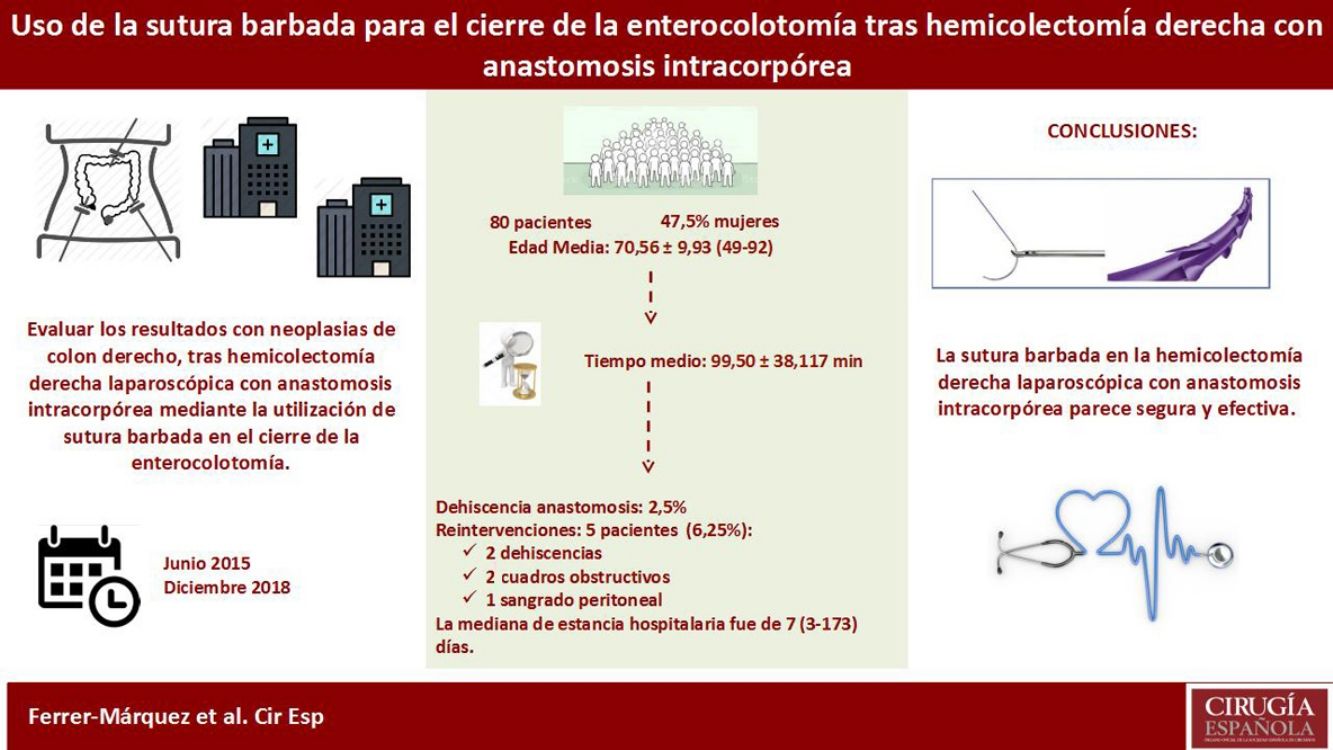
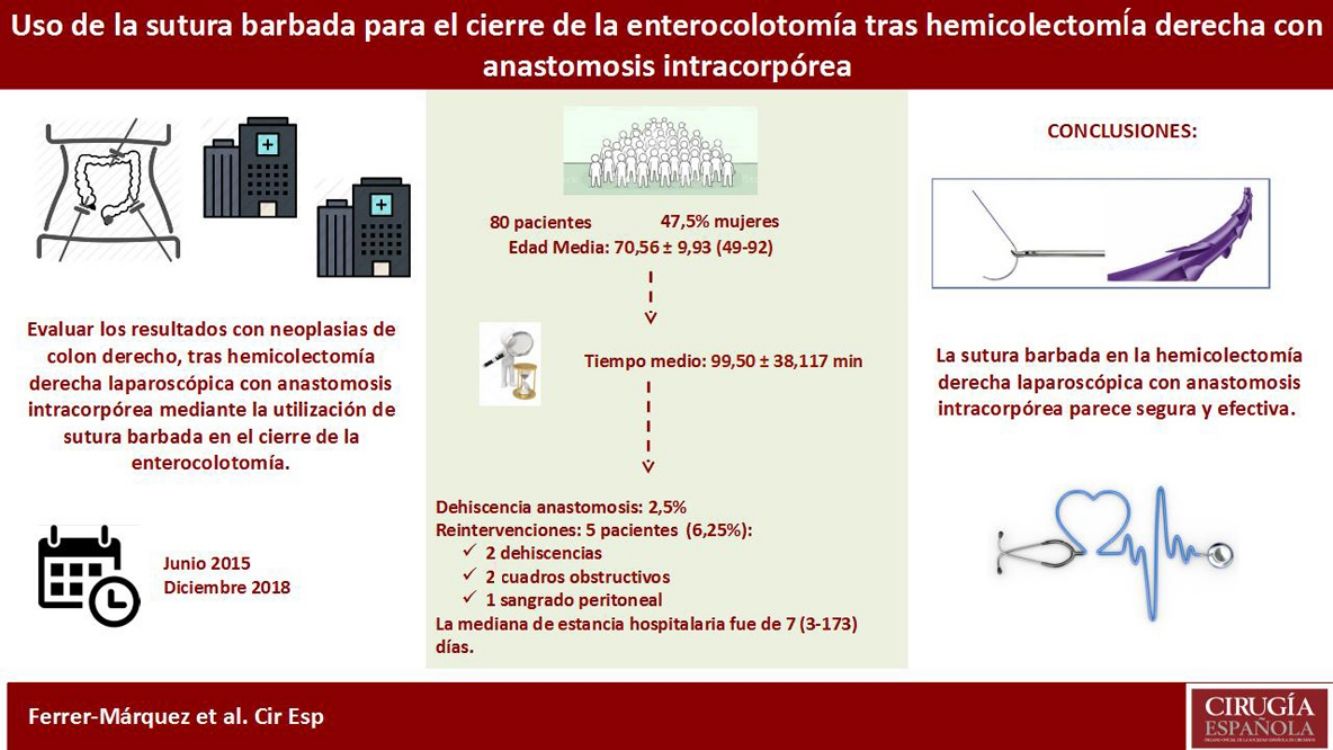
Performing intracorporeal anastomoses and sutures is possibly the technique that requires the greatest skill in laparoscopic surgery. The appearance of the new barbed sutures in recent years has seemed to facilitate this surgical step. The aim of our study is to evaluate short-term results in patients with neoplasms of the right colon, after laparoscopic right hemicolectomy with intracorporeal anastomosis using barbed suture at the closure of the enterocolotomy.
Patients and methodsThis is a multicenter, prospective, descriptive study that includes patients who underwent laparoscopic right hemicolectomy for neoplastic colonic pathologies between June 2015 and December 2018. In all patients, the intracorporeal anastomosis was performed using the endocutter, and closure of the enterocolotomy was done with a double layer of barbed suture.
ResultsA total of 80 patients were treated (47.5% women), with an average age of 70.6 ± 9 (49–92) years. The average operative time was 99.5 ± 38 min. Anastomotic dehiscence was observed in 2.5% of the sample, and 5 patients required re-operation (6.2%) as a result of two leaks, two obstructive symptoms and one peritoneal bleeding. Mean hospital stay was 7 (3–173) days.
ConclusionsThe use of barbed suture in laparoscopic right hemicolectomy with intracorporeal anastomosis seems to present a morbidity similar to series described in literature. Prospective, controlled and randomized studies with a larger number of patients would be necessary to confirm these findings.
Posiblemente la parte técnica que más destreza precisa en laparoscopia es la realización de anastomosis y suturas intracorpóreas. La aparición de las nuevas suturas barbadas durante los últimos años parece facilitar dichos gestos quirúrgicos. El objetivo de nuestro estudio es evaluar los resultados a corto plazo en pacientes con neoplasias de colon derecho, tras hemicolectomía derecha laparoscópica con anastomosis intracorpórea mediante la utilización de sutura barbada en el cierre de la enterocolotomía.
MétodosSe trata de un estudio descriptivo prospectivo multicéntrico en el que se incluyen pacientes que han sido intervenidos mediante hemicolectomía derecha laparoscópica por patología neoplásica colónica entre junio de 2015 y diciembre de 2018. En todos ellos se realizó la anastomosis intracorpórea mediante el uso de endocortadora, y el cierre de la enterocolotomía mediante una doble capa de sutura barbada.
ResultadosSe han intervenido un total de 80 pacientes (47,5% mujeres), con una edad media de 70,6 ± 9 (49–92) años. El tiempo operatorio medio fue 99,5 ± 38 minutos. Un 2,5% de la muestra presentó dehiscencia de anastomosis, y se tuvieron que reintervenir 5 pacientes (6,2%) como consecuencia de dos dehiscencias, dos cuadros obstructivos y un sangrado peritoneal. La mediana de estancia hospitalaria fue de 7 (3–173) días.
ConclusionesEl uso de la sutura barbada en la hemicolectomía derecha laparoscópica con anastomosis intracorpórea parece presentar una morbilidad similar a las series descritas en la literatura. En cualquier caso, serían necesarios estudios con mayor número de pacientes, prospectivos, controlados y aleatorizados para confirmar estos hallazgos.
Since the debut of laparoscopic colorectal surgery, numerous studies have demonstrated its advantages in terms of safety and effectiveness. Compared to open surgery, patients undergoing laparoscopic surgery have an earlier recovery and fewer short-term complications,1 without presenting differences in terms of cancer outcomes, survival or recurrence.2
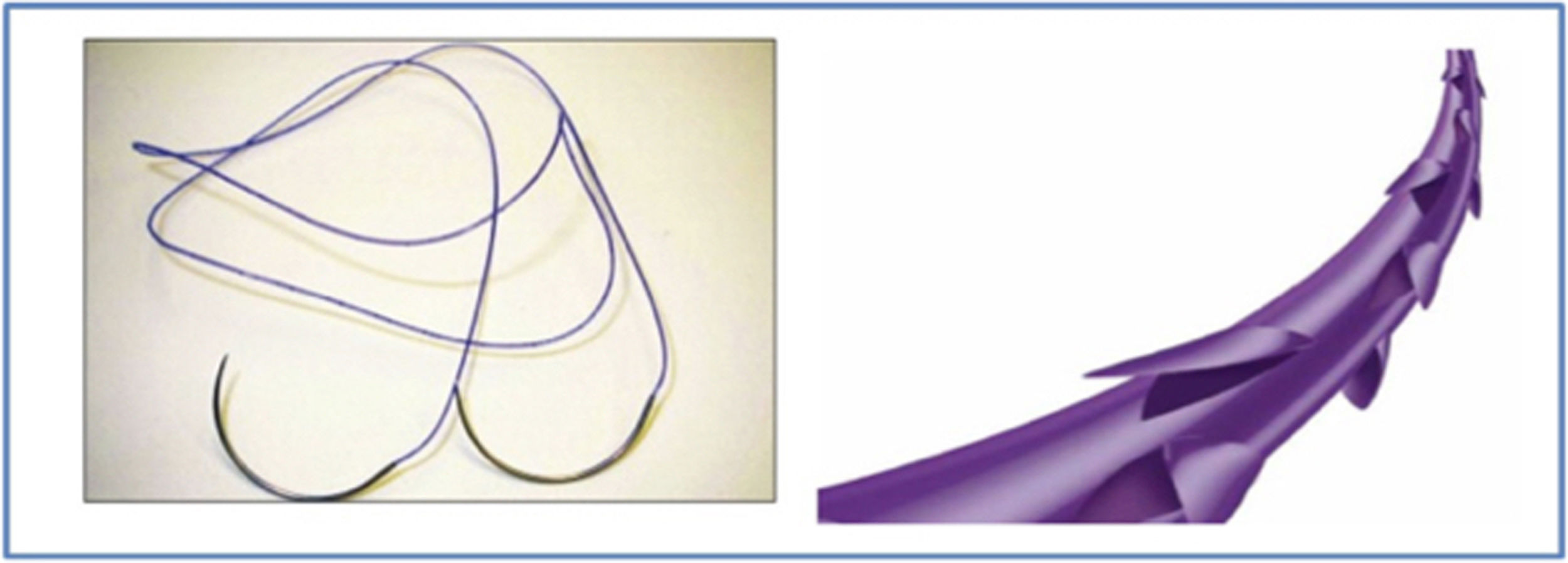
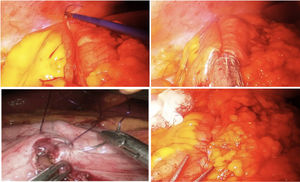
The laparoscopic right hemicolectomy technique for the treatment of colonic lesions can be done by either creating the anastomosis after exteriorization of the intestine through a minilaparotomy (extracorporeal anastomosis), or by performing a totally laparoscopic intra-abdominal anastomosis (intracorporeal anastomosis). To date, different articles have compared both techniques, although there are no clear differences between the two to indicate which is currently the best.3–7 Despite this, the latest meta-analyses seem to defend intracorporeal anastomosis and identify certain advantages over the extracorporeal method, such as earlier recovery and fewer postoperative complications.8–10 The advent of barbed suture in recent years seems to facilitate the creation of these anastomoses. The clinical review of the literature supports its use as a safe and effective technique, which at the very least is equivalent to conventional absorbable sutures11 (Fig. 1).
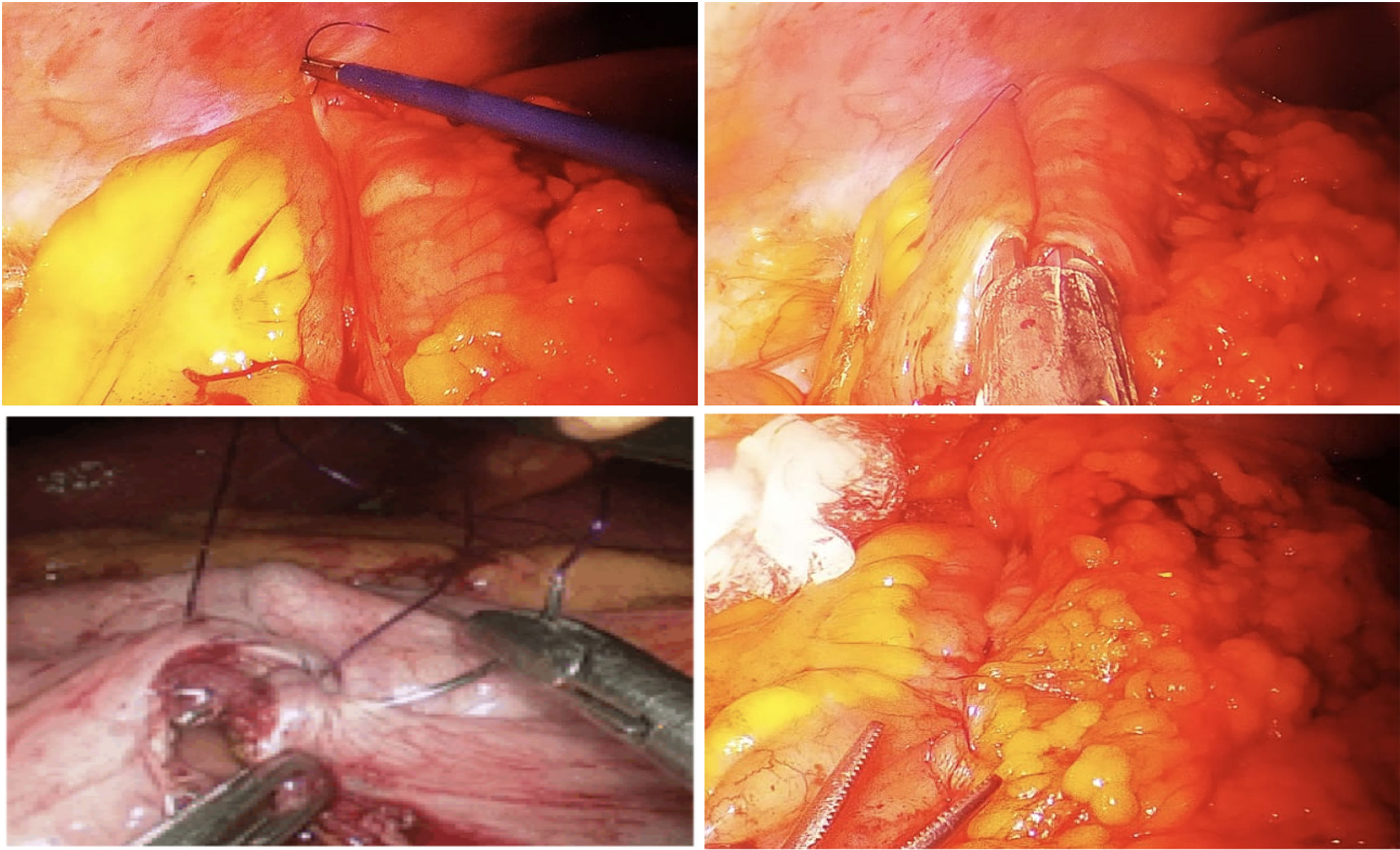
The objective of our study is to evaluate the short-term results in patients with right colon cancer after laparoscopic right hemicolectomy with intracorporeal anastomosis using barbed suture at the closure of enterocolotomy (Fig. 2).
MethodsStudy DesignThis is a prospective multicenter descriptive study including patients who have undergone laparoscopic right hemicolectomy surgery with intracorporeal anastomosis for colon cancer from June 2015 to December 2018. The study has been assessed and approved by the ethics committees of the participating hospitals (3 hospitals in southeastern Spain). All patients gave their informed consent to participate in the study.
Patients diagnosed with neoplasm of the right colon (cecum, ascending colon and hepatic flexure) were included in the study. The exclusion criteria were: the existence of synchronous neoplastic lesions in the colon, distant metastasis (stage IV), invasion of neighboring organs (T4) at the time of diagnosis, patients with Crohn’s disease or ulcerative colitis, emergency surgery and contraindication for laparoscopic surgery. Patients who had an extracorporeal anastomosis for whatever reason were likewise excluded from the study.
The main variables to be measured were patient characteristics (sex, age, location of the lesion), intraoperative (surgical time, percentage of conversion, size of the incision to remove the surgical specimen, complications), postoperative (days to introduce intake, presence of paralytic ileus, hospital stay, reoperation, complications, mortality).
Surgical TechniquePatients received preoperative antibiotic and antithrombotic prophylaxis, as well as colon preparation with a low-residue diet during the week prior to the intervention. The patients were operated on under general anesthesia and in a French position (Trendelenburg position with open legs). The procedure began with the placement of an initial infraumbilical trocar measuring 12 mm and the subsequent placement of 3 accessory ports (5 mm × 5 mm × 12 mm).
Complete exploration of the abdominal cavity was conducted in search of the primary tumor, distant lesions or peritoneal implants. The ileocolic vessels were exposed and, after their resection, the dissection continued medial to lateral. Once the mesocolon was dissected, we decided where to dissect the transverse colon with the endocutter (endoGIA1 60 mm Articulating Medium/Thick Reload with Tri-Staple Technology 3 mm, 3.5 mm, 4 mm —EGIA60AMT—, Medtronic, Minneapolis, USA), and dissection was completed by mobilizing the hepatic flexure. Subsequently, the terminal ileum was identified and divided at about 10 cm from the ileocecal valve with an endocutter (endoGIA1 60 mm Articulating Vascular / Medium Reload with Tri-Staple Technology 2 mm, 2.5 mm, 3 mm —EGIA60AVM—, Medtronic, Minneapolis, U.S.). The right paracolic dissection was completed when the surgical piece was completely released.
A Pfannenstiel incision was made for the extraction the surgical specimen, protected with an Alexis® type separator (Alexis® or Wound Retractor/Protector, Applied Medical Technology, CA, USA).
The terminal ileum was placed next to the transverse (isoperistaltic) colon to create a side-to-side anastomosis, placing a traction suture proximal to the anastomosis and joining the edge of the colon and the ileum. Afterwards, buttonholes were opened to introduce the endocutter (endoGIA1 60 mm Articulating Medium/Thick Reload with Tri-Staple Technology 3 mm, 3.5 mm, 4 mm —EGIA60AMT— Medtronic, Minneapolis, USA). The anastomosis was created and the enterocolotomy was closed. To do so, a few stitches were made with 2-0 barbed suture at the distal end and inferior to the buttonhole (as a point of reference), then proceeding with the closure using continuous 2-0 barbed double suture (the first sero-submucosal and the second sero-serosa) (PDO 26 mm, 1/2 circle). After performing the suture, knotting is not necessary and the thread was cut approximately 0.5−1 cm from the end. None of the ends (colon or ileum) were oversutured. The abdominal cavity was checked. If necessary, a suction drain was placed (the surgeon’s decision).
Follow-upThe urinary catheter was removed on the first postoperative day (when diuresis was adequate). All patients began to move to a chair and even walk from day one. If there was peristalsis or flatulence, oral intake was initiated with liquids. If the liquid diet was well tolerated, intake was gradually increased to semi-liquid and soft foods. Surgical drains were withdrawn after 24 h if the discharge was serous or serosanguineous. The criteria for discharge are: solid foods are tolerated; mobilization is adequate; flatulence; no nausea; patient acceptance; no abdominal pain, or pain controlled with oral analgesia.
Statistical AnalysisThe statistical analysis was performed with SPSS 20.0 software (IBM Inc. Rochester, MN, USA). A descriptive analysis was conducted of the collected study variables.
For the qualitative variables, frequencies were calculated; for the quantitative variables, standard deviation measures of dispersion were calculated.
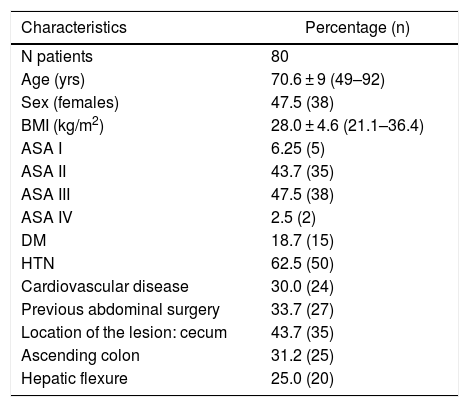
ResultsA total of 80 patients were treated surgically between June 2015 and December 2018. The characteristics of the population studied are shown in Table 1. The average age of the sample was 70.6 ± 9 (49–92) years. The average body mass index was 28.0 ± 4 (21.1–36.4) kg/m2. Regarding the location of the neoplastic lesions, 43.7% were in the cecum, 31.2% in the ascending colon and 25% in the hepatic flexure.
Characteristics of Patients in the Study.
| Characteristics | Percentage (n) |
|---|---|
| N patients | 80 |
| Age (yrs) | 70.6 ± 9 (49–92) |
| Sex (females) | 47.5 (38) |
| BMI (kg/m2) | 28.0 ± 4.6 (21.1–36.4) |
| ASA I | 6.25 (5) |
| ASA II | 43.7 (35) |
| ASA III | 47.5 (38) |
| ASA IV | 2.5 (2) |
| DM | 18.7 (15) |
| HTN | 62.5 (50) |
| Cardiovascular disease | 30.0 (24) |
| Previous abdominal surgery | 33.7 (27) |
| Location of the lesion: cecum | 43.7 (35) |
| Ascending colon | 31.2 (25) |
| Hepatic flexure | 25.0 (20) |
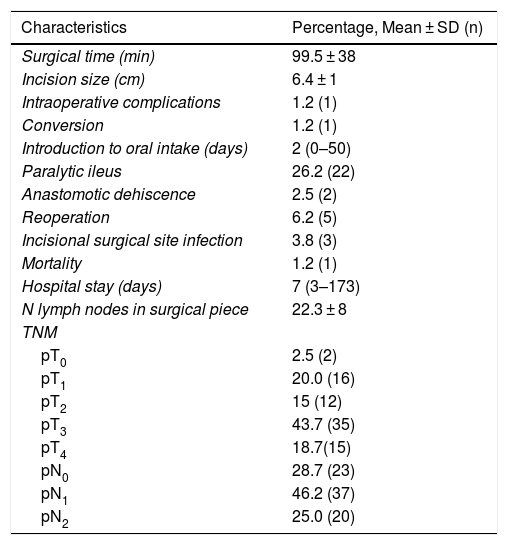
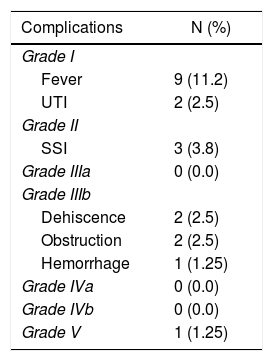
Intraoperative variables are shown in Table 2. The mean surgical time of the intervention was 99.5 ± 38 min. In the postoperative period, 26.2% of the sample presented paralytic ileus, which delayed the introduction of oral intake (median 2 days [0–50]). The percentage of overall complications in the series was 25% (Table 3). Anastomotic dehiscence was observed in 2.5% of the sample, and 5 patients (6.2%) had to be reoperated as a result of 2 dehiscences, 2 symptoms of obstruction and one peritoneal bleeding. All patients were reoperated by laparoscopy and 3 were converted to laparotomy. Among the patients with anastomotic dehiscence, a leak occurred at the edge of the small intestine dissection and was treated by resection of this stump. In the second case, the leak occurred on the mechanical suture line. The obstructive symptoms were due to an internal hernia and an intestinal loop adhered in the pelvis. Both cases were converted to laparotomy and were resolved without the need for intestinal resection. Superficial surgical site infection occurred in 3.8% of cases. There was one death in the series due to pulmonary thromboembolism. The median stay in the series was 7 (3–173) days. Regarding the pathology results, 28 patients were stage I, 10 patients stage IIA, 24 stage IIIA and 16 stage IIIB.
Intra- and Postoperative Variables.
| Characteristics | Percentage, Mean ± SD (n) |
|---|---|
| Surgical time (min) | 99.5 ± 38 |
| Incision size (cm) | 6.4 ± 1 |
| Intraoperative complications | 1.2 (1) |
| Conversion | 1.2 (1) |
| Introduction to oral intake (days) | 2 (0–50) |
| Paralytic ileus | 26.2 (22) |
| Anastomotic dehiscence | 2.5 (2) |
| Reoperation | 6.2 (5) |
| Incisional surgical site infection | 3.8 (3) |
| Mortality | 1.2 (1) |
| Hospital stay (days) | 7 (3–173) |
| N lymph nodes in surgical piece | 22.3 ± 8 |
| TNM | |
| pT0 | 2.5 (2) |
| pT1 | 20.0 (16) |
| pT2 | 15 (12) |
| pT3 | 43.7 (35) |
| pT4 | 18.7(15) |
| pN0 | 28.7 (23) |
| pN1 | 46.2 (37) |
| pN2 | 25.0 (20) |
The treatment of neoplasms of the right colon has evolved towards the use of laparoscopic procedures, thereby achieving the benefits that this minimally invasive approach provides.12–16 However, this surgical technique involves controversies, including which of the possible anastomoses is the most appropriate (extracorporeal or intracorporeal). To date, several publications have tried to demonstrate which is more advantageous, but, although certain studies advocate one or the other, definitive conclusions cannot be drawn.3–7 The meta-analysis by Feroci et al.16 shows that there are no statistically significant differences between the techniques in operative time, postoperative complications, reoperations, number of isolated lymph nodes in the surgical piece and mortality. However, the systematic review carried out by van Oostendorp et al.8 concludes that intracorporeal anastomosis is associated with a reduction in short-term morbidity (OR 0.68, 95% CI, 0.49-0.93; I2 = 20%), as well as a shorter hospital stay (mean –0.77 days, 95% CI, –1.17-0.37; I2 = 4%).
Proponents of intracorporeal anastomosis rely on the fact that the technique provides adequate visualization along the entire length. With regards to extracorporeal anastomosis, depending on the characteristics of the patient, the extraction of the intestinal ends for the anastomosis is sometimes complicated, especially in obese subjects.17 In addition, it provides correct visualization of the mesentery to prevent its rotation, which may lead to postoperative complications due to vascular compromise (more frequent in the extracorporeal technique18). On the other hand, intracorporeal anastomosis allows you to decide where you want to make the extraction incision of the surgical piece (McBurney, right hypochondrium, Pfannenstiel, etc.). This is unlike the extracorporeal method, in which the incision must be made in the area that provides the extraction of both ends, requiring, in certain patients, longer incisions than in the intracorporeal type.19 In our series, intracorporeal anastomosis has allowed us to extract the surgical pieces through Pfannenstiel incisions. Regarding the orientation of the anastomosis, the intracorporeal method allows us to decide whether the anastomosis is performed iso- or antiperistaltic.20 During our study, all anastomoses were isoperistaltic.
One of the main drawbacks of intracorporeal anastomosis is that it requires a significant level of skill from a technical point of view, mainly to perform the enterocolotomy suture. This was shown by Jamali et al.21 in their study about the degree of difficulty of different laparoscopic techniques, which shows evidence that intracorporeal anastomosis presents more difficulties for surgeons than the extracorporeal technique. Therefore, in our study we present the use of barbed suture in order to demonstrate its advantages in terms of surgical ease.
Since the introduction of barbed sutures, their use has spread to various specialties.22–28 Although these types of sutures are approved for use in soft tissues, their safety and effectiveness have not been approved in intestinal anastomosis. However, the number of publications about them is growing every day. Most of the studies published during recent years are related to bariatric surgery and the use of barbed sutures in laparoscopic gastric bypass.11,29–31 Recently, their use has been described in colorectal surgery, where barbed sutures have been used safely in the closure of the pelvic cavity after abdominoperineal resection,32 in the closure of the rectal wall after transanal endoscopic microsurgery,33 as well as in the closure of enterocolotomy after right hemicolectomy. Among these latest publications, both Feroci et al.34 and Bracale et al.35, in their respective studies, defend the technique as safe and effective, although both presented a small number of subjects (47 and 40 patients, respectively).
Our team uses a double-layer closure (Quills®, Anglotech, Reading, PA, USA), as described by Reggio et al.36 in their study comparing double versus single-layer sutures, finding different differences in favor of the former (lower percentage of anastomotic leakage). In the literature,20 the percentage of leaks after this surgery ranges between 0% and 8.5%. Our data show a low percentage that is within the range reflected in the literature (2.5%). In addition, in our series neither of the 2 dehiscences was related to the barbed suture: one occurred in the stump of the small intestine due to necrosis and another due to dehiscence on the posterior side of the mechanical anastomosis. In terms of the rest of the complications, our results (25% overall) are within the range shown in the literature.4,6,17
Possibly, the most technically challenging skill in laparoscopy is the performance of intracorporeal sutures and anastomoses (advanced laparoscopy). With the advent of barbed suture, these difficulties can be overcome, as they avoid the need to perform intracorporeal knots or the need for the surgical assistant to maintain tension in the continuous suture. This clearly improves key surgical aspects, such as reproducibility and operative time. The use of barbed suture in the right hemicolectomy with intracorporeal anastomosis seems to present a morbidity rate that is similar to series described in the literature. In any event, prospective, controlled, randomized studies with more patients are needed to confirm these findings.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ferrer-Márquez M, Torres-Fernández R, Rubio-Gil F, Belda-Lozano R, Moya-Forcén P, Benavides Buleje JÁ, et al. Uso de la sutura barbada para el cierre de la enterocolotomía tras hemicolectomía derecha con anastomosis intracorpórea. Estudio prospectivo descriptivo. Cir Esp. 2020;98:136–142.