Spontaneous haematoma of the rectus abdominis muscle is an uncommon cause of abdominal pain. It occurs mostly in anticoagulated patients. The objective of this paper is to analyse the onset, diagnosis and treatment in patients under anticoagulant therapy.
MethodsA retrospective analysis of a prospectively maintained database of all patients with a diagnosis of spontaneous haematoma of the abdominal rectus muscle between March 2003 and December 2014.
ResultsThe study included 34 patients, of whom 28 were women, with an average age of 80 years old. All the patients showed a unilateral infraumbilical haematoma. Twenty-eight patients had received long-term anticoagulant treatment (26 with acenocumarol and 2 low molecular weight heparin); and 6 patients were under anticoagulant prophylaxis with low molecular weight heparin. The diagnosis was performed with ultrasound in 7 cases, computed tomography angiography in 27 patients, and with both methods in 6 cases. The treatment consisted of stopping the anticoagulant drug, correcting haemostasis parameters and blood transfusion when required. Ten patients displayed active bleeding in the computed tomography angiography, and 8 underwent selective arterial embolisation. The evolution was successful in 34 patients, however, 2 patients required surgery and, finally, died due to persistent haemorrhage.
ConclusionSpontaneous haematoma of the rectus abdominis muscle is more frequent in elderly women under oral anticoagulant treatment. Non-operative treatment is successful in most cases. Computed tomography angiography is useful to determine which patients could benefit from selective arterial embolisation.
El hematoma espontáneo del músculo recto del abdomen es una causa infrecuente de dolor abdominal que sucede con mayor frecuencia en pacientes anticoagulados. El objetivo de nuestro trabajo fue analizar la forma de presentación, el diagnóstico y los resultados del tratamiento en este grupo de pacientes.
MétodosAnálisis retrospectivo con una base de datos prospectiva de todos los casos de hematoma espontáneo del músculo recto del abdomen tratados en nuestro centro entre marzo de 2003 y diciembre de 2014.
ResultadosSe incluyó a 34 pacientes (25 mujeres) con una edad media de 80 años. En todos los casos el hematoma fue unilateral e infraumbilical. Veintiocho pacientes recibían tratamiento anticoagulante como parte de su tratamiento habitual (26 de ellos acenocumarol y 2 pacientes heparinas de bajo peso molecular a dosis terapéuticas). Seis pacientes recibían heparina de bajo peso molecular a dosis profilácticas. El diagnóstico se realizó mediante ecografía en 7 pacientes, tomografía axial computarizada con contraste intravenoso en fase arterial (angio-TC) en 27 y, con ambos métodos, en 6. El tratamiento consistió en la suspensión de la anticoagulación, corrección de la hemostasia y reposición hemática. En 10 pacientes se evidenció hemorragia activa en angio-TC y en 8 se realizó embolización selectiva. La evolución fue favorable en 32 pacientes. Dos pacientes fueron intervenidos debido a hemorragia grave persistente y fallecieron.
ConclusionesEl hematoma espontáneo del músculo recto del abdomen es más frecuente en mujeres de edad avanzada y en tratamiento con anticoagulantes orales. La mayoría evolucionan favorablemente con tratamiento no operatorio. La angio-TC es útil para indicar la embolización arterial selectiva en caso de hemorragia activa.
The most common cause of haematomas in the rectus abdominis muscle is trauma. They may occur after surgical procedures, direct trauma to the abdominal wall, subcutaneous injections, insertion of laparoscopic trocars, etc.1 Although haematomas caused by trauma had been identified in Ancient Greece,1,2 the first bibliographic reference is attributed to Maydl in 1882.3 In 1946, Teske presented a case of spontaneous haematoma of the rectus abdominis muscle when he analysed a series of 100 cases, including those caused by trauma.4
Less common than haematomas of traumatic origin are spontaneous rectus sheath haematoma (RSH), in which there is no direct trauma responsible for the lesion and the patient's baseline disease or medication have a causal relationship (blood dyscrasia, high blood pressure, oral anticoagulants, use of heparins, respiratory infection or coughing).
Spontaneous RSH is defined as the accumulation of blood in the interior of the muscular sheath due to rupture of the inferior or superior epigastric arteries, or one of their branches.5 It is usually more frequent in women and situated in the infraumbilical region. The inferior epigastric artery is most often responsible.
These haematomas may appear with abdominal pain or palpable mass and, occasionally, pose a problem in the differential diagnosis. They represent less than 2% of all cases of abdominal pain treated in the Emergency Department.6 Complications include those derived from the hypovolemic shock caused by the haemorrhage and others such as increased intraabdominal pressure, muscle necrosis, coronary syndromes because of low output, or even patient death.
In the following article, we present an extensive series of patients with spontaneous RSH from a single hospital. The objective is to analyse the forms of presentation of spontaneous RSH, determine the risk factors that favour its appearance and discuss treatment results.
MethodsWe have conducted an observational study of the patients who presented spontaneous RSH and were treated at the Hospital Príncipe de Asturias in Alcalá de Henares (Madrid) by the General and Digestive Tract Surgery Department. In accordance with the distribution protocol in the Emergency Department at our hospital, all patients with this disease were admitted to the Surgery ward or, if a coinciding pathology required, they were admitted to other wards but an evaluation by the Surgery Department was requested in all cases. Data was collected prospectively between March 2003 and December 2014.
Excluded from the study were cases of trauma-related RSH, those that presented during the postoperative period after abdominal surgery and those that affected other locations such as the retroperitoneum or iliopsoas muscles.
For each patient, data was collected for each of the following parameters: age, sex, baseline disease, reason for hospitalisation, pre- and post-haemorrhage haemoglobin, platelet count, coagulation parameters (such as the international normalised ratio [INR]), hospital stay, pro-haemostatic agents administered, concomitant diseases, radiology results, haematoma size, treatment, need for surgical intervention and patient progress.
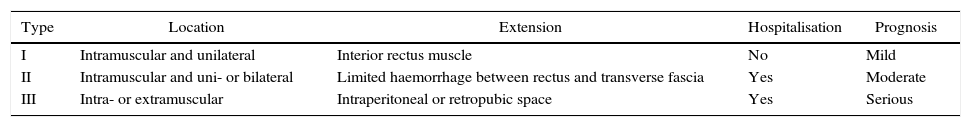
For the diagnosis of RSH, confirmation was required with imaging studies, specifically either abdominal ultrasound or computed tomography (CT) scan. For an objective description, we used the classification proposed by Berna et al. based on the size and location of the spontaneous RSH after CT scan.7 This classification is able to define the RSH as one of 3 types with implications in terms of presentation, severity and prognosis. Type I refers to unilateral RSH that only extend in the interior of the muscle, with no haemodynamic compromise. Type II includes RSH with bleeding that may extend between the rectus abdominis muscle and the transverse fascia, with a drop in haematocrit levels. Type III is reserved for the severest cases with extension of the haemorrhage towards the peritoneum or retropubic space (Table 1).7,8
Berna Grading System for Rectus Abdominis Haematomas.
| Type | Location | Extension | Hospitalisation | Prognosis |
|---|---|---|---|---|
| I | Intramuscular and unilateral | Interior rectus muscle | No | Mild |
| II | Intramuscular and uni- or bilateral | Limited haemorrhage between rectus and transverse fascia | Yes | Moderate |
| III | Intra- or extramuscular | Intraperitoneal or retropubic space | Yes | Serious |
In patients with signs of active bleeding on CT angiography, selective arteriography and embolisation of the arterial vessel were performed by the Vascular and Interventional Radiology Department.
Statistical AnalysisThe data were tabulated in a computerised database (Microsoft Office Excel 2010®). For categorical variables, the proportion of each category was calculated over the total number of patients. For the qualitative variables, we studied the distribution of phenomena, while for the quantitative variables we studied the means and standard deviation.
ResultsThe analysis included all patients diagnosed with spontaneous RSH during the study period. There were 34 patients (25 women and 9 men) with ages between 53 and 93 and a mean age of 80.3±9 years.
The most frequent symptoms were abdominal pain and the presence of a palpable mass, both of which were present in 30 patients. Four patients presented nausea, 10 tachycardia, and 2 vomiting. The most frequent location was in the left lower hemiabdomen (21 patients).
All patients were being treated with some sort of anticoagulant medication. In 28 cases, the patients were being treated with anticoagulants as part of their routine treatment: 26 with acenocoumarol and 2 with low-molecular-weight heparin (LMWH) with Clexane® at a dose of 60mg every 12h, administered subcutaneously. Another 6 patients received LMWH as prophylaxis (subcutaneous Clexane® 40mg/24h) over the course of their hospitalisation due to concomitant disease.
The indications for anticoagulation therapy were: atrial fibrillation in 14 patients, atrial flutter in 2, pulmonary thromboembolism in 3, recurring deep venous thrombosis in one and prosthetic valves in 8, and prophylactic administration during hospitalisation in 6.
Only 9 patients who were being treated with oral anticoagulants presented a dose that exceeded the anticoagulation dose required for their pathology. The INR of the anticoagulated patients with acenocoumarol who did not present overdose at the time of diagnosis was 2.1±0.9, while in patients with excessive dosage it was 4.23±1.8.
In 25 patients, a significant drop in haemoglobin was detected (more than 2 points from the previous net value of haemoglobin), which required transfusion of blood products in 23 patients of an average of 3 units of packed red bloods cells each. In order to correct the anticoagulation, we requested assessment from the Haematology Department at our hospital, which recommended the administration of coagulation factors (Octaplex® 25U/kg) in anticoagulated patients who did not have prosthetic valve replacement (20 patients). In the 9 patients who had excessive doses of Sintrom® and in the 2 anticoagulated patients with LMWH at therapeutic doses, vitamin K was administered intravenously (Konakion®, dose of one 10mg ampoule/1mL) in conjunction with Octaplex® (dose 25U 7kg). In the 2 patients who required urgent surgery, fibrinogen was also used (2g). In one patient, fresh plasma was also administered (20mL/kg weight) due to a situation of haemorrhagic shock. After assessing the risks and benefits, anticoagulation was temporarily suspended in 33 patients (only in the patient with aortic valve prosthesis was anticoagulation maintained, although acenocoumarol was temporarily substituted for LMWH at a dose of 40mg/24h).
For the diagnosis of spontaneous RSH, abdominal ultrasound was used in 7 patients while, in the remainder, CT scans were used. In 6 patients, both tests were done. In those patients who presented a drop in haemoglobin (21 patients), CT angiography was conducted after the administration of intravenous contrast in the arterial and portal phases. In the remainder (6 patients), the study was only done in baseline and venous phases.
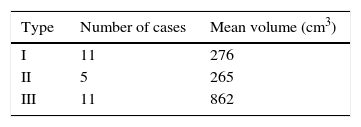
According to the Berna classification,7,8 based on CT findings, 11 patients presented type I haematoma, 5 patients type II haematoma and 11 patients type III. We calculated the mean volume for each type of spontaneous RSH represented as an ellipsoid, and using the formula (V=4/3×3.1416×AP×TR×CC), where V means volume measured in cubic centimetres, AP is anteroposterior axis, TR is transverse axis and CC is craniocaudal axis, measured in centimetres6 (Table 2). CT angiography in the arterial phase showed evidence of active bleeding in 10 patients. In 9, the inferior epigastric artery was identified as being responsible, and in one it was the superior gluteal artery, due to an anatomical variation of the vascular arcade (Fig. 1). In 8 patients, arteriography and selective embolisation were used afterwards, and bleeding ceased (Figs. 2 and 3).
With the non-surgical treatment based on the suspension of anticoagulation, blood replacement, coagulation factor replacement and selective arterial embolisation, 32 patients progressed satisfactorily. Only 2 patients were treated surgically. In these 2 cases, active haemorrhage had been previously identified on CT angiography, but embolisation could not be done due to local logistical problems. Surgery was indicated for progression of the haematoma and the haemodynamic instability caused by the haemorrhage. We drained the haematoma and achieved haemostasis of the bleeding vessel. These patients were the eldest subjects of the series (92 and 93 years old), and both died. After the initial hypovolemic shock, the first patient developed respiratory distress with multiple organ failure. The second died of pneumonia associated with mechanical ventilation.
After overcoming the spontaneous RSH episode, we assessed the risks and benefits of maintaining anticoagulation therapy after hospital discharge. In 7 patients, anticoagulant therapy was suspended, and in 2 patients acenocoumarol was substituted for LMWH at prophylactic doses due to the age of these patients and having assessed the risks and benefits of the treatment. There were no thrombotic or thromboembolic effects related with the modification of the doses or the replacement of the anticoagulant drug during patient follow-up. Mean hospital stay was 14 days.
DiscussionOur study presents the largest case series of spontaneous RSH at a single hospital in Spain.6 All other publications report a greater number of women with RSH than men, at a 3:1 ratio,2–4 which concurs with our data. It is also observed in pregnant women, with a reported foetal mortality rate of approximately 13%.9 RSH are more frequently located on the rectus abdominis muscle of the right side, infraumbilical, although in our series the predominance was seen on the left side.2,10
According to Luhmann et al.,1 the mean age for spontaneous RSH is usually in the fifth or sixth decades of life. Nevertheless, in our series the mean age was higher (80 years). Our data coincide with other recent publications that report that the incidence of RSH has increased in recent decades, which is in correlation with the indication of anticoagulant therapy in increasingly older patients.11
Abdominal pain and the presence of a palpable mass are the most characteristic symptoms and signs of this condition.5 Spontaneous RSH is an uncommon cause of acute abdomen, but it should be suspected when it coincides with a detected abdominal mass. Several signs have been described to suspect its presence during physical examination: Fothergill sign (positive when the contraction of the abdomen reveals a less mobile midline mass), Laffont sign (presence of equimosis on the mass), Nadeu sign (abdominal pain due to the elevation of a lower extremity or head) or Carnett sign (positive when pain increases with the change from supine decubitus to the sitting position). All these signs can be of great help during the abdominal examination of these patients.1,6
Nausea, vomiting and tachycardia caused by the haemorrhage are also frequent, but these are more non-specific symptoms. We have observed that signs of peritoneal irritation can also appear, due to the absence of the posterior sheath of the rectus abdominis under the arcuate line (arch of Douglas), which means that only the peritoneum and transverse fascia lie between the haematoma and the abdominal organs.12 Haematomas that collect in this space are classified as Berna type III.10,13 It is a known fact that the use of oral anticoagulants increases the risk for haemorrhage, either as external bleeding or haematomas.14 The rectus abdominis and iliopsoas muscles are the most frequent places for spontaneous haemorrhage in these patients. Only 9 patients out of the 26 who received treatment with acenocoumarol presented, at the time of diagnosis of the RSH, excessive dosage for the dose of anticoagulation required for their pathology. In other words, most were within the recommended therapeutic range for anticoagulation. The exact pathogenic relationship between anticoagulation and spontaneous RSH is unknown. A diffuse microvascular origin has been suggested as a result of the damage caused to the intima of the vessels by arteriosclerosis, or perhaps some heparin-type anticoagulants induce microangiopathy. This could indicate that the anticoagulant agents make the vascular wall somewhat labile.15,16 It is possible that the coincidence with other triggering factors (such as increased abdominal pressure caused by coughing) may cause the vascular rupture and haematoma.17 Due to the increase in the number of patients at increasingly older ages being treated with anticoagulant drugs, it is likely that we will see spontaneous RSH more frequently in the future.
The radiological test that presented the best performance was CT, which detected RSH in all cases and provided information about its extension and size. Moreover, in combination with intravenous contrast at baseline, arterial and portal phases, it was able to identify active bleeding and its location in 10 out of 27 of these cases. Other publications have reported similar results; therefore, CT should be considered the diagnostic test of choice.5 Out of the 27 spontaneous RSH diagnosed by CT, 10 were in arterial phase and the remainder in venous phase. This enabled us to conduct selective embolisation after arteriography in the patients with positive CT angiography. Patients with a venous origin responded favourably to non-surgical treatment.
Treatment of RSH should be based on the replacement of blood loss, transfusion of blood products and the correction of anticoagulation. But we should also emphasise the contribution of arterial embolisation of the bleeding artery, which is indicated according to the findings of a CT angiogram. In our series, haemostasis of the bleeding vessel was achieved and the progression of the haematoma was halted in all patients in whom it was applied (8 patients). With these actions, 32 of the 34 patients progressed satisfactorily. In a review of the literature, we have found no clinical guidelines or recommendations for the management and treatment of RSH. Some authors propose specific algorithms aimed at diagnosing RSH and recommend certain imaging tests.13,18
In our review of the literature, we have found no clinical guidelines that recommend the best time to reinstate the use of anticoagulant therapy. In accordance with authors Witt and Kunkula, and after individualising the cases, it seems reasonable to reinitiate anticoagulant medication between the 4th and 7th days after the diagnosis of RSH, as this reduces the number of thrombotic phenomena and the recurrence of haemorrhages.11,19
The efficacy of embolisation to stop the haemorrhage in cases of spontaneous RSH has been discussed in some publications.20,21 According to certain authors, RSH arise as a consequence of multifactorial diffuse microvascular conditions involving several collateral complexities.22 In our experience, this is not completely true, as we have observed that there is usually a main vessel responsible. In addition, with more precise materials used in interventional radiology, such as coils or microcoils, effective embolisation is achieved.
We believe that surgery to drain the haematoma and achieve haemostasis should be the last resort, used only after the failure of the other therapeutic options.23 Our series did not record good progress after surgical intervention in these patients. Published data indicate that spontaneous RSH present low mortality (close to 4%), although in patients treated with anticoagulation this rate can reach 25%.1,24 Authors like Dag et al.25 have published series with overall mortality rates of between 9 and 67% for patients with RSH who are treated surgically. In our series, overall mortality was 6%, while the mortality rate of the patients who underwent surgery was 100%.
In conclusion, spontaneous RSH are usually detected by the presence of abdominal pain and a palpable mass. They are more frequent in women of advanced ages who are being treated with oral anticoagulants. Most patients progress favourably with non-surgical treatment. CT angiography provides better diagnostic information than ultrasound and, moreover, it facilitates later selective arterial embolisation in cases of active bleeding.
Authorship/CollaboratorsStudy design: Fernando Mendoza Moreno, Enrique Ovejero Merino, Rafael Villeta Plaza, Ana María Minaya Bravo.
Data collection: Fernando Mendoza Moreno, Diego Martín Córdova García, Ana María Minaya Bravo.
Data analysis and interpretation: Fernando Mendoza Moreno, Diego Martín Córdova García, Javier Granell Vicent.
Drafting of the article: Fernando Mendoza Moreno, Enrique Ovejero Merino, Rafael Villeta Plaza, Manuel Díez Alonso.
Critical review and approval of the final version: Rafael Villeta Plaza, Manuel Díez Alonso, Francisco Javier Granell Vicent.
Conflict of InterestsThe authors of the manuscript have no conflicts of interest.
Please cite this article as: Mendoza Moreno F, Díez Alonso M, Villeta Plaza R, Minaya Bravo AM, Ovejero Merino E, Córdova García DM, et al. Hematoma espontáneo del músculo recto anterior del abdomen. Cir Esp. 2016;94:294–299.