We have read with special interest the case report and image of the patient described by Bernabeu García et al.1, which provided details about a case of emphysematous cholecystitis with suspected SARS-CoV-2 infection. We have recently treated a similar clinical situation.
To provide a brief description, we present the case of an 87-year-old patient with a pacemaker due to atrial fibrillation and hypertensive heart disease, treated with acenocoumarol, digoxin and antihypertensives. He reported one week of general malaise, difficulty breathing and abdominal pain, mainly focused in the right hypochondrium. He denied having had fever, nausea or vomiting.
In the emergency room, blood work was done, which showed: creatinine 3.18 mg/dL, bilirubin 3.03 mg/dL, LDH 288 U/L, ferritin 474 ng/mL, d-dimer 3.45 mg/L, as well as leukocytosis 29.6 × 109/L (92% neutrophilia) and C-reactive protein 455 mg/dL.
Given the pandemic situation in which we find ourselves, the first diagnostic suspicion that was established was respiratory failure in the context of decompensated heart failure, with possible superinfection by SARS-CoV-2 virus. However, PCR determination from nasopharyngeal and oropharyngeal swab smears was negative.
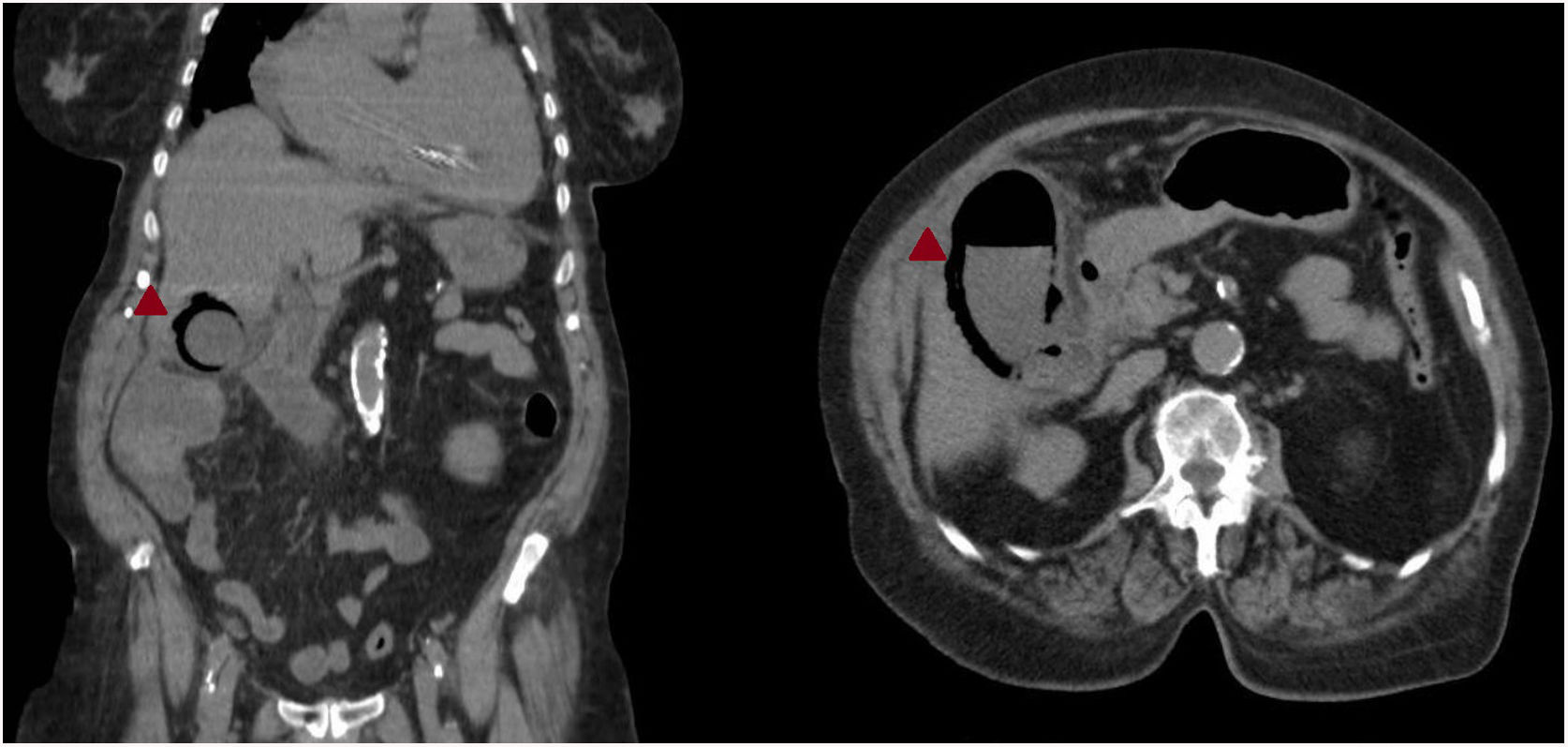
We decided to complement the study with a chest X-ray, which showed hilar congestion and a small left pulmonary effusion (Fig. 1). Thoracoabdominal scan revealed peribronchial thickening and some bibasilar laminar atelectasis, as well as a gallbladder with significant parietal emphysema, pericholecystic fluid, and rarefaction of the adjacent fat suggestive of emphysematous cholecystitis (Fig. 2). Although in our patient, unlike the case of Bernabeu García et al.1, surgical treatment was posed in addition to antibiotic coverage, the outcome was just as fatal.
Analyzing recent studies, such as the national survey on the treatment of cholelithiasis,2 an annual risk of 1%–3% was estimated for complications related to cholelithiasis due to the suspension of elective surgeries in the present pandemic situation. Many of these complications will lead to cholecystitis requiring urgent treatment. Our patient also seems to highlight the fact that there are more evolved cases,3,4 perhaps for fear of in-hospital infection or delay in the consultation of symptoms or hospital access. But what also impresses us, subjectively, is the variation in the diagnostic approach in elderly patients with previous cardiorespiratory disease, where the first diagnostic suspicion now falls on SARS-CoV-2 infection if the abdominal symptoms are not very evident. Although we have not currently found studies or data that specifically support this perception, it would be interesting analyze as it may be another factor that increases the delay in surgical treatment, and our being faced with increasingly complex clinical cases.
Please cite this article as: Gómez Sánchez J, Ubiña Martínez JA, Expósito Sequera F. Respuesta a «Colecistitis enfisematosa en un paciente con sospecha de infección por SARS-CoV-2». Cir Esp. 2021;99:167–168.