Primary retroperitoneal mucinous cystadenomas are uncommon tumours of uncertain aetiology that mainly affect women. Micro and macroscopically, they are similar to ovarian mucinous cystadenomas, with which they can be confused, and these should be included in the differential diagnosis.
We present the case of a 35-year-old woman who, because of repeated urinary tract infections, underwent bladder and kidney ultrasound, which detected a cystic mass measuring 11cm that was in contact with the inferior pole of the left kidney. The study was followed by a computed tomography (CT) scan that identified a left anterior renal cystic mass that extended to the paracolic gutter and was spindle-shaped, well-defined and had maximum diameters of 66mm×72mm×110mm. There was no clear dependence on neighbouring organs, signs of infiltration, or exerted mass effect. Tumour markers (αFP, CEA, CA125 and CA19.9) were negative.
Given the absence of radiological signs of malignancy, the patient was followed-up with annual radiological studies.
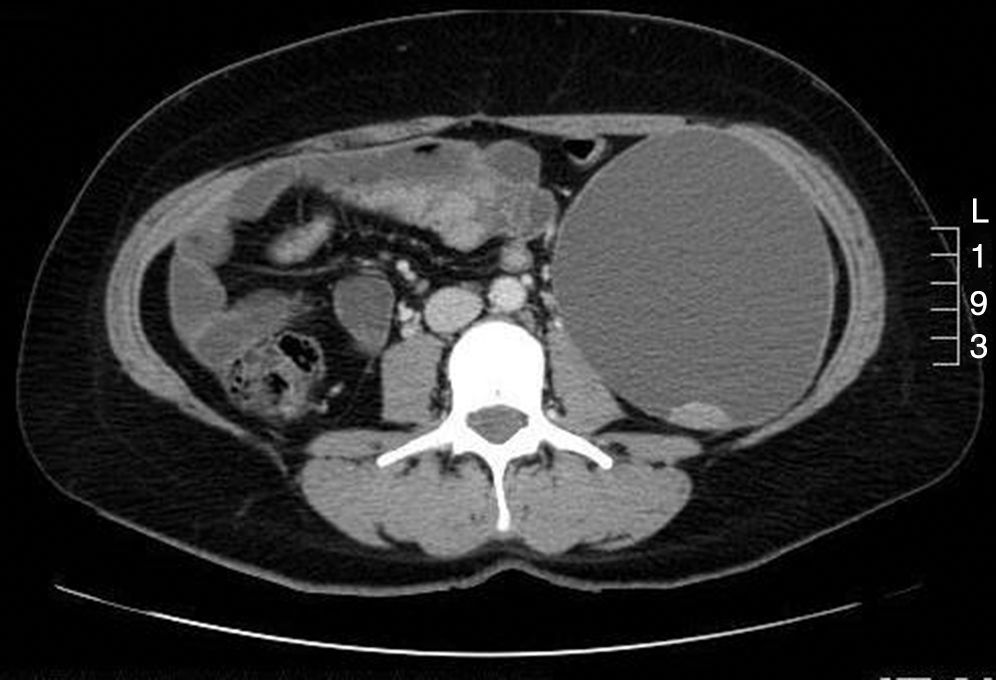
Five years after the diagnosis, ultrasound showed evidence of tumour growth, which at that time measured 109mm×103mm×140mm. Abdominal CT scan also detected wall changes of endophytic growth with papillary projections; the tumour exerted a mass effect, with medial displacement of the left kidney and psoas muscle (Figs. 1 and 2).
With these radiological changes, and because malignancy could not be ruled out, elective surgery was scheduled. The approach used was midline laparotomy, which revealed the mass located in the left retroperitoneal space and partially attached at its most anterior portion to the peritoneum. Complete exeresis was performed, without rupture of the capsule, ligating the vessels of the gonadal vessels. The patient was discharged on the third day post-op, with no incidents.
The macroscopic study reported a simple cystic formation, with diameters of 14cm×11cm×10.5cm and a weight of 890g. The definitive histopathology diagnosis was a borderline primary retroperitoneal mucinous cystadenoma with areas of low-grade carcinoma in situ. There were no signs of infiltration of the stroma, and the capsule was whole. The immunohistochemistry study was positive for CK20 and CK7, and negative for WT1. It was also positive for calretinin and oestrogen receptors. The most atypical tumour areas presented strong nuclear Ki-67 positivity (90%).
Primary retroperitoneal mucinous cystadenomas represent only 0.01%–0.2% of all retroperitoneal neoplasms1,2; only 50 cases have been reported in the literature, and only 5 of these were males.3
The origin of these tumours is not well defined, and several hypotheses have been postulated. Some authors suggest that, due to micro and macroscopic similarities, the tumours originate in ectopic ovarian tissue.4 This argument is based on the fact that both are cystic and have a structure of columnar cells, nuclei in basal position and positivity for CK7 and CK20. However, the positivity for calretinin (characteristic of mesothelial cells) and having been reported in males both partially dismiss this hypothesis. Others believe that they originate from a teratoma that would develop at the expense of an excessive growth of columnar cells. A third hypothesis postulates their development from coelomic metaplasia during embryonic growth.
The large dimensions that these tumours reach could be explained by the presence of oestrogen receptors, which would favour their growth.
Three histological types are described: (1) simple mucinous cystadenoma (the most common), which is a well-outlined benign tumour with thin walls; (2) borderline mucinous cystadenoma (the least common), which is characterised by having carcinoma in situ nodules and low malignant potential; and (3) malignant mucinous cystadenocarcinoma, which tends to recur and create metastasis.
The exact diagnosis of these tumours is difficult. Symptoms are nonspecific or even absent, and the radiologic characteristics on CT or MRI can be suggestive but not conclusive for the definitive diagnosis of the lesion.5 Preoperative FNA is debatable as it has limited diagnostic performance and entails a risk for dissemination.6 The definitive diagnosis is made with the pathology study of the surgical specimen.7
The differential diagnosis should include retroperitoneal cystic lesions, both benign as well as malignant, including cystic lymphangioma, cystic mesothelioma, cystic teratoma, Müllerian cyst, lymphocele, urinoma, etc.6
The treatment of choice of these retroperitoneal tumours is complete exeresis with an intact capsule. A less invasive approach like laparoscopy could provide apparently satisfactory results,8 but it is necessary to study the long-term progress of these cases to define the safest and most appropriate surgical technique. As for prognostic and relapse factors, these include histology grade and capsular integrity during surgical extraction. Tumour size does not seem to be a determinant prognostic factor.
Some authors have used adjuvant chemotherapy and even hysterectomy and double adnexectomy in cases of malignant cystadenocarcinoma, but there is no evidence of their usefulness due to the few cases reported.
To conclude, and in reference to our case, due to the fact that the definitive diagnosis can only be reached with the pathology analysis of the surgical specimen, we therefore believe that surgery should be indicated in future cases at the moment of diagnosis instead of periodical radiological studies.
Please cite this article as: Vicario FJ, Estalella L, Hermoso J, Díaz F, Gris P. Cistoadenoma mucinoso retroperitoneal primario. Tumoración infrecuente en mujer joven. Cir Esp. 2016;94:243–245.