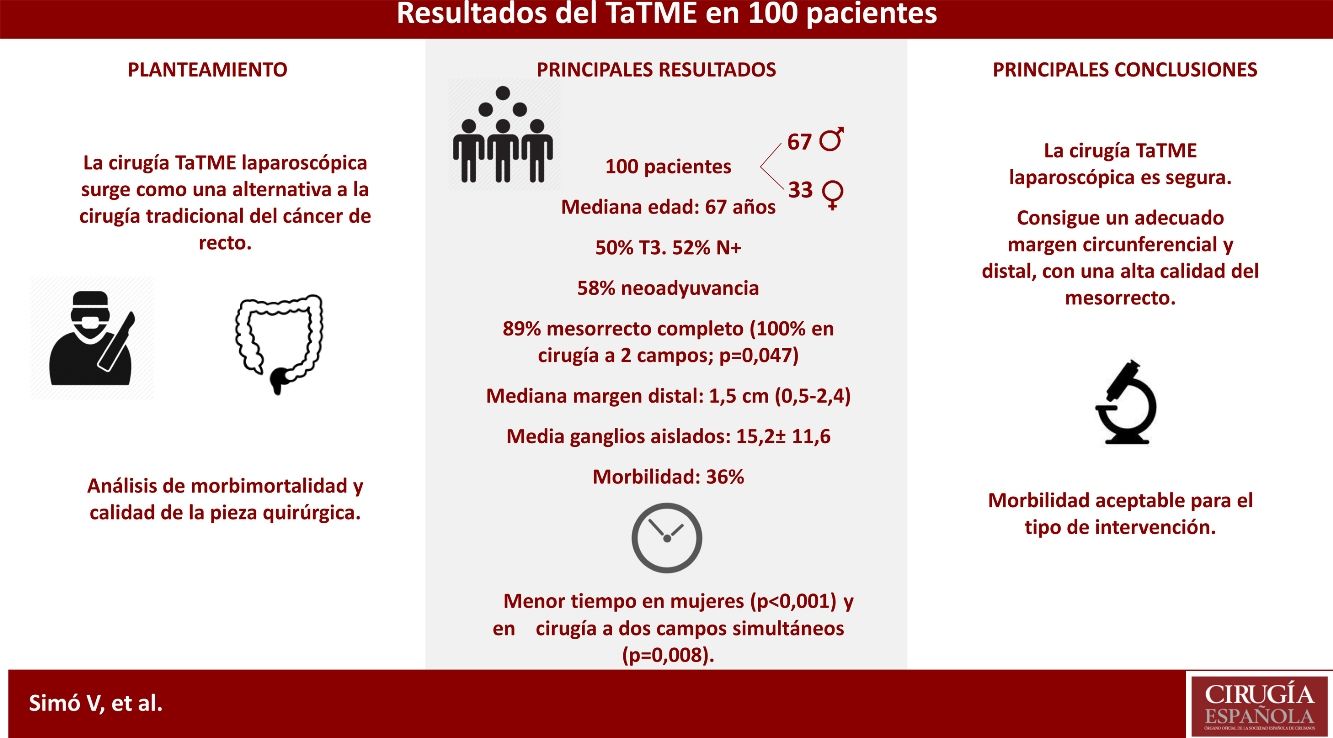
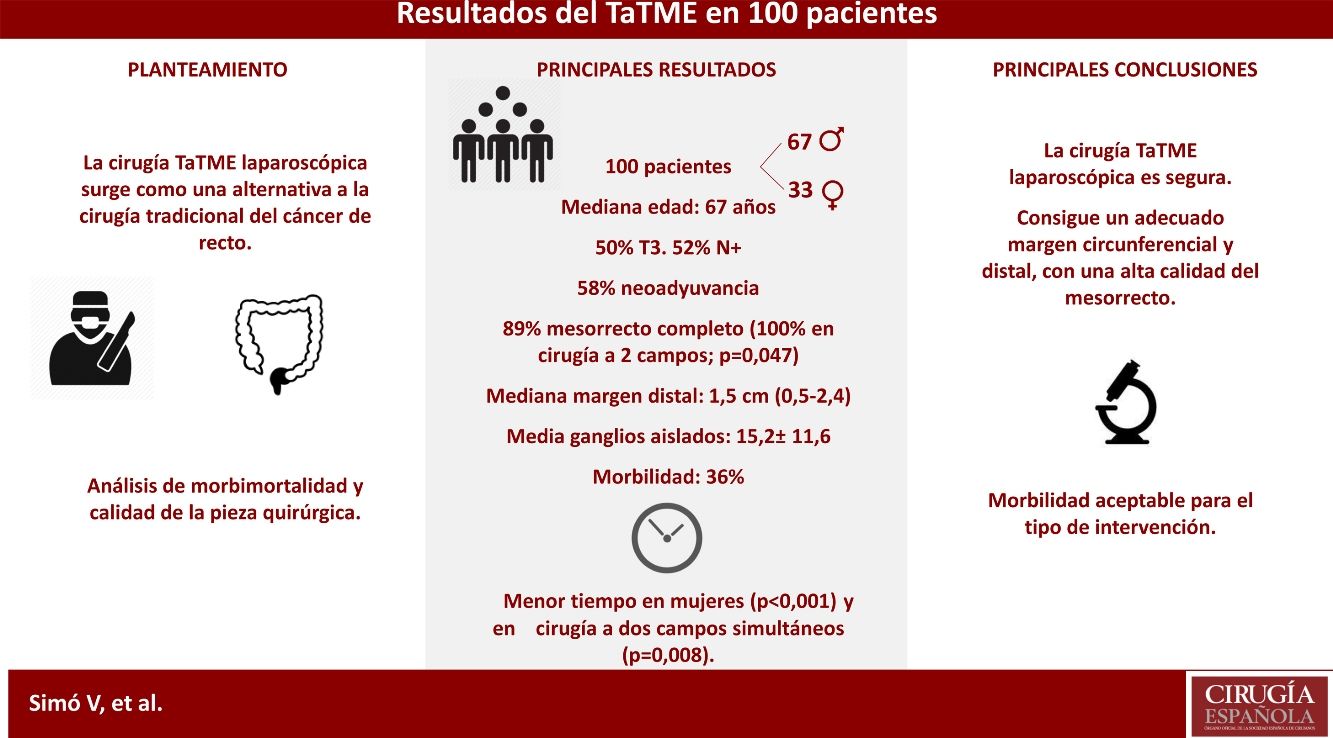
The aim of this study is to describe and evaluate our clinical short-term surgical results of laparoscopic transanal total mesorectal excision.
MethodsAnalysis of 100 consecutive patients with mid and lower rectal cancer who underwent transanal total mesorectal excision from November 2013 to September 2018. Main outcomes described are operative data, morbidities, mortality and quality of the specimen. A comparative analysis was done between gender and simultaneous versus non simultaneous abdominal-perineal surgery.
ResultsMean patient age was 67 years (56–75), and 67% were male. On MRI, 50% were stage T3 tumors, and 52% had positive nodes. Mean distance of the tumor from anal verge was 4.9±1.3cm. A total of 58% underwent neoadjuvant treatment. Mean operative time was 262±40.7min; it was shorter in females (P<.001) and in simultaneous 2-field surgery. Median specimen distal free margin was 1.5cm (0.5–2.4). A total of 89% of the specimens were with complete mesorectum, with better results when a simultaneous approach was used (P=.047). The mean number of retrieved lymph-nodes was 15.2±11.6, and 26% of patients had positive nodes. Median length of stay was 5.5 days (4–8). Morbidities occurred in 36% of cases, and one patient died.
ConclusionsAccording to our experience, laparoscopic transanal total mesorectal excision is safe and effective with adequate circumferential and distal free margins and high quality of the resected mesorectum specimen. Post-operative morbidity is acceptable, according to the current literature.
El objetivo de este estudio es analizar los resultados quirúrgicos a corto plazo de la escisión completa del mesorrecto por vía transanal laparoscópica.
MétodosAnálisis en 100 pacientes con cáncer de recto medio e inferior, intervenidos consecutivamente entre noviembre de 2013 y septiembre de 2018. Se describen los datos operatorios, la morbimortalidad y la calidad de la pieza quirúrgica. Se realiza un análisis comparativo entre sexos y la cirugía a uno y a 2 campos simultáneos.
ResultadosLa mediana de edad fue de 67 años (56–75), siendo el 67% varones. El 50% fueron tumores T3 y el 52% con afectación ganglionar, por RMN. La media de distancia al margen anal fue de 4,9±1,3cm. El 58% recibió neoadyuvancia. La media de tiempo quirúrgico fue de 262±40,7min, siendo menor en mujeres (p<0,001) y en la cirugía simultánea a 2 campos (p=0,008). La mediana de margen distal fue de 1,5cm (0,5-2,4). Se obtuvo un mesorrecto completo en el 89%, con mejores resultados en la cirugía a 2 campos (p=0,047). La media de ganglios aislados fue de 15,2±11,6. El 26% de los pacientes tuvieron afectación ganglionar. La mediana de estancia fue de 5,5 días (4-8). Hubo una morbilidad del 36% y un paciente falleció.
ConclusionesLa escisión completa del mesorrecto por vía transanal laparoscópica es segura, consiguiendo un adecuado margen circunferencial y distal, con una alta calidad del mesorrecto. Ofrece una morbilidad aceptable para el tipo de intervención quirúrgica, según la literatura actual.
Current treatment of locally advanced rectal cancer is based on the combination of neoadjuvant chemoradiotherapy followed by surgery. This therapeutic sequence has improved local disease control, compliance rate, sphincter preservation and toxicity, but has not improved overall survival.1 Total mesorectal excision (TME) on the anatomical plane, as described by Heald, is the standard surgical technique. This procedure reduces the risk of locoregional recurrence and improves survival,2 although there is interhospital variability.3 Meanwhile, the laparoscopic approach offers the advantages of minimally invasive surgery, without compromising oncological results.4
Recently, different techniques have been developed to treat rectal lesions, including the transanal approach and options like transanal endoscopic microsurgery, which has improved results in incipient tumors compared to traditional transanal excision.5 Minimally invasive transanal surgery is an easily reproducible and less expensive technique, whose initial indications have been expanded to TME.6–8
In spite of the technological advances, TME continues to be very demanding when it comes to performing the distal division of the rectum.9 Thus, the ability to obtain a sufficient distal margin may become compromised, with the obvious risk of local recurrence.10 Transanal total mesorectal excision (TaTME) is a technique in which the intervention is performed in the opposite direction to the conventional method. This provides excellent exposure of the surgical field, especially in the most complex situations: obese men, locally advanced or bulky tumors, distal third of the rectum, narrow pelvis, prostatic hyperplasia or tissue alteration secondary to preoperative radiotherapy.8 In this way, the technique has emerged as a therapeutic alternative to conventional approaches for TME, and there is new evidence of its oncological safety.11 In addition, its use has been considered for proctectomy in ulcerative colitis, rectovaginal fistula repair or bowel reconstruction after Hartmann’s intervention, and even performing complete pelvic exenteration transanally.12
The objective of this study is to describe the short-term surgical results of rectal cancer surgery using a laparoscopic TaTME approach, assessing operative data, morbidity/mortality rates and the quality of the surgical specimen. We also analyze the impact of sex and of performing the intervention in one or two simultaneous fields.
MethodsA retrospective descriptive study was conducted based on data collected prospectively from a cohort of consecutive patients treated surgically between November 2013 and September 2018.
In addition, a comparative analysis was performed based on the sex of the patient and the performance of the surgery in one or two simultaneous fields. The patients were diagnosed with adenocarcinoma of the middle and lower rectum, with a distance of up to 8cm from the anal margin, measured by rigid rectoscopy during the first consultation. Type III and IV tumors of the Rullier classification13 were exclusion criteria, as was cT4, unless it was due to involvement of the pouch of Douglas. Endoanal ultrasound was very infrequently used to assess the involvement of the intersphincteric groove. The study included all patients with middle-low rectal cancer diagnosed at our hospital and assigned for surgery with this technique by the surgical team who also met the selection criteria.
All patients were evaluated by the Multidisciplinary Oncology Committee, which assessed the indication of neoadjuvant treatment according to the criteria of the European Society of Medical Oncology.14 This study was approved by the local Clinical Research Ethics Committee, and the patients signed the informed consent form for the type of surgery being conducted.
Mechanical preparation of the colon, antithrombotic prophylaxis with enoxaparin and antibiotic prophylaxis with metronidazole and cefuroxime were carried out. The theoretical ileostomy site was marked by a stoma therapy nurse preoperatively. Starting in May 2016, all patients followed a multimodal rehabilitation protocol.
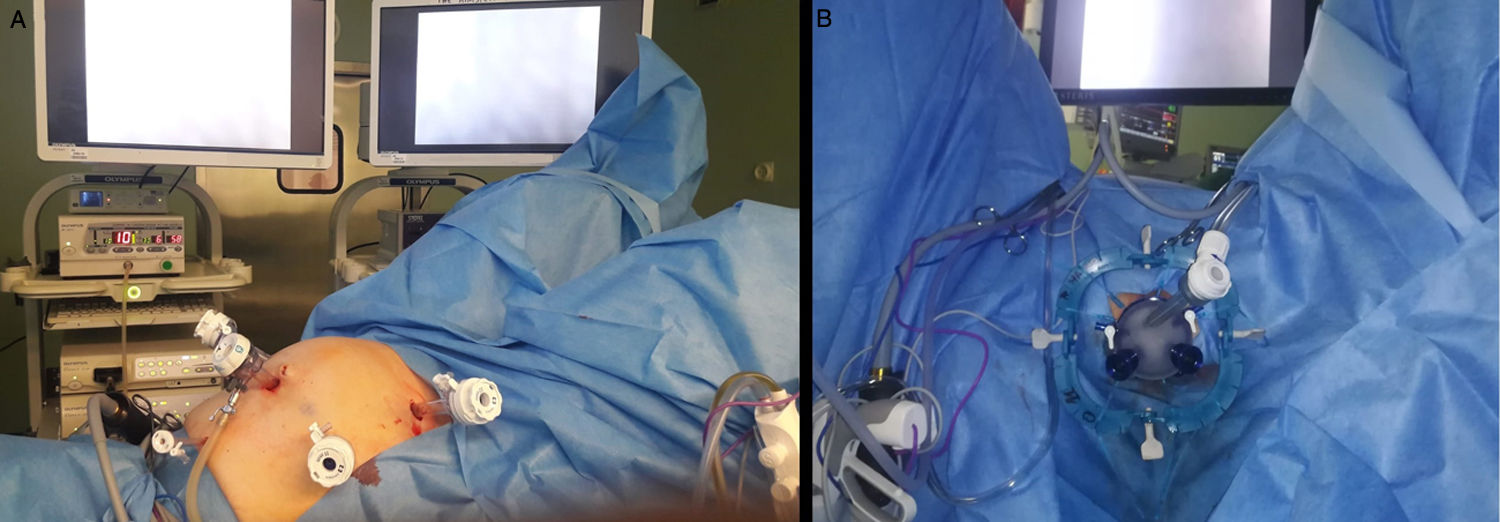
The operating room was equipped with standard laparoscopic surgery material. The patients were placed in a modified lithotomy position with Allen stirrups. In the abdominal stage, 5 trocars were used: one 12-mm supraumbilical trocar, two 11-mm trocars in the right and left flanks, one 5-mm substernal and another 12-mm in the right iliac fossa (Fig. 1A). After complete systematic descent of the splenic angle, dissection of the inferior mesenteric vessels at their origin, identifying the retroperitoneal elements, the mesorectal excision was begun, until the peritoneal reflection was opened.
For the transanal stage, the Lone Star® type separator (CooperSurgical, Trumbull, CT, USA) was used with the GelPOINT® Path Transanal Access Platform (Applied Medical, Inc., Rancho Santa Margarita, CA, USA). In the first cases, a conventional insufflation system was used, and in the last 40 interventions the AirSeal® (Palex) system was used to optimize the stability of the pneumorectum (Fig. 1B).
Following the Rullier classification,13 in type I after rectal lavage with povidone-iodine, the rectal lumen was closed with non-absorbable 2/0 suture in a tobacco pouch, and rectotomy was subsequently performed. In type II, we began with partial resection of the proximal internal anal sphincter, and then the rectal lumen was closed with 2/0 non-absorbable continuous suture. After that, the GelPOINT® Path system was introduced, which was connected to the AirSeal®. Then the ‘down-to-up’ technique was started, performing the distal division at a safe distance from the tumor. After the identification of the TME plane, the dissection was continued in the cephalic direction until it connected with the abdominal equipment. In cases of bulky tumors, visceral obesity, narrow pelvis or thickened mesorectum, the surgical specimen was removed transabdominally. In favorable cases, extraction was transanal.
In Rullier type I, a 29-mm mechanical side-to-end anastomosis was performed; in type II, a manual end-to-end anastomosis was done in accordance with the Parks technique. If sufficient colon was available, a J-pouch was created. Infrequently, the Turnbull-Cutait technique was performed in patients in whom, during surgery, poor colon preparation was observed and also in those who absolutely rejected stomata after the first consultation, so this possibility was offered. Transverse coloplasty was infrequently used in patients in whom a colonic reservoir could not be performed and who seemed candidates, due to the possibility of early stoma closure. A Blake suction drain was placed and a lateral protective ileostomy was performed in the left iliac fossa, except for patients who underwent a Turnbull-Cutait and in an exceptional case, in the absence of prior radiotherapy and due to a particular situation of patient incapacity for stoma care.
The seventh edition of the TNM classification15 was applied, describing whether the circumferential involvement was less than 2mm, both due to direct tumor involvement as well as lymph node involvement.16 The mesorectal quality analysis was classified as complete, almost complete or incomplete, in accordance with the technique published by Nagtegaal et al.17
Morbidity and mortality were described according to the Clavien-Dindo classification.18 All complications that occurred in the first 90 postoperative days or during the same hospital stay after surgery were included. Anastomotic dehiscence has been defined as evidence of contrast leak in postoperative CT, with administration of rectal contrast, requested due to clinical suspicion. Subclinical fistula has been defined as that identified during the routine opaque enema study performed one month after the intervention, with no other associated symptoms. The ileostomy was reconstructed at least one month later, unless adjuvant treatment was required, in which case it was performed afterwards.
Statistical analysisThe demographic data of the series, radiological tumor staging, neoadjuvant treatment, intraoperative aspects, type of anastomosis, pathological analysis, hospital stay and postoperative morbidity and mortality were analyzed. The results were expressed as means±standard deviation or median (p25 - p75) for quantitative variables, and by proportion for the qualitative variables. The previously mentioned variables of the 2 cohorts were compared by statistical analysis depending on whether the intervention was carried out in one field or 2 fields simultaneously, and according to sex; both groups were comparable. Categorical variables were analyzed using contingency tables and the Chi-squared test. Continuous variables were analyzed by comparing means using the Student’s t test. P values <0.05 were considered statistically significant; the SPSS® 20.0 program (SPSS Inc., Chicago, IL, USA) was used for this.
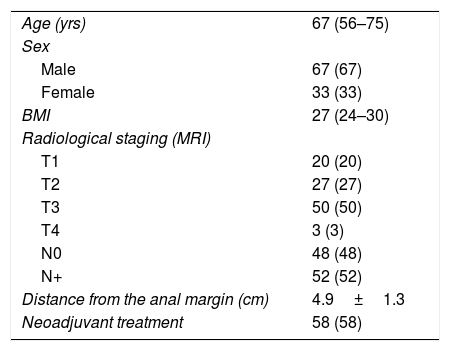
ResultsA total of 100 patients with a diagnosis of low-middle rectal cancer were treated consecutively using a laparoscopic TaTME technique. Median patient age was 67 years (56–75), and were male. The median body mass index was 27kg/m2 (24–30), while 24% presented a BMI greater than 30kg/m2. The most frequent clinical stage, measured by magnetic resonance imaging, was T3 tumors (50%). There were 20% T1 tumors that, after local resection (endoscopic or by minimally invasive transanal surgery), presented pathological factors for a poor prognosis, including lymphatic/vascular invasion or poor differentiation; the multidisciplinary committee decided to perform an oncologically correct surgery. 52% of the patients had lymph node involvement and the mean distance to the anal margin was 4.9±1.3cm. In 58%, neoadjuvant treatment was administered (Table 1).
Demographic data.
| Age (yrs) | 67 (56–75) |
| Sex | |
| Male | 67 (67) |
| Female | 33 (33) |
| BMI | 27 (24–30) |
| Radiological staging (MRI) | |
| T1 | 20 (20) |
| T2 | 27 (27) |
| T3 | 50 (50) |
| T4 | 3 (3) |
| N0 | 48 (48) |
| N+ | 52 (52) |
| Distance from the anal margin (cm) | 4.9±1.3 |
| Neoadjuvant treatment | 58 (58) |
Data expressed as mean±standard deviation, median (p25-p75) or absolute value (percentage).
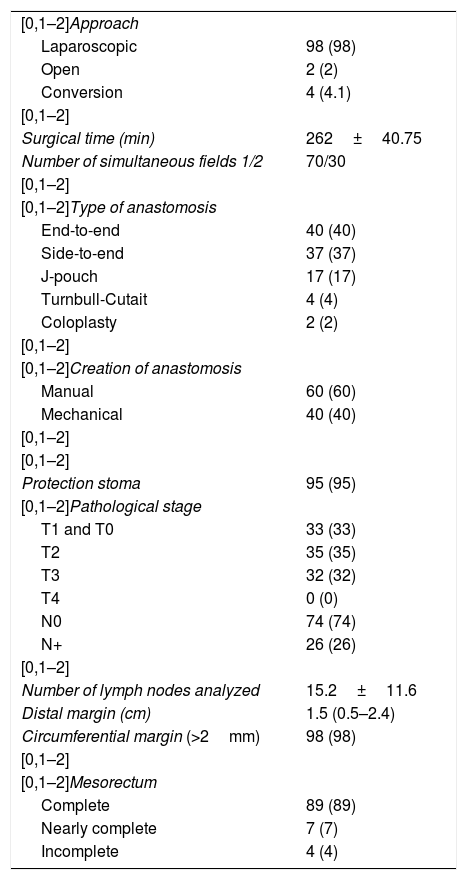
The laparoscopic approach was used in 98% of cases, requiring conversion in 4% due to adhesions secondary to previous abdominal surgeries. In all patients, the intervention was started with the abdominal phase and a TaTME was planned for each. In 30% of cases—basically the last patients of the series—the procedure was carried out simultaneously in 2 fields, which was influenced by the availability of the equipment and personnel. The mean surgical time was 262±40.7min. The most frequent anastomoses were manual end-to-end in 39%, followed by mechanical side-to-end in 37%. The median distal margin was 1.5cm (0.5–2.3). A circumferential margin greater than 2mm was obtained in 98% of the cases, achieving complete mesorectum in 89% and almost-complete in 7%. The mean number of isolated lymph nodes was 15.2±11.6, and 26% of patients presented lymph node involvement in the pathological analysis (Table 2). The median hospital stay was 5.5 days (4–8). There was an overall morbidity of 36%, and one patient died due to a complication of cardiovascular origin on the fourth postoperative day, showing no evident association with surgery or sepsis (Table 3).
Surgical and pathological results.
| [0,1–2]Approach | |
| Laparoscopic | 98 (98) |
| Open | 2 (2) |
| Conversion | 4 (4.1) |
| [0,1–2] | |
| Surgical time (min) | 262±40.75 |
| Number of simultaneous fields 1/2 | 70/30 |
| [0,1–2] | |
| [0,1–2]Type of anastomosis | |
| End-to-end | 40 (40) |
| Side-to-end | 37 (37) |
| J-pouch | 17 (17) |
| Turnbull-Cutait | 4 (4) |
| Coloplasty | 2 (2) |
| [0,1–2] | |
| [0,1–2]Creation of anastomosis | |
| Manual | 60 (60) |
| Mechanical | 40 (40) |
| [0,1–2] | |
| [0,1–2] | |
| Protection stoma | 95 (95) |
| [0,1–2]Pathological stage | |
| T1 and T0 | 33 (33) |
| T2 | 35 (35) |
| T3 | 32 (32) |
| T4 | 0 (0) |
| N0 | 74 (74) |
| N+ | 26 (26) |
| [0,1–2] | |
| Number of lymph nodes analyzed | 15.2±11.6 |
| Distal margin (cm) | 1.5 (0.5–2.4) |
| Circumferential margin (>2mm) | 98 (98) |
| [0,1–2] | |
| [0,1–2]Mesorectum | |
| Complete | 89 (89) |
| Nearly complete | 7 (7) |
| Incomplete | 4 (4) |
Data expressed as mean±standard deviation, median (p25-p75) or absolute value (percentage).
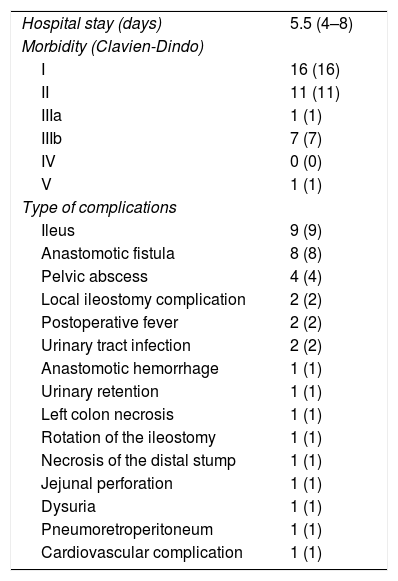
Morbidity and mortality results.
| Hospital stay (days) | 5.5 (4–8) |
| Morbidity (Clavien-Dindo) | |
| I | 16 (16) |
| II | 11 (11) |
| IIIa | 1 (1) |
| IIIb | 7 (7) |
| IV | 0 (0) |
| V | 1 (1) |
| Type of complications | |
| Ileus | 9 (9) |
| Anastomotic fistula | 8 (8) |
| Pelvic abscess | 4 (4) |
| Local ileostomy complication | 2 (2) |
| Postoperative fever | 2 (2) |
| Urinary tract infection | 2 (2) |
| Anastomotic hemorrhage | 1 (1) |
| Urinary retention | 1 (1) |
| Left colon necrosis | 1 (1) |
| Rotation of the ileostomy | 1 (1) |
| Necrosis of the distal stump | 1 (1) |
| Jejunal perforation | 1 (1) |
| Dysuria | 1 (1) |
| Pneumoretroperitoneum | 1 (1) |
| Cardiovascular complication | 1 (1) |
Data expressed as mean (p25-p75) or absolute value (percentage).
In relation to the comparative analysis according to sex, it has been observed that the duration of the intervention was shorter in women (240 vs. 276.5min); this difference was statistically significant (p<0.001). No differences were found in terms of complications or specimen quality.
When the comparison was made based on whether the intervention had been carried out starting with the abdominal stage followed by the transanal, or whether the transanal technique had been performed simultaneously with the abdominal (during which the intervention overlapped from the opening of the peritoneal reflection), we observed a shorter surgical time (247.3 vs. 272min; p=0.008) and higher percentage of complete mesorectum (p=0.047) in favor of simultaneous surgery. No other statistically significant differences were found.
After a median follow-up of 24 months (13–39), 2% of the patients have presented local recurrence and 12% distant recurrence, with a mortality rate of 10% (Table 4).
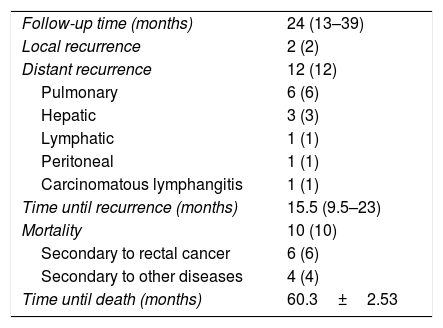
Oncological results.
| Follow-up time (months) | 24 (13–39) |
| Local recurrence | 2 (2) |
| Distant recurrence | 12 (12) |
| Pulmonary | 6 (6) |
| Hepatic | 3 (3) |
| Lymphatic | 1 (1) |
| Peritoneal | 1 (1) |
| Carcinomatous lymphangitis | 1 (1) |
| Time until recurrence (months) | 15.5 (9.5–23) |
| Mortality | 10 (10) |
| Secondary to rectal cancer | 6 (6) |
| Secondary to other diseases | 4 (4) |
| Time until death (months) | 60.3±2.53 |
Data expressed as mean±standard deviation, median (p25-p75) or absolute value (percentage).
This study provides a description of the short-term results obtained from a cohort of one hundred patients. In addition, the observed results have been compared according to sex and the approach used (one or two simultaneous fields).
Rectal cancer surgery has undergone significant development in recent decades. Laparoscopic TaTME is a hybrid approach that combines transanal and abdominal phases, reflecting the parallel evolution of technological advances and surgical requirements. Currently, it is considered an adequate method for performing quality TME, ensuring oncological results and optimizing sphincter preservation.19
However, this procedure is technically very demanding and involves a learning curve. Therefore, it should be carried out at hospitals and by surgeons with extensive experience in laparoscopic surgery and in transanal resections, who have had specific training for this intervention, such as stays at referral hospitals, courses in TaTME or cadaver practice; training in pairs is recommended.20 This is especially important, since an increase has been observed in the incidence of urethral injuries, nerve injuries and sacral venous plexus injuries using this approach.19 Therefore, it is recommended to contribute results to the international TaTME registry and to audit the quality of the resection by pathological analysis of surgical specimens.21 A recent meta-analysis indicates that TaTME provides direct tumor visualization, ensures the distal margin, reduces involvement of the radial margin and achieves complete tumor excision; all these factors have implications in long-term oncological results.22 Moreover, in the increasingly frequent scenario of having to perform TME after a previous local resection, the quality of surgical pieces seems better with this approach versus the traditional approach because there is less risk of rectal perforation.23
In light of the results published in the literature, minimally invasive transanal surgery appears to be the ideal approach for TaTME and surpasses transanal endoscopic microsurgery/surgery.24 Technological advances are still essential to facilitate this intervention, such as the implementation of continuous insufflation systems, which eliminate smoke and prevent wobbling with pneumorectum.25
Recently, the International TaTME Registry has published the results from 720 and 1594 patients.26,27 Compared to our series, the data are similar in distribution by sex, tumor stage and body mass index.27 Our population presented an older average age (67 vs. 63.7 years), a lower percentage of T3 tumors (50 vs. 69%), radiological lymph node involvement (52 vs. 57.3%) and a shorter distance to the anal margin (4.9 vs 6.0cm). As for the surgical technique, a higher percentage of manual anastomosis (60 vs. 54%) was observed due to technical reasons, given a shorter distance to the anal margin. Similarly, a longer operative time (262 vs. 241min) has been observed. The standardization of the surgical technique and overcoming the learning curve have allowed us to significantly reduce the times in our series, also facilitated by the higher percentage of cases performed in 2 simultaneous fields in the last patients. This aspect has been described in the literature, with a demonstrated decrease in operative time compared to the laparoscopic approach.28 Hospital stay is slightly shorter (5.5 vs 8 days), with a similar percentage of grade III complications (7 vs 6.1%). In our cohort, no other typical complications of this technique were observed, such as vascular or urethral injuries. We should mention the low incidence of urine retention (1%), which is a result of less nerve injury during dissection.
The pathological analysis of the surgical specimens was similar to published reports, although we would like to highlight a better pathological quality of the mesorectum when the surgery was performed in 2 simultaneous fields. This could be because dissection is simplified, mainly in the proximal portion of the rectum, as double traction was possible once communication between both fields was achieved.
Given the complexity of this technique, it seems advisable to start with the most favorable patients. In our series, the shorter surgical times observed in women could be due to their wider pelvis, no possible prostate or urethral injury, and shorter transanal dissection length. We believe that the most complex cases, although technically more difficult with this technique, may benefit most from the TaTME approach because of the better visualization and exposure of the rectum.
This is a single-center, retrospective study without a control group that entails the limitations of this type of analysis. Its advantages are that patient treatment was homogeneous (although this makes extrapolation to other medical centers difficult) and the sample size was large. More studies are needed to confirm the results and also to assess the long-term oncological and functional results of this new technique.
The laparoscopic TaTME technique allows TME to be performed safely in terms of surgical piece quality, as it ensures adequate circumferential and distal margins with a high mesorectal quality. According to the current literature, TaTME offers an acceptable morbidity rate for this type of surgical intervention.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Simó V, Arredondo J, Hernán C, Jiménez LM, Ielpo B, Fernández J, et al. Tratamiento del cáncer de recto mediante escisión completa del mesorrecto por vía transanal. Resultados en 100 pacientes consecutivos. Cir Esp. 2019;97:510–516.