Pheochromocytomas are neuroendocrine tumors of the adrenal medulla (originating in the chromaffin cells) or extra-adrenal chromaffin tissue that occur during involution after birth and secrete excessive quantities of catecholamines. Traumatic rupture of a pheochromocytoma and the resulting retroperitoneal hemorrhage are rare complications,and management can be difficult.
We present the case of a 45-year-old male who, in a suicide attempt, fell from the fifth floor of a building and suffered severe trauma. His medical history included arterial hypertension, insulin-dependent diabetes and the presence of a right adrenal mass that was being studied after having been incidentally detected during an abdominal ultrasound performed some weeks earlier. Meanwhile, the patient was receiving psychiatric drug treatment for anxiety and depression.
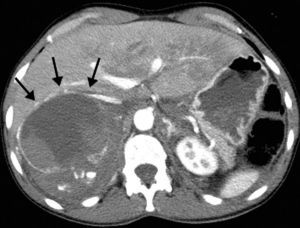
Upon arriving at our Emergency Department, the patient presented blood pressure of 180/110mmHg, heart rate 135bpm and hemoglobin 9.9g/dL. Emergency abdominal computed tomography (CT) revealed a right adrenal mass measuring 10.5cm×9cm×8.8cm with signs of active bleeding and a retroperitoneal hematoma (Fig. 1). The patient also presented facial trauma, bilateral pneumothorax and fractures of the right transverse processes from L1 to L5, sacrum, coccyx and right tibia and open fracture of the right astragalus.
Given the suspected active bleeding of the adrenal mass, the patient was considered a candidate for radiological embolization prior to the possible need for emergency surgery. Due to the hemodynamic stability and to the fact that hemoglobin levels were maintained above 9g/dL for 24h after hospitalization, we opted for a conservative approach and initiated treatment with urapidil and labetalol, which provided adequate blood pressure control 36h after hospitalization.
Catecholamine determination in urine showed levels of metanephrine of 20659mcg/dL (normal, 64–302mcg/dL) and norepinephrine 5644mcg/dL (normal, 12–85mcg/dL). These data, together with the radiological findings, established the diagnosis of traumatic rupture of a pheochromocytoma.
Four weeks later, follow-up CT showed partial reabsorption of the retroperitoneal hematoma, with better tumor definition (Fig. 2).
Laparoscopic right adrenalectomy was scheduled (fourth week of hospitalization). Nonetheless, the adhesion of the tumor to the inferior vena cava and the difficulties for maintaining the patient hemodynamically stable made it necessary to convert to open surgery, and the procedure was successfully completed. The pathology report confirmed the diagnosis of hemorrhagic cystic pheochromocytoma.
Post-operative recovery was favorable. The psychiatric symptoms disappeared and catecholamine levels progressively returned to normal limits.
Approximately 5% of the adrenal tumors are pheochromocytomas.1 In the literature, the incidence of traumatic injury to the adrenal gland is between 0.03% and 3%. Traumatic adrenal injury may itself present as a hyperadrenergic state simulating a pheochromocytoma, although when the hematoma is resolved and the gland recovers its normal function, both arterial pressure as well as catecholamine levels return to normal limits. However, complete bilateral destruction of the adrenal glands usually causes cardiovascular shock as a consequence of corticoadrenal insufficiency.2
Spontaneous non-traumatic hemorrhage of a pheochromocytoma is another rare form of presentation of these tumors, which is often associated with anticoagulant treatment or severe sepsis; abdominal pain and hypertensive crises are the most frequent manifestations. Only 54 cases have been described in the literature.3
Immediate surgery as treatment for the traumatic rupture of a pheochromocytoma has been associated with a high rate of mortality (44.7%), which is minimized if the surgery is performed electively after stabilizing blood pressure with the use of alpha blockers or after arterial embolization.3 If blood pressure is uncontrollable or bleeding is persistent despite pharmaceutical treatment, embolization should be the first option for controlling hemostasis before opting for emergency surgery.
In our patient's case history, the presence of high catecholamine levels in urine and the radiological images of adrenal gland rupture suggested the diagnosis of traumatic hemorrhagic pheochromocytoma. This is an extremely rare condition (5 cases reported in the literature) requiring complex management.4 Therefore, an adrenal mass that is discovered incidentally justifies an etiological study to rule out the presence of pheochromocytoma, which is especially relevant for trauma patients who could need surgery for other injuries. In our case, conservative management was the initial option given the patient's hemodynamic stability. The rapid response to drug treatment allowed surgical resection to be delayed, and it was performed 4 weeks later under more favorable anatomical and clinical circumstances.
Lastly, pheochromocytoma has been described as a “great imitator” due to its numerous manifestations. Anxiety is the most frequent psychiatric symptoms, with a prevalence of 22%–44% of patients with this tumor. Other less common manifestations have also been reported, such as depression, suicide attempts and delirium.5 The psychiatric problems that our patient presented were the cause of the fall and subsequent trauma injuries and were resolved after the tumor was resected.
Please cite this article as: Gómez Hernández MT, et al. Hemorragia retroperitoneal tras rotura traumática de un feocromocitoma. Cir Esp. 2013;91:197–9.