Non-operative treatment (NOM) of splenic trauma is the management of choice in hemodynamically stable patients. Aim of the present study was to assess the failure rate of the NOM after implantation of a multidisciplinary protocol for splenic injuries comparing the results with the literature.
Methods16-year retrospective study. Management of these lesions was recorded according to our hospital protocol: demographic data, blood pressure, respiratory rate, Glasgow Coma Scale(GCS), Revised Trauma Score(RTS), Injury Severity Score(ISS), grades of injuries according to the American Association for the Surgery of Trauma(AAST), failure of the NOM, morbidity and mortality.
Results110 patients were included, 90 (81.8%) men, 20 (18.2%) women; mean age 37 years; 106 (96.5%) cases were blunt and four (3.5%) penetrating by knife. The diagnosis was established by US/CT. AAST classification: 14 (13%) patients were grade I; 24 (22%) grade II; 34 (31%) grade III; 37 (34%) grade IV. Emergency laparotomy was performed in 54 patients: 37 due to grade IV injuries, 17 due to hemodynamic instability. NOM was established in 56, conservative surgery in 16 and splenectomy in 38. Ten patients presented postoperative complications: seven in the splenectomy group, two in the conservative surgery group and one in non-operative group. One patient died. Average hospital stay: 22.8 days- TNO 17.6 days, conservative surgery 29, splenectomy 22.4 days.
ConclusionsAlthough we continue with a high hospital stay, our results are comparable to the literature. The implementation of the protocol by consensus contributed to the change towards NOM.
El tratamiento no operatorio (TNO) de los traumatismos esplénicos es el manejo de elección en pacientes estables hemodinámicamente. El objetivo del presente estudio fue valorar la tasa de fracaso del TNO tras la implantación de un protocolo multidisciplinar para las lesiones esplénicas y comparar los resultados con la literatura.
Métodosestudio retrospectivo, 16 años de duración. Se registró el manejo de estas lesiones según nuestro protocolo hospitalario, datos demográficos, tensión arterial, frecuencia respiratoria, escala de Coma de Glasgow (GCS), Revised Trauma Score (RTS), Injury Severy Score (ISS), gradación de las lesiones según la American Association for the Surgery of Trauma (AAST), fracaso del TNO, morbilidad y mortalidad.
ResultadosSe incluyeron 110 pacientes, 90 (81,8%) varones (81,8%), 20 (18,2%) mujeres; edad media 37 años; 106 (96,5%) casos fueron contusos y cuatro (3,5%) penetrantes por arma blanca. El diagnóstico se estableció mediante ECO/TAC. Clasificación AAST, 14 (13%) pacientes fueron grado I; 24 (22%) grado II; 34 (31%) grado III; 37 (34%) grado IV. Se realizó laparatomía de urgencia en 54 pacientes: 37 por lesiones grado IV y 17 por inestabilidad hemodinámica. En 56 pacientes se instauró TNO, cirugía conservadora en 16 y esplenectomía en 38. Diez pacientes presentaron complicaciones postoperatorias: siete en el grupo de esplenectomía, dos en el grupo de cirugía conservadora y uno en el de tratamiento no operatorio (que requirió intervención por fracaso en TNO). La mortalidad fue un paciente. Estancia media: 22,8 días- TNO 17,6 días, cirugía conservadora 29, esplenectomía 22,4 días.
ConclusionesSi bien continuamos con una estancia hospitalaria elevada, nuestros resultados son comparables a la literatura. La implantación consensuada del protocolo contribuyó al cambio hacia TNO.
Non-operative management (NOM) of splenic trauma continues to be the cornerstone of the management of patients with splenic injuries who are hemodynamically stable.1 This trend towards splenic preservation is due to the important immunological functions of the spleen (which eliminates the risk of post-splenectomy sepsis) as well as the accumulated experience, mainly in pediatric surgery, demonstrating that complete healing of the organ and total recovery of its immunological function are possible.2,3 Furthermore, splenectomy is not an innocuous procedure, and it has been related with an increase in blood loss and the need for transfusions, the formation of postoperative abscesses of the residual splenic cavity and the increase in sepsis mortality in splenectomized patients.3 In addition, the development of multidisciplinary protocols involving radiologists, intensivists and surgeons has contributed significantly to this change in approach.3,4 The objective of this study was to assess the NOM failure rate after the implementation of a multidisciplinary protocol for splenic trauma.
MethodsSince 2003, there is a multidisciplinary hospital protocol for the management of patients with splenic trauma, which was developed by surgeons, emergency physicians, anesthesiologists, radiologists and intensivists.
After obtaining the authorization of the Ethics Committee of the Hospital Clínico Universitario San Cecilio, this retrospective study was prepared reviewing the medical files of all the patients treated in the Emergency Department between January December for this disease. The diagnostic-therapeutic approach was recorded (demographic data, blood pressure, respiratory rate, Glasgow Coma scale [GCS], Revised Trauma Score [RTS], Injury Severity Score [ISS], trauma injury score according to the American Association for the Surgery of Trauma [AAST], failure of the NOM, morbidity, mortality). The protocol was based on classifying patients by the degree of hemodynamic stability according to the Advanced Trauma Life Support (ATLS) guidelines, which evaluates blood pressure, Glasgow Coma Scale (GCS), respiratory rate. These clinical parameters are added to obtain the triage Revised Trauma Score (RTS). An RTS equal to or less than 2003| 2018| 3| 10, entails a mortality rate greater than 30%(demographic data, blood pressure, respiratory rate, Glasgow Coma scale [GCS], Revised Trauma Score [RTS], Injury Severity Score [ISS], trauma injury score according to the American Association for the Surgery of Trauma [AAST], failure of the NOM, morbidity, mortality)(ATLS)(GCS)(RTS), therefore, this type of patients should be, transferred to a referral hospital center that has 24-h surgical, radiology services, etc.5 Splenic trauma injuries were classified by the American Association for the Surgery of Trauma Organ Injury Scale4which establishes 5, degrees of injury, from lesser to greater severity.
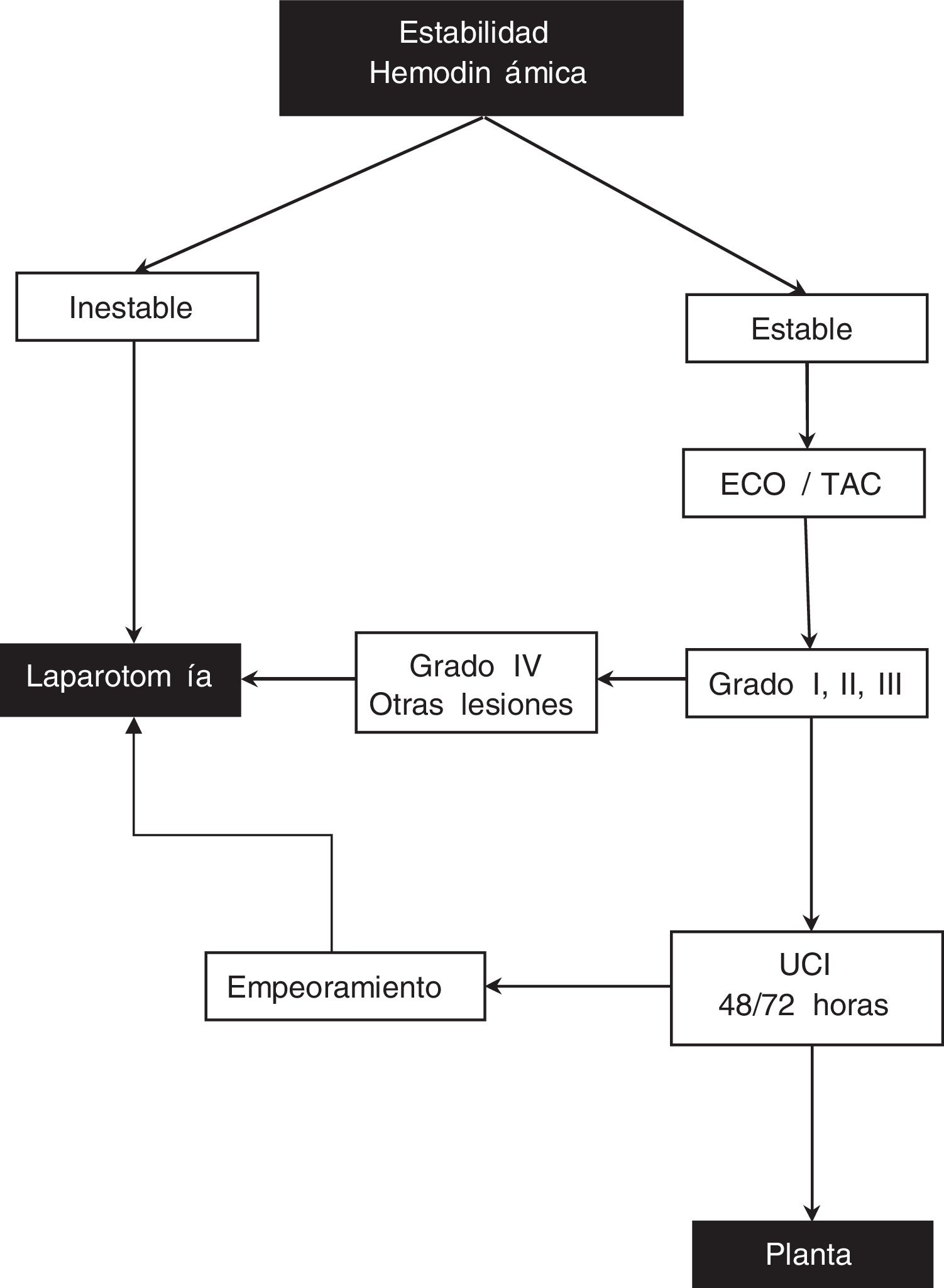
When a patient arrives at the ER with abdominal trauma, our actions are based on the following protocol (Fig. 1):
- 1)
Unstable patient, systolic blood pressure <90 mmHg, profuse sweating, cold skin, tachycardia, weak radial pulse, polypnea and oliguria or suspicion of other injuries: laparotomy.
- 2)
Hemodynamically stable patient, negative or doubtful abdominal examination, hematocrit >25% or mild trauma: perform ultrasound/CT scan. If grade IV splenic injury or if there are more visceral injuries, laparotomy is performed. In the case of grade I, II, III splenic injuries, patients are managed conservatively in an intensive care unit for 48–72 h, with complete blood count every 4–6 h/48 h and then daily, nasogastric tube until peristalsis begins, bed rest 3–5 days and hospitalization for 7–10 days. If during that time the patient worsens or needs more than one transfusion, laparotomy is performed. Laparoscopy is not part of the management protocol for these patients.
All the data obtained through the collection of the variables defined (demographic data, blood pressure, respiratory rate, GCS, RTS, ISS, AAST grade, NOM failure, morbidity and mortality) were analyzed statistically by comparing the different groups formed using SPSS 21 software and the ANOVA statistical test.
ResultsFollowing our protocol, 110 patients were included, 90 of which were men (81.8%) and 20 women (18.2%). Mean age was 37 years (24–65). In 106 cases (96.5%) of splenic injury, the etiology was blunt abdominal trauma; 4 cases of knife stabbings (3.5%) were also recorded. The diagnosis of the injuries was established by ultrasound/CT.
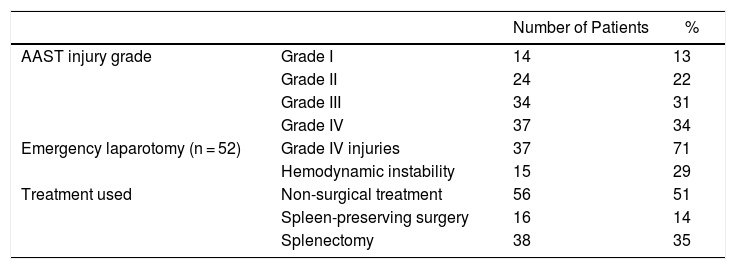
According to the splenic injury classification of the AAST, 14 (13%) patients had grade I injuries, 24 (22%) grade II injuries, 34 (31%) grade III injuries and 37 (34%) grade IV injuries. In 54 patients, the initial approach was emergency laparotomy, specifically in patients with grade IV lesions (n = 37) diagnosed by ultrasound/CT and in those who were hemodynamically unstable (n = 15). In these patients, the following associated injuries were found: one case of head of the pancreas injury, 12 cases of renal injuries (3 hematomas treated with conservative treatment; the rest required nephrectomy), one case of mesocolon tear, one case of laceration to the abdominal aorta, and one case of hepatic laceration, with the resulting segmentectomy of the affected segment. In terms of patients with associated lesions in the thoracoabdominal area, rib fractures (30 patients) and pulmonary contusions (6 patients) stand out. In no case was there a need to transfer the patient to a referral hospital because the injuries were resolved with conservative management. Moreover, these injuries were not related to the laparotomy used to perform the splenectomy (either partial or total), or with the age or comorbidity of the patients, but instead with the mechanism of the abdominal trauma itself (in all the cases blunt abdominal trauma). There were 22 patients in total who presented a solitary splenic injury (36%).
With regard to treatment, 56 patients (51%) were managed with NOM, spleen-preserving surgery was conducted in 16 patients (14.5%) (vicryl mesh, partial splenectomy, splenorrhaphy), and splenectomies were done in 38 (34.5%). We did not include embolization in any of the possible treatment branches of the study because interventional radiology was not available 24/7 at these facilities. The mortality rate was one patient (1.6%), a 67-year-old male with no personal history of interest, who had blunt abdominal trauma from a car accident; in addition to the grade IV splenic injury, the patient presented a torn mesosigmoid, several fractured ribs, complex pelvic fracture and a contained aortic laceration. The patient underwent emergency surgery while hemodynamically unstable, and splenectomy was performed along with the placement of an aortic stent. He died within hours of surgery due to septic shock, oliguria and acute renal failure. Out of the total patients, 10 (17.5%) had postoperative complications: 7 in the splenectomy group, 2 in the spleen-preserving surgery group and one in the nonoperative treatment group (due to later splenic rupture).
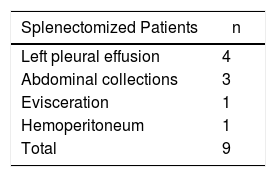
In splenectomized patients, the most frequent complication was left pleural effusion (n = 4), followed by postoperative collections (n = 3), evisceration (n = 1) and hemoperitoneum (n = 1). There were no notable complications in the spleen-preserving group, and the case of later rupture in a single case of NOM is striking (Table 1). The average hospital stay was 22.8 days (3–42): NOM 17.6 days (3–10), spleen-preserving surgery 29 days (3–42) and splenectomy 22.4 days (4–30) (Table 2).
Management According to the Spleen Injury Scale.
| Number of Patients | % | ||
|---|---|---|---|
| AAST injury grade | Grade I | 14 | 13 |
| Grade II | 24 | 22 | |
| Grade III | 34 | 31 | |
| Grade IV | 37 | 34 | |
| Emergency laparotomy (n = 52) | Grade IV injuries | 37 | 71 |
| Hemodynamic instability | 15 | 29 | |
| Treatment used | Non-surgical treatment | 56 | 51 |
| Spleen-preserving surgery | 16 | 14 | |
| Splenectomy | 38 | 35 |
Classically, urgent laparotomy was considered the standard procedure to treat blunt abdominal trauma. This approach was based on concepts from the beginning of the last century, such as those described by Kocher,6 who established that splenic trauma required splenectomy to stop bleeding and that this was not associated with detrimental effects. In the same context, Pringle7 established the same behavior for major splenic injuries. However, these concepts have been changing, especially in recent decades, and today the frequency of NOM has increased to 40%-80%, depending on the series.8,9
This evolution has been due to several factors, including the demonstrated possibility of post-splenectomy sepsis,10 the high morbidity and mortality of the surgical treatment of severe splenic trauma11,12 and the fact that in 20%-30% of patients treated with laparotomy due to hemorrhage this would have cedido at the time of surgery.12–14 This led to the indication for immediate surgical indication being rethought. Furthermore, the increased availability and advances in more accurate radiodiagnostic techniques for classifying the degree of injury, as well as its evolution, have contributed to the development of NOM, providing good results.4
The treatment approach for splenic trauma injuries depends on a number of factors, the most important of which is the degree of hemodynamic stability. The ATLS defines instability based on the score introduced by Champion et al.: RTS (blood pressure, GCS and respiratory rate),3,4 age, analytical parameters and classification1/grade of splenic injury, as well as the presence of associated injuries. Unstable patients or those with evidence of bleeding should be taken to the operating room to complete resuscitation and perform surgery.14 Technical improvements in imaging and radiodiagnostic methods can accurately assess the degree of trauma, adapt the conservative treatment of solid organ injuries, and thereby avoid unnecessary laparotomies while monitoring patients.4
A multicenter study by the Eastern Association for the Surgery of Trauma found that surgical treatment decreased from 52% in 1993 to 39% in 1997. NOM failed in 10.8% of cases, 60.9% in the first 24 h, 13.8% on the second day, 6.9% on the third day and 4.6% on the fourth day post-trauma. This was mainly related to the degree of injury, as confirmed by other studies.15–17
Our hospital also changed its approach to treat splenic trauma injuries. In 2003, we published a series of 26 patients14 who underwent 16 splenectomies (61.5%), 5 spleen-preserving procedures (19.2%) and NOM in 5 patients (19.2%). In a series of cases diagnosed from 2003 to 2018, splenectomy decreased (to 39.3%), as did spleen-preserving surgery (to 13.1%) in favor of NOM, which increased to 47.5% of cases. It should be noted that ours is a specialty hospital and is less than 300 m from a regional hospital, so the number of patients with polytrauma is lower than in other hospitals at the same level, and treated patients are less severe in terms of RTS.
Currently, the initial therapeutic approach in pediatric patients and adults is directed towards non-surgical treatment.2,3 In well-selected patients, the probability of success in children is 92%18,19 and 75%-90% in adults.20,21 The rate of NOM in adults is close to 50% of cases, and the splenectomy rate has decreased significantly. In our series, it was approximately 49% of cases in adults (no pediatric cases were registered). The spleen preservation rate with combined NOM and conservative surgery was between 40% and 75%, with an average overall rate in adults of 55%.3 In our study, the current percentage was 65%.
The percentage of patients who undergo splenorrhaphy ranges from 17% to 35%. However, the overall splenic preservation rate has increased with the use of absorbable mesh to 67%. In cases of penetrating trauma injuries, according to the degree of severity, rates have reached up to 92% for grade III and 37% for grade IV. The conversion rate of conservative to surgical treatment in children is 0.4%-1.8%, while in adults this figure ranges between 6% and 19%. The failure rate of simple splenorrhaphy is between 1.3% and 4%. There is a striking lack of data in the literature for failure rates in patients treated with splenorrhaphy and prosthetic material, although the majority of series indicate the absence of re-bleeding and the need for re-operations.3 In our series, 4 vicryl mesh (6.6%) were used, and a TachoSil local hemostatic agent was applied in one patient (1.6%). These were grade III splenic lesions in all 5 patients. The complication rate was lower in the group of splenectomized patients, although in other series and literature reviews the rate of overall morbidity, mortality and hospital costs were lower in patients with non-surgical management.22 Due to the number of patients of our study, we cannot make a categorical statement.
In conclusion, although we continue to have a long hospital stay, which is perhaps influenced by an extremely cautious approach with prolonged direct observation and imaging tests that could be done on an outpatient basis, our results are comparable to others reported in the literature. The definition of appropriate criteria and the existence of multidisciplinary action protocols mean that more and more surgeons are more prone to preserving the spleen, whose functions have not always been appreciated. In our experience, the consensus protocol has contributed to a change in approach in favor of conservative management.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Zurita Saavedra M, Pérez Alonso A, Pérez Cabrera B, Haro García AM, Ruiz García VM, Mirón Pozo B, et al. Resultados en el tratamiento de traumatismos esplénicos utilizando un protocolo multidisciplinar en 110 pacientes consecutivos en un hospital de nivel II. Cir Esp. 2020;98:143–148.