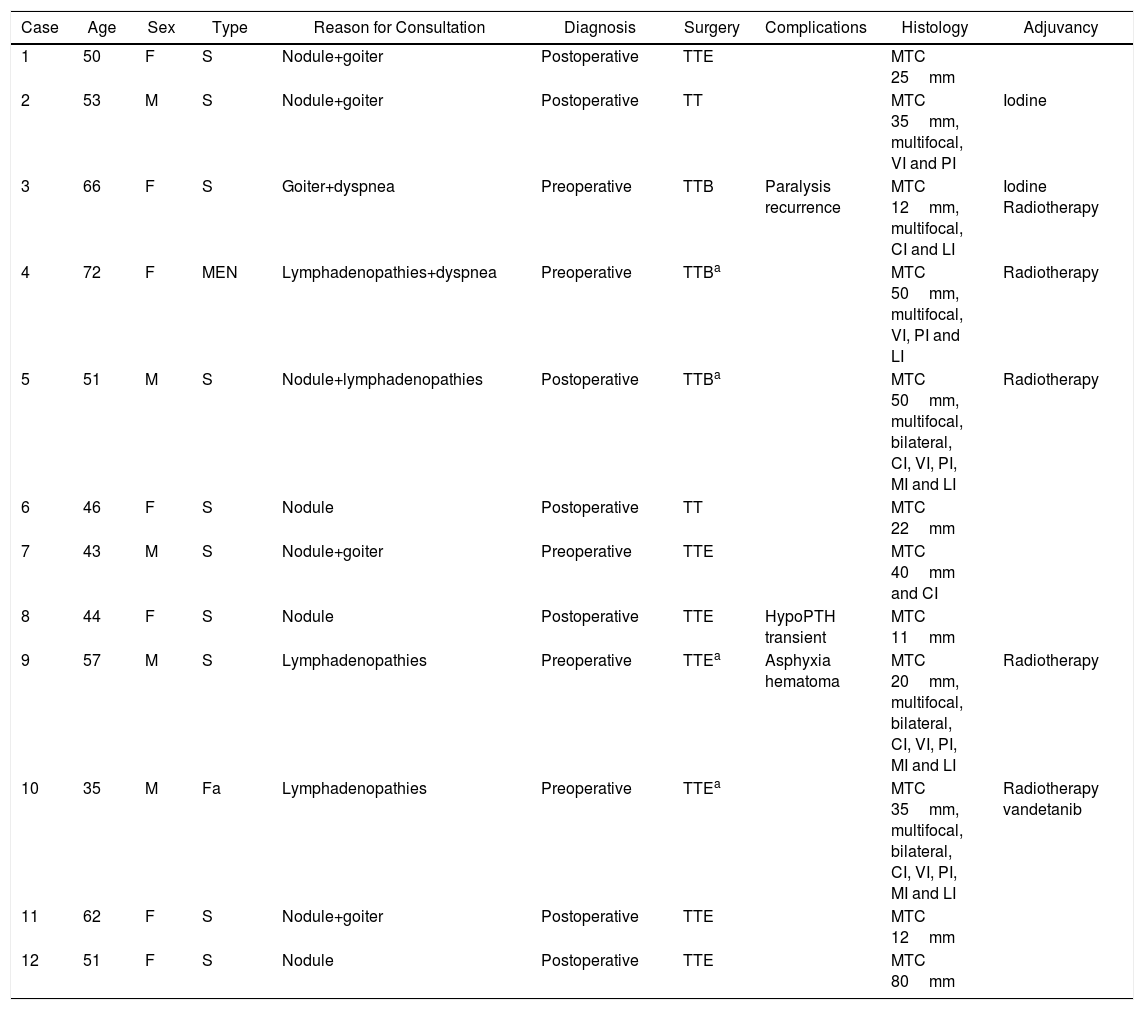
Between 2000 and 2016, 12 patients underwent surgery for MTC at our hospital, with an average follow-up of 86 months and a mean overall survival of 7.1 years. The majority were women (58%), with a mean age of 52 years and no family history of carcinoma; the study reported mutations of the RET proto-oncogene in only 3 cases. Clinically, 33% started with palpable cervical lymphadenopathies associated with other symptoms, such as goiter, nodules or dyspnea. In more than half of the patients, the diagnosis was obtained incidentally in the histological study of the piece, consequently requiring more than 2 surgical interventions for its treatment (Table 1). Analytical studies (to rule out other endocrine tumors), cervical ultrasounds (to evaluate lateral lymph node chains) and cervical–thoracic CT scans were performed systematically as extension studies in all patients during the preoperative period and were completed before totalization surgery in patients with incidental diagnoses. Total thyroidectomy was performed in all patients, with bilateral central lymph node dissection in 7; 57% were during the same surgery, and the rest were in a second operation; lateral compartment dissection was done in only 4 (cases 8–11). In 4 patients, surgery was palliative treatment as they had extensive muscular or esophageal invasion, associated with metastatic disease (mainly mediastinal or pulmonary). Three patients presented complications (Table 1): bilateral recurrent nerve paralysis (case 3), transient hypoparathyroidism (case 8) and asphyxia hematoma (case 9), the latter resulting in reoperation.
Characteristics of the Patients Treated (n=12).
| Case | Age | Sex | Type | Reason for Consultation | Diagnosis | Surgery | Complications | Histology | Adjuvancy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 50 | F | S | Nodule+goiter | Postoperative | TTE | MTC 25mm | ||
| 2 | 53 | M | S | Nodule+goiter | Postoperative | TT | MTC 35mm, multifocal, VI and PI | Iodine | |
| 3 | 66 | F | S | Goiter+dyspnea | Preoperative | TTB | Paralysis recurrence | MTC 12mm, multifocal, CI and LI | Iodine Radiotherapy |
| 4 | 72 | F | MEN | Lymphadenopathies+dyspnea | Preoperative | TTBa | MTC 50mm, multifocal, VI, PI and LI | Radiotherapy | |
| 5 | 51 | M | S | Nodule+lymphadenopathies | Postoperative | TTBa | MTC 50mm, multifocal, bilateral, CI, VI, PI, MI and LI | Radiotherapy | |
| 6 | 46 | F | S | Nodule | Postoperative | TT | MTC 22mm | ||
| 7 | 43 | M | S | Nodule+goiter | Preoperative | TTE | MTC 40mm and CI | ||
| 8 | 44 | F | S | Nodule | Postoperative | TTE | HypoPTH transient | MTC 11mm | |
| 9 | 57 | M | S | Lymphadenopathies | Preoperative | TTEa | Asphyxia hematoma | MTC 20mm, multifocal, bilateral, CI, VI, PI, MI and LI | Radiotherapy |
| 10 | 35 | M | Fa | Lymphadenopathies | Preoperative | TTEa | MTC 35mm, multifocal, bilateral, CI, VI, PI, MI and LI | Radiotherapy vandetanib | |
| 11 | 62 | F | S | Nodule+goiter | Postoperative | TTE | MTC 12mm | ||
| 12 | 51 | F | S | Nodule | Postoperative | TTE | MTC 80mm |
MTC: medullary thyroid carcinoma; S: sporadic; Fa: familial; CI: capsular invasion; LI: lymphatic invasion; MI: muscle invasion; PI: perineural invasion; VI: vascular invasion; F: female; MEN: multiple endocrine neoplasia; TT: total thyroidectomy; TTE: total thyroidectomy, extended; TTB: total thyroidectomy+lymph node biopsy; M: male.
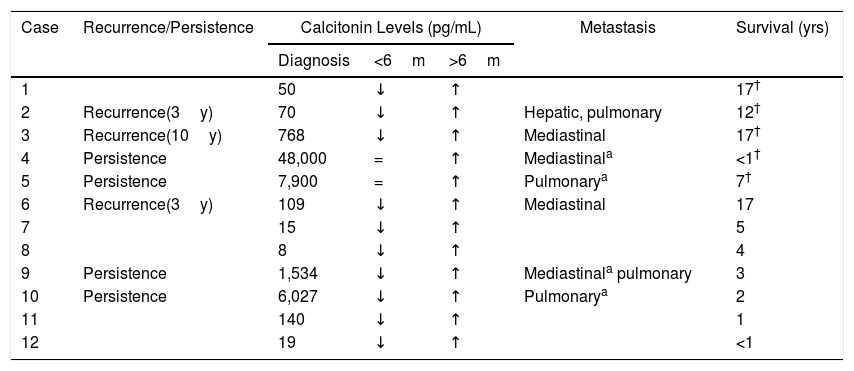
Persistent disease was defined as maintained elevated calcitonin levels 6 months after surgery, and recurrence was the increase of calcitonin after its descent or normalization in this period of time.4 Seventy-one percent of patients with disease persistence or recurrence had calcitonin levels higher than 500pg/mL at diagnosis (Table 2). Four patients had persistent disease (cases 4, 5, 9 and 10); in 2 of them (cases 4 and 5), no decrease in calcitonin levels was observed after surgery, and during follow-up they increased progressively. In the remainder (cases 9 and 10), these levels initially decreased but increased again after a few months. The maintained high levels of the first group are explained by the presence of unresected metastatic disease and the appearance of involvement in new locations,5,6 while the decrease in tumor burden would explain the initial decrease in calcitonin in the second group.6 Although it is widely accepted that calcitonin levels are related with the prognosis of these patients, they do not always coincide with the amount of metastatic deposits, and disseminated disease can be observed even with lower levels of this parameter.7
Correlation of Calcitonin Levels With Persistent Disease and Locoregional Recurrence (n=12).
| Case | Recurrence/Persistence | Calcitonin Levels (pg/mL) | Metastasis | Survival (yrs) | ||
|---|---|---|---|---|---|---|
| Diagnosis | <6m | >6m | ||||
| 1 | 50 | ↓ | ↑ | 17† | ||
| 2 | Recurrence(3y) | 70 | ↓ | ↑ | Hepatic, pulmonary | 12† |
| 3 | Recurrence(10y) | 768 | ↓ | ↑ | Mediastinal | 17† |
| 4 | Persistence | 48,000 | = | ↑ | Mediastinala | <1† |
| 5 | Persistence | 7,900 | = | ↑ | Pulmonarya | 7† |
| 6 | Recurrence(3y) | 109 | ↓ | ↑ | Mediastinal | 17 |
| 7 | 15 | ↓ | ↑ | 5 | ||
| 8 | 8 | ↓ | ↑ | 4 | ||
| 9 | Persistence | 1,534 | ↓ | ↑ | Mediastinala pulmonary | 3 |
| 10 | Persistence | 6,027 | ↓ | ↑ | Pulmonarya | 2 |
| 11 | 140 | ↓ | ↑ | 1 | ||
| 12 | 19 | ↓ | ↑ | <1 | ||
y: yrs after initial surgery; m: months; ↓: descent; ↑: increase; =: equal; †: exitus.
As for recurrences (cases 2, 3 and 6), we observed that the initial surgery was limited to the thyroid, with selective biopsy of certain lymphadenopathies. Furthermore, although there was capsular, vascular or lymphatic invasion in the histology study, no other surgical procedure was performed at that time. This could confirm the need for bilateral central lymph node dissection in all patients, especially those with high levels of calcitonin and suspicious lymphadenopathies on ultrasound,8–10 leaving lateral compartment dissection for selected cases (evidence of pathological central and lateral lymphadenopathies).9 Over time, it has been shown that the implementation of standard bilateral central lymph node emptying decreases locoregional recurrence rates, so that “berry-picking” techniques are not recommended.8,9
We observed common characteristics in both groups of patients (persistent and recurrent). Most had pathological lymphadenopathies at the beginning of the disease and had undergone incomplete initial thyroid surgery. In addition, the tumors were larger, multifocal and with capsular or vascular invasion, all of which were unfavorable prognostic factors identified in the literature.1,8,9,11 Case 6 would be an exception, as it was a smaller solitary tumor (22mm), with no capsular or vascular invasion and with a long survival, despite having relapsed 3 years after the initial surgery. External radiotherapy was the most common adjuvant option, especially in the 4 palliative patients and in one patient with recurrence. Vandetanib was used in one of the most recent cases, providing a good response until the present time. Radioactive iodine was used as adjuvant therapy in 2 patients who had associated papillary carcinoma. All the patients with recurrence presented metastatic disease during follow-up, and the first cause of general death was related respiratory insufficiency.
Calcitonin levels remain a cornerstone in the follow-up of patients, which, associated with other characteristics (incomplete surgical treatment, presence of lymph node infiltration, tumor size and unfavorable anatomic pathology characteristics of the tumor), can predict their prognosis. New therapies like tyrosine kinase inhibitors are being used with good initial results, but their use is limited only to patients with a large tumor burden and evidence of disease progression.2 Until new lines of treatment appear, surgery will be the only effective treatment for this disease, and prognostic factors will help us select the best therapeutic option for each type of patient.
AuthorshipAll the authors have participated in the study design, data collection, analysis and interpretation of the results, article composition, critical review and approval of the final version.
Please cite this article as: Tejera Hernández AA, Gutiérrez Giner MI, Rocca Cárdenas JC, Rodríguez Rodríguez F, Hernández Hernández JR. Enfermedad persistente y recaída en el carcinoma medular de tiroides. Serie de casos. Cir Esp. 2019;97:234–237.