Pelvic arteriovenous malformations (AVM) are a rare condition that pose a diagnostic and therapeutic challenge for medical professionals. They can affect any age group or either sex, and, in terms of clinical symptoms, they can be symptomatic or asymptomatic processes. The most frequent clinical manifestations are palpable mass or local pain caused by compression.1 Diagnosis is made using various imaging studies, treatment is complex, and the recurrence rate is high.2
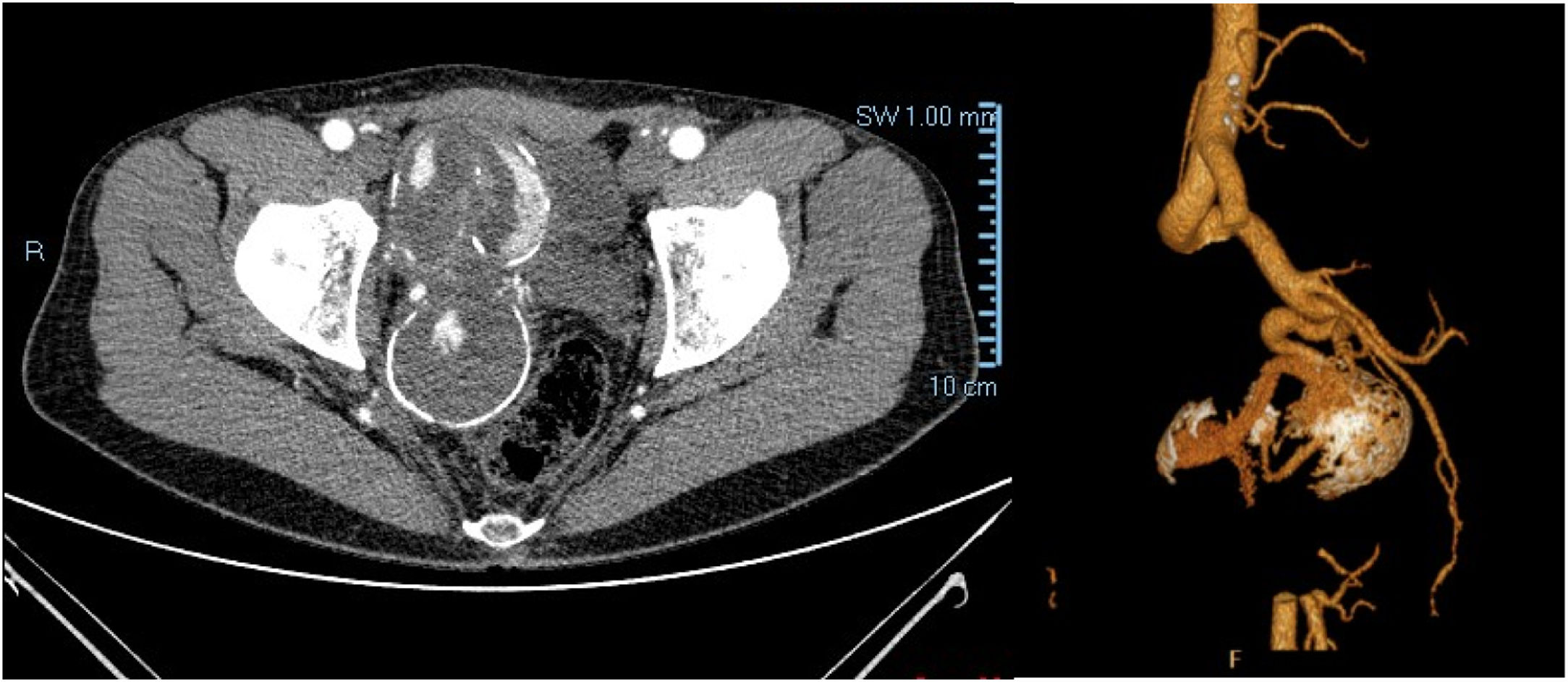
We present the case of a 47-year-old man, with no relevant medical or surgical history except for a hiatal hernia with occasional esophageal spasms. He went to his primary care physician for symptoms of sciatic pain radiating to the right leg and perineal region, accompanied by paresthesia that had been progressing for weeks, with no previous trauma. Spine radiography showed increased density in the bladder region. Lumbosacral MRI revealed minimal lumbar disc degeneration and a rounded lesion adjacent to the right psoas muscle, possibly renal in origin, along with lobulated masses in the pelvic area. Given these findings and the clinical suspicion of a bladder tumor, the patient was referred to the urology unit. In the specialized consultation, abdominal ultrasound detected a right paravesical polylobulated mass that was vascularized and partially calcified, although the etiology could not be determined. Given these findings, a pelvic MRI was ordered, which identified a large highly vascular tubular lesion measuring 13.3 × 12.2 × 6.1 cm (craniocaudal, anteroposterior and transverse, respectively) that was displacing the bladder, prostate, seminal vesicles and the anorectal area. Dilation of adjacent venous structures was also reported. The patient was referred to the vascular surgery consultation for evaluation. The physical examination of the patient was normal, with pulses present at all levels and no pulsatile abdominal mass. CT angiography with contrast revealed a fusiform aneurysmal dilatation measuring 54 × 53.2 × 74.8 mm (craniocaudal, transverse, anteroposterior) that began in the right internal iliac artery and extended towards the pelvis (Fig. 1). Given the suspected diagnosis of right hypogastric aneurysm, arteriography was ordered, which revealed a high-flow AVM with arterial flow from the bladder arteries and venous drainage through the pudendal veins to the internal iliac vein. The venous drainage presented 2 stenoses (Fig. 2).
We decided to conduct endoluminal surgery for embolization of the AVM after selective catheterization of the right hypogastric artery, right femoral vessel and contralateral femoral vein. In the first injection of diagnostic contrast, a large decrease in the size of the nidus was observed, with almost complete thrombosis; therefore, a 5 × 20 Concerto® coil was placed in the afferent artery and Onyx in the residual area. In the final examination, excellent morphological control was observed with thrombosis of the nidus.
The patient was discharged 24 h after surgery, with no local or procedural complications. One month later, he came to the outpatient clinic for follow-up and was asymptomatic; the symptoms that originated the initial consultation had disappeared. Follow-up CT angiography showed no AVM filling with thrombosis and calcification.
Congenital pelvic AVM are rare entities. A limited number of cases have been described in the literature, which makes it difficult to standardize their diagnosis and management. They are defined as abnormal communications between arterial and venous channels with no interposition of the capillary system.1
They mainly affect young adults, without a predominance of either sex, and their spontaneous appearance has been mainly related to traumatic events and/or urological procedures.1,2
They are usually asymptomatic, and therefore go unnoticed. In symptomatic cases, the clinical manifestations are variable: pain, palpable mass, hematuria, arterial hypertension or compression symptoms. The diagnosis is made using imaging studies, such as Doppler ultrasound, MRI, CT angiography, or digital subtraction angiography.1,3
The treatment of this pathological process is complex and presents high surgical morbidity and mortality rates, regardless of the treatment chosen.4,5 In addition, patients should be followed long-term, as the lesions may recur. Recurrence rates are highly variable in the series published, ranging from 8% to 93%.6 AVM in the abdominopelvic cavity can be treated with a combination of sclerotherapy and open surgical resection. Currently, the most standardized treatment is endovascular surgery with embolization or mixed percutaneous-endovascular vascular approaches combined with open surgery.7
Spontaneous thrombosis of the AVM is a phenomenon that is usually associated with morphology, occlusion of the draining vein, and type of flow.5,8,9 The presence of calcifications is related to cortical thickening and the chronicity of the old thrombus, which are more typical of low-flow AVM.9 In our case, we believe that the presence of 2 stenoses in the drainage vein was a decisive factor for its partial thrombosis.
Please cite this article as: Doiz Artázcoz E, Manosalbas Rubio IM, González Calbo A, Martín Cañuelo JJ, Rodríguez Piñero M. Malformación arteriovenosa pélvica sintomática tratada con éxito mediante abordaje endovascular. Cir Esp. 2020;98:493–495.